Management of a tooth with primary periodontal lesion with AF F One
26/10/2023
Francesca Cerutti
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The interrelationship between periodontal and endodontic disease has always aroused confusion, since differentiating between a periodontal and an endodontic problem can be difficult. In some cases, the influence of pulpal pathology may cause the periodontal involvement and vice versa.
The periodontal-endodontic lesions have been characterized by the involvement of the pulp and periodontal disease in the same tooth. This makes it difficult to diagnose because a single lesion may present signs of both endodontic and periodontal involvement. The vast majority of lesions are the result of bacterial infection, thus one disease may be the result or cause of the other or even originated from two different and independent processes which are associated with their advancement. Diagnosis is complicated by the fact that these diseases are too frequently viewed as independent entities. However, it is critical to recognize the interrelationship for successful management of these lesions. The pathways for the spread of bacteria between pulpal and periodontal tissues are still a subject of controversy.
We talk about Primary Periodontal Lesion when the periodontal disease has gradually spread along the root surface towards the apex. The pulp may remain vital but may show some degenerative changes over time. In such cases, it is advisable to treat the periodontal tissues only.
Lindhe and Adriaens reported that bacteria coming from the periodontal pockets can reach the pulp, suggesting that the dentinal tubules may serve as a reservoir for these microorganisms and that a recolonization of the treated root surface may occur. moreover, the root planning and scaling may result in the rupture of the vessels and destruction of the neurovascular bundle in the lateral canals, provoking a reduction of the blood supply and consequently leading to pulp alterations.
Knowledge of these disease processes is essential in coming to the correct diagnosis. This is achieved by careful history taking, examination, and performing special tests.

Fig. 1
A 40 years old patient was referred to me by a periodontolgist who had diagnosed a primary periodontal lesion, with a deep probing on the palatal and distal aspect of tooth 2.7
The tooth was symptomatic and positively responding to pulp sensibility tests.
The request of the period ontologist was to do the endodontic treatment before the periodontal intervention, since the lesion was involving the apex of the root and some sign of pulp degeneration were present.
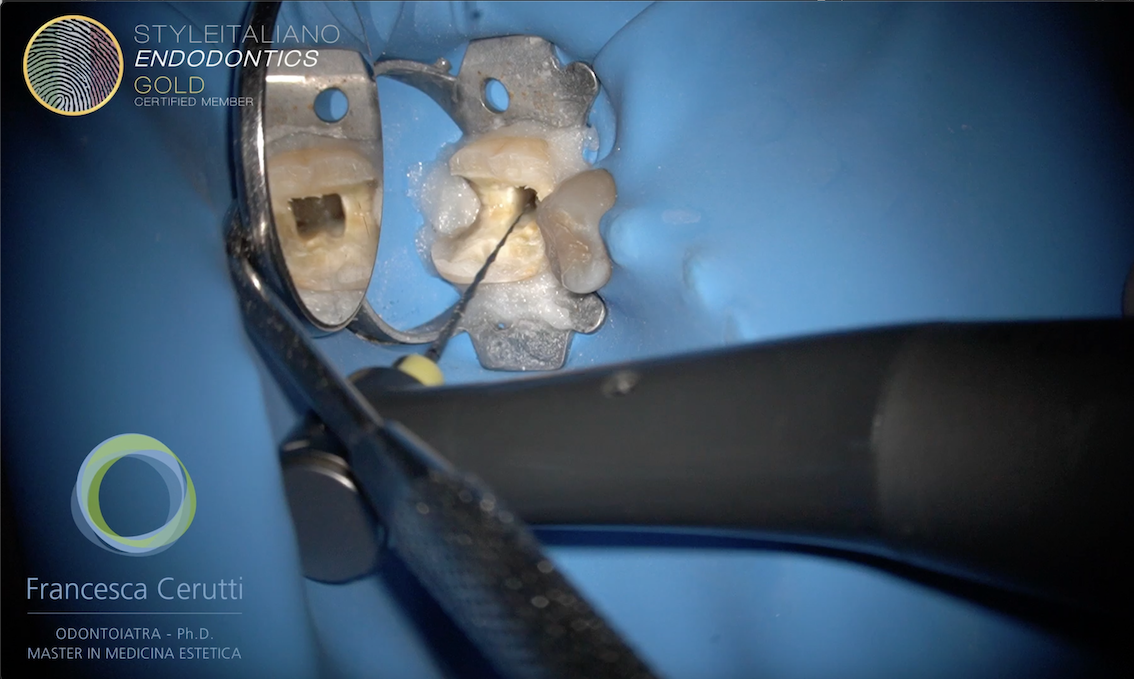
The tooth was isolated with rubber dam. The existing onlay was considered good, so the access cavity was done through the restoration.
A diamod coated tapered bur was used, followed by an ultrasonic tip.
The pulp was in an inflamed state, with profuse bleeding.
Once the three main canals were visible, a full mechanical pre flaring was done with Fanta AF-F One 13/.03, 20/.04, 25/.06.
The rotary file was inserted into the root canals without applying any pressure, 5 mm short from the estimated working length
Appearance of the tooth after preflaring
After recording the working length and establishing a glide path, the canals were shaped to the working length by Fanta Af-F One Style Italiano Endodontics selection
The visual gauging helped to determine the final size of the apical preparation
The root canals were irrigated with NaOCl, acitvated by US tips, then rinsed with sterile water and irrigated again with EDTa, also activated by US tips. In the end the canal was rinsed with sterile water.

Fig. 2
Intra operative x-ray with cone fit
The tooth was obturated with single cone + tricalcium silicate based sealer

Fig. 3
The access cavity was restored in the same appointment

Fig. 4
The symptoms of the patient disappeared within 24 hours; the week after the endodontic treatment she received the periodontal nonsurgical treatment.
Conclusions
A correct diagnosis and a multidisciplinary approach are the key to approach correctly endo-perio lesions.
The use of strict protocols is mandatory to achieve a successful outcome.
Bibliography
Didilescu AC, Rusu D, Anghel A, Nica L, Iliescu A, Greabu M, et al. Investigation of six selected bacterial species in endo-periodontal lesions. Int Endod J. 2012;45(3):282-93.
Gandhi A, Kathuria A, Gandhi T. Endodontic-periodontal management of two rooted maxillary lateral incisor associated with complex radicular lingual groove by using spiral computed tomography as a diagnostic aid: a case report. Int Endod J. 2011;44(6):574-82.
Oktawati S, Siswanto H, Mardiana A, Neormansyah I, Basir I. Endodontic–periodontic lesion management: A systematic review. Medicina Clínica Práctica. 2020;3.
1. Rotstein I, Simon JHS. The endo-perio lesion: a critical appraisal of the disease condition. Endo Topics. 2006;13:34–56.