Dental Adhesives: a 10 years story
30/03/2022
The Community
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
An article by dr. Salvatore Sauro
Overview and basic commentary
Before any discussion about adhesion to crown and root dentine, it is imperative to state that there is no substantial scientific research evidence-base that can support a specific bonding approach rather than another.
Said that, there are several in vitro studies showing that multi-step bonding systems bonded to dentine can have a longer lasting durability compared to simplified one-bottle systems, in particular with those applied through an etch-and-rinse approach. Nowadays, only two main categories of bonding systems are available for clinical applications; etch-and-rinse adhesives (ERAs) and self-etching adhesives (SEAs). The latest adhesives are known as “universal” adhesives that combine etchant, primer, and adhesive in a single solution which can be used both with phosphoric acid etching pre-treatment or as a self-etching adhesive.
However, despite the progress in the formulation of dental adhesive systems over the last ten years, shortcomings such as post-operative sensitivity, premature reductions in bond strength, interface and marginal degradation, and biocompatibility are still considered important issues with such materials. Enzymatic degradation of collagen fibrils within the hybrid layer and hydrolysis of polymers are the major factors thought to destabilise the resin-dentine interface. It is also important to consider that glass ionomer materials can be considered as self-adhesive, which can be used in alternative to conventional adhesive-composite restoration or as dentine substitute materials; these materials are less affected by conventional degradation events commonly occurring at the resin-dentine interface (i.e. hybrid layer) created using adhesive systems. Nevertheless, the use of glass-ionomer-cement as dentine substitute material in resin composite restoration does not have any effect on the survival of resin-composite restorations; after 18-years there was no clinical difference in the survival rate between resin-composite restoration performed with or without an intermediate layer of glass ionomer cement. However, it would be interesting to see the results of future clinical studies if the use of air-abrasion performed with bioactive glass before bonding procedures may reduce the influence of secondary caries and improve the clinical longevity of composite restoration performed with or without an intermediate layer of glass ionomer cement
Pathways for the degradation of the bonding interfaces
The longevity of dentine adhesive restorations still remains a challenge as bonding failures lead to recurrent caries (e.g. secondary caries), and represent the main reason for replacement of direct restorations [1,2]. Indeed, more than 50% of restorations being replaced have been reported to be caused by formation of secondary caries [1,3,4]. The longevity of amalgam is over 20 years, while adhesive/composite restorations are estimated to endure in the patients’ mouth less than 7 years; the failure rate of posterior resin composite restorations after 7 years can be 50% greater than that of high-copper content amalgams [5, 6]. Regarding the restoration of endodontically-treated teeth, It is challenging to evaluate the survival rate since it is influenced by a huge number of variables such as residual volume of structure in prepared teeth, the presence of proximal contact-points, location of the teeth, cuspal coverage restoration in molar teeth and the employment of a post. However, it has been reported that teeth restored with fibre posts have comparable survival rates to those restored with direct or indirect metal posts [7]. Moreover, direct composite restorations in root-filled premolars with Class II cavities performed as well as teeth restored with single unit crowns [8]
The issue about the longevity of the adhesive interface of composite restorations is related to two main mechanisms which have been identified to contribute to resin-dentine hybrid layer degradation: i) Intrinsic or proteolytic degradation of the organic matrix; ii) Extrinsic or hydrolytic degradation of the resin matrix. Both mechanisms are interlinked and occur simultaneously, decreasing the durability of resin-dentine bonds. [9-11]. However, it is important to state that the choice of the material to being used for bonding and restoration represent only one of several factors (patient compliance, complexity of the clinical case, medical history of the patients and so on…) that may influence the longevity and survival of the treatment; the most important factor remains the ability and the skills of the clinician [2].
Guide through bonding systems currently used in dentistry – Pros & Contras
Adhesives are generally categorised into "generations" in order to outline the different components (e.g. etchant, primer, and adhesive) of all classes of products. Nevertheless, the use of such a classification cannot be universally accepted. Indeed, a great number of adhesive have been lunched on the market so this type of classification has become rather inept and confusing [9]. Contemporary adhesives are classified based on their mode of interaction with dental hard tissues as either etch-and-rinse adhesives (ERAs) or self-etch adhesives (SEAs) [10, 11]. ERAs require the use of a 32-40% phosphoric acid etching to remove the smear layer and demineralised dentine and enamel to create micro-retentions. This is then rinsed, followed by the application of a resin primer, and adhesive (three-step systems) or by a single-bottle self-priming agent (two-step systems). On the other hand, self-etching do not require and pre-etching with phosphoric acid in dentine, but the acidic components (e.g. 10-methacryloxydecyl-dihydrogen-phosphate (10-MDP)) of the adhesive can partially remove the smear layer and expose a very thin layer of demineralised collagen. [9, 11]. Subsequently the primed dentine does not need to be not rinsed and the solvents in the primered-dentine is evaporated with air for approx. 5s, and it is then covered with an adhesive and light-cured (two-step systems). The one-bottle or all-in-one systems are single bottle adhesives that contains functional acidic-methacrylates (e.g. MDP) for etching purpose and cross-linking dimethacrylates for polymerisation. In this latter category we can include the “universal” adhesives that combine etchant, primer, and adhesive in a single solution which can be used both with phosphoric acid etching pre-treatment or as a self-etching adhesive [12].
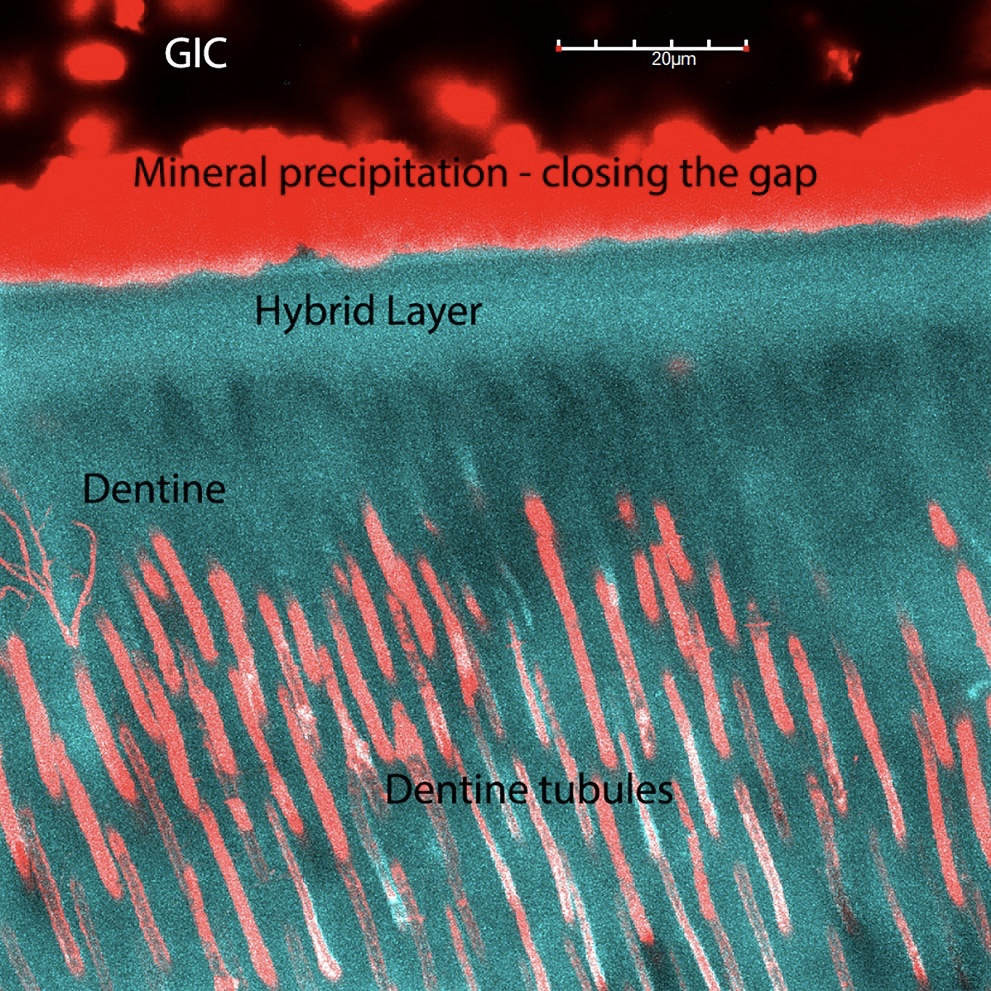
The bonding performance at short-time period (24hr) of most adhesive currently in use is outstanding, but in vitro studies have shown that the main drawback of “simplified” systems (including modern universal adhesives), is their poor durability over a period superior of 3 months of storage in water, especially for those applied in ER mode [13]. Indeed, an proper penetration of adhesive monomers into the etched dentine is a key requirement to accomplish the formation of a “high quality” and long lasting hybrid layer [14,15]. Unfortunately, simplified adhesive, including the modern universal adhesives, when applied in ER mode cannot penetrate into acid-etched dentine due to the excess of water within the demineralised collagen fibrils [16-18] (Figure 1).
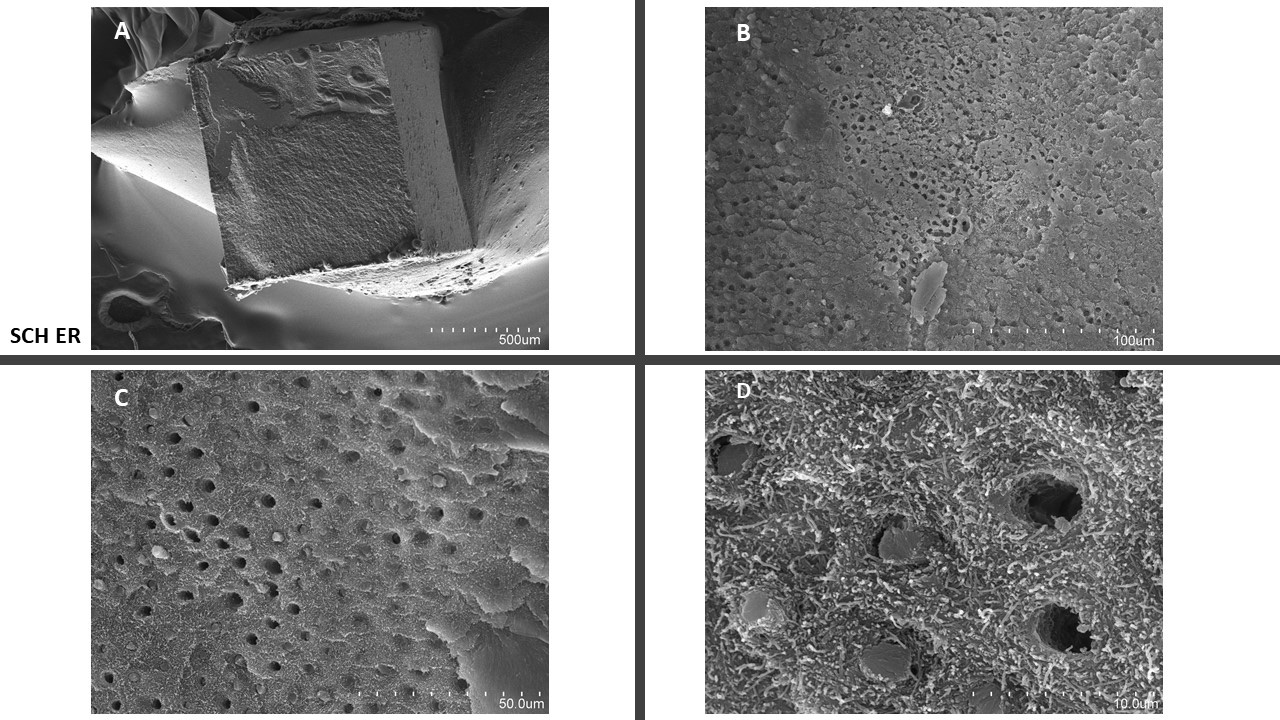
Figure 1: Scotchbond universal applied in ER mode. It is possible to see a mixed failure (A) and when observing at higher magnifications (B, C, D) on the zone with adhesive failure, it is possible to see zones characterised by several exposed collagen fibrils due to a great lack of resin infiltration .
Such residual water may culminate in nanoleakage within the hybrid layer and nano-phase separation of the adhesive monomers between the polymerised resin; this increases uptake water and jeopardise the mechanical properties of the resin-dentine interface [19-21]. Moreover, It has been demonstrated that the presence of active metalloproteinases such as MMP-2 and MMP-9 and cathepsins within poorly infiltrated hybrid layers plays a crucial play a role in the destruction of the dentine collagen so contributing significantly to the reduction of the durability of the bonding interface [22,23]. Conversely, although self-etching adhesives can also activate such proteolytic enzymes [24], but there is a general consensus that collagen degradation occurs more in ERAs; phosphoric acid etchants demineralise dentine more deeply and more completely, leaving collagen fibrils exposed, and making them more susceptible to proteolytic degradation by the endogenous dentinal enzymes [15, 25]. Indeed when employing milder self-etching adhesives (SEAs) or glass ionomer cements (GICs), the degradation processes at the bonding interface are extremely less compared to etch-and-rinse adhesive. This is mainly due to the fact that milder acidic SEAs and GICs do not totally expose the collagen fibrils and leaves small smear plugs within the dentinal tubules [26-28]. Moreover, it is also noteworthy that the dentine demineralisation when using SEAs or GICs is very superficial (less than 1-2 microns) [9] and therefore the resin-infiltration of SEAs and GICs can occur quite easily, so creating an hybrid layer less porous compared to that created with ERAs [28].
As earlier said, contemporary bonding systems can be categorised as: “etch-and-rinse adhesives” (ERAs), “self-etch adhesives” (SEAs) or “glass ionomer-based materials” (GICs). This latter class of materials include classic GICs and RMGICs that can be also used for bonding purpose [11, 29, 30]. The main difference between these systems is their degree of “acidic-invasiveness”. Commonly, ERAs systems cause substantial alteration of the dentine due to the use of phosphoric acid, which exceeds that of SEAs and conventional GIC or resin-modified glass ionomer cements (RMGIC); these latter interact with the dental hard tissues modifying the smear layer and only partially exposing collagen fibrils [9,23].
The GIC/RMGIC systems are classified as proper self-adhesive materials; that can bond to dentine micromechanically, through infiltration of the collagen network previously exposed by conditioning the dentine using 10% polyacrylic acid (PAA), in combination with chemical bonding obtained by ionic interaction of carboxyl groups from the acid with calcium ions of remaining crystals of hydroxyapatite (HAP) [11, 29]. Furthermore, glass ionomers are biocompatible materials that release specific ions such as fluoride that can have antibacterial [32, 33] and remineralising properties at the bonding interface [9, 11, 34]. They also have thermal expansion coefficients that match that of dentine and clinically, RMGICs result much more resistant rather than GIC to the tough conditions in the oral cavity such as low pH and thermal stress [35]. Indeed, it was shown that such materials may create durable bond strength after several years of water storage without any drastic loss of micro-mechanical and chemical bonding at the dentine [36, 37]. Moreover, it has been also demonstrated the bond stability after 1 year aging of conventional glass ionomer cements applied to dentine, with or without dentine pre-treatment using a polyalkenoic acid [38].
To conclude, it is important to highlight the possibility to keep etching the enamel (selective etching) even if a SEA or an universal adhesive is employed during the restorative procedures. However, Sato et al. [39] stated that although selective phosphoric acid etching could create a stable adhesive-enamel interface, the bond strength remains dependent on the type of material utilised.
Thus, to the question “what bonding strategy should I use when I restore a cavity after root-canal treatment?” it is possible to affirm that in view of all the studies considered so far, the use of multi-step SEA or ERA system seem to remain the best option to achieve a long-lasting bonding stability. However, in case of employing an universal bonding system, it would be recommendable to use it in self-etching mode associated with a selective-etching approach in enamel. However, it is important to bear in mind that one of the most “robust” (in terms of bonding longevity) approach is represented by the use of materials based on glass ionomer cements, therefore it should not be excluded the use of such dentine replacement materials without any previous application of adhesive system in dentine.
What restorative material should be used for direct restoration of endodontically treated teeth?
As previously stated at the beginning of this study, there is no substantial scientific research evidence-base that can support a specific bonding restorative approach rather than another in terms of survival. Moreover, the restoration of endodontically-treated teeth is influenced by a huge number of variables so it is quite challenging to evaluate the survival rate of different restorative approach to state which one is the most appropriate; a standardisation in this situation does not exist, especially in the case of direct restorations. Moreover, it is important to recall that teeth restored with fibre posts have comparable survival rates to those restored with direct or indirect metal posts [7] and that direct composite restorations in root-filled premolars with Class II cavities performed as well as teeth restored with single unit crowns [8]. It has been also demonstrated that the use of a glass-ionomer-cement as base prior composite restoration has no negative affect on their survival rate. Indeed, acceptable annual failure rates could be achieved after 18 years when placing an intermediate layer of GIC with no significant difference compared to conventional composite restorations; thus no improvement in survival should be expected based on such a clinical restorative approach [40].
Said that, direct restorations are frequently undertaken using conventional resin composites due to their excellent mechanical and aesthetic properties [41, 42]. Nevertheless, light -curing resin-based materials remain characterised by important drawbacks associated to their polymerisation shrinkage, which can provoke stress at resin–dentine interfaces and jeopardize the overall longevity of the restoration [43–45]. Indeed, the volumetric contraction of conventional resin composites can cause debonding of some adhesive systems [43, 46, 47]. Accordingly, the sealing between composite and dentine can be seriously compromised with the formation of gaps and marginal leakage; pathways for microleakage of oral fluids, bacteria, and enzymes penetration [43, 48–50]. Such a scenario results in important clinical issues such as marginal discoloration, secondary caries, pulp and root-canal retreatment in endodontically-treated teeth [51, 52].
However, there are several clinical strategies that may reduce the stress concentration at the resin–dentine interface during polymerization and possibly increase the longevity of the resin-dentine interface [53]. For instance, flowable composites or glass-ionomer cements (GIC/RMGIC) used as base/liner or dentine-substitute materials may represent a proper method to provide a sort of “stress-absorption” [54,55]; they may prevent stress development at the dentine-bonded interface and reduce the risk for gap formation, microleakage, so promoting secondary caries formation [53,56,57]. Moreover, It is also important to consider that occlusal stress during mastication, swallowing, as well as in cases of parafunctional habits, can exuberate such issue since they can jeopardise the integrity of the bonding interface, making such a structure more susceptible to degradation over time [58, 59].
Further efforts to diminish the effect of the shrinkage stress of composites have been proposed, such as the incremental filling techniques.[60, 61] indeed, several studies have demonstrated that such procedural approaches may reduce cuspal deflection, incidence of enamel cracks or fractures, premature gap and formation at the resin–dentin interface. [60, 62, 63] The rationale of the incremental technique is to avoid the application of composite that can join the opposite walls of the cavity with a large volume of composite. Conversely, shrinkage stress is minimised when there are fewer bonded prepared walls involved during the polymerisation, thus reducing the C-factor. In addition, by incrementally curing either 2-mm thick increments, a higher degree of conversion is expected due to lower light attenuation. [62, 64]
However, there is a growing interest in bulk-fill composites , which have been designed to replace the need for incremental layering, providing simple and fast clinical procedures. This new category of composites is intended to be applied as a single incremental application of 4 to 6 mm thick layer. This simplified strategy is said to be attributed to increased composite translucency, allowing greater light transmission with depth, and to the addition of more reactive photo-initiators. [65, 66] In addition, these materials are claimed to have low shrinkage stress due to inclusion of proprietary stress reliever molecules and polymerisation modulators [65, 67], but unfortunately there are yet too little scientific support for these latter observation, so it is suggested to use an incremental layer technique (up to 2 mm thickness) even when using a bulk-fill resin-composite system (figure 2).
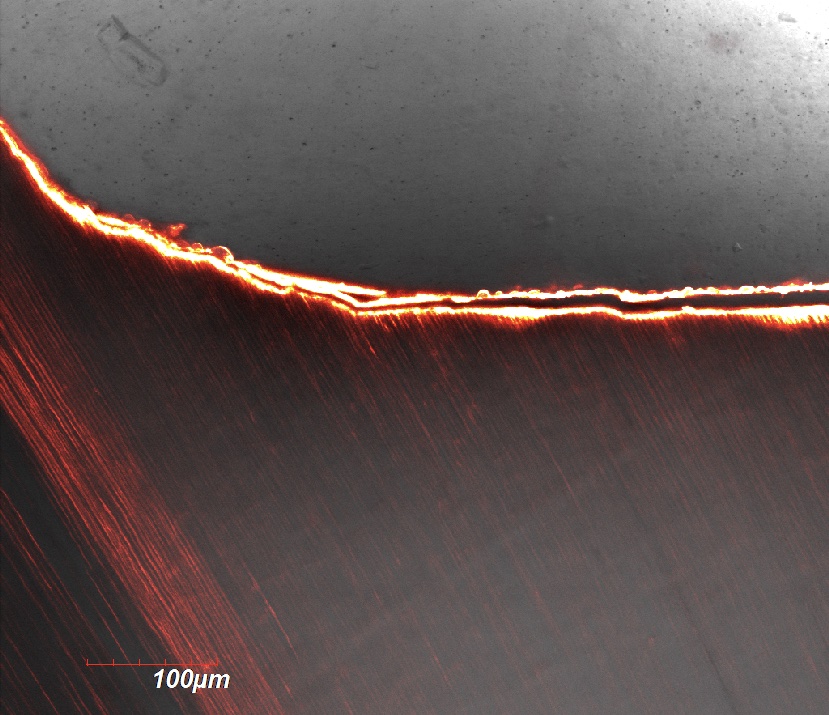
Figure 2: Confocal image of a resin-dentine interface created with the application of a bulk-fill composite. It is possible to see the presence of important gaps probably due to shrinkage of the material during light-curing procedure
In conclusion, to the question “What restorative material should be used for direct restoration of endodontically treated teeth?” it is possible to answer that in view of all the studies considered so far we can only suggest to use materials with lower modulus of elasticity such as flow composite applied as liner/base at the access of the canals to reduce the stress of the polymerisation of the conventional composite that will be subsequently used to restore the cavity. In case of using bulk-fill sculptable or flow composites, our suggestion is to apply it layer by layer not thicker than 2 mm and light-cure each one of it separately for 20-30 sec. Moreover, the use of GIC-based materials as base or dentine-replacement material, followed by adhesive/composite restoration would be a further option, especially in those cases where the volume of restoration with one or more walls lost during caries excavation and cavity preparation.
Is there any potential benefit in using air-abrasion before adhesive restoration of endodontically-treated teeth?
Originally, air-abrasion (AB) was proposed as an alternative method to handpiece for cavity preparation, but subsequently it was also advocated for minimally invasive cavity preparation and/or caries removal or for decontamination of the dental substrates before adhesive restorations [68,69]. AB can be considered a kinetic method, which uses a stream of abrasive particles to gently remove dentine and/or enamel via an end-cutting process [70-72]. It has been reportedd to generate a smooth cavity with blurry walls and margins along the cavity [68]. Moreover, it generates no vibrational stress on tooths tructures, so resulting in low disconfort for patients durign air-abrasion procedures [73, 74]. The most common abrasive powder in AB is Alumina (aluminium oxide) [69,75] and recently there has been the introducion of bioactive glass powders, as an alternative abrasive/polishing powder [72, 76].
A recent study has shown that dentine prepared with alumina or other bioactive glass powders was characterised by the presence of smoother dentine walls and indistinct margins compared to the those prepared with burs [76]. It was also shown [68] that the most relevant morphological feature of a cavity prepared through AD is a contour with rounded shape and indistinct walls and margins [77]. Cavities with rounded internal line angles may have less C-factor with consequent a lesser amount of stress concentration along the bonding interface [68, 78]. Conversely, an evident surface roughness characterise the cavities prepared with conventional burs. In this latter situation, when such cavities are restored using conventional resin composites, fatigue failure may happen subsequent to masticatory stress, particularly if the degree of the stress at the interface is sufficient to initiatiate crack propagation [79, 80].
As previously stated, new bioactive powders have been formulated to being used in air-polishing/cutting procedures as an alternative to alumina [72, 76]. It was demostrated that dentine air-abrasion performed using bioactive glasse (BAG) van criate a “bio-reative”smear layer [9], which can remain available at the interface when restoations are perfoemd glass-ionomer cements or SE adhesives; their biactivity can contribute to the reduction of the degradation processes that occur at the bonding interface over time [81,82]. Indeed, a recent study showed that air-abrasion performed with alumina has no negative effect on the immediate bonding performance of SE adhesives, but the bonding longevity may be jepardise due to degradation procecess at the bonding interface over time [21]. Conversely, the presence of BAG at the interface may protect the hybrid layer thanks to the hydrated silica Si(OH)4 produced such a biaoctive substance once in gets in contact with water, saliva, blood [83]. Subsquenlty, this latter may serve as template for mineral precipitation (e.g. Ca and PO) which then maturates into apatite [84, 85]. Such a remineralisation process may reduce the proteolytic degradation caused by MMPs [86-88]. Moreover, BAG have an antibacterial effect that may be attributed to the release of specific ions (e.g., fluoride, zinc calcium and phosphate), that have a toxic effect on the cells and cause neutralization of the local acidic environment [89], due to a local increase in pH that is not well tolerated by many oral bacteria [90].
However, the hypotesis that may justify the use of bioglass before retorations of endodontically treated-teeth is based on the posibility of such biactive materials to repair gaps via apatite remineralisation at the interface, so avoiding bacterial leakage and reinfection of the root-canal system, with a consequent need for endodontic retreatment. Indeed, a recent study showed that a resin-based material doped with BAG, was able to reduce significantly the extent of bacterial biofilm penetration into preexisting marginal gaps. Moreover, the release of BAG ions into the gap can help control the local gap chemistry and create an antimicrobial environment that slows biofilm development and propagation [91].
It is important to bear in mind that the presence of gaps may facilitate accumulation of biofilm within the restoration-tooth margins [92, 93]. Moreover, cyclic loading due to mastication is a known potential cause of margin failure and gap propagation [94, 95]. On the other hand, polymerization shrinkage of resin composites during light-curing procedure may cause stresses on the interface that increase the chance of interfacial failure [93]. In other words, gaps at the restoration-tooth interface seem to be inevitable, and that represent a real and constant risk factor that may jeopardise the longevity of our restorations
Thus, to the question “Is there any potential benefit in using air-abrasion before adhesive restoration of endodontically-treated teeth?” it is possible to answer that in view of all the studies considered so far, the use of air-abrasion with alumina or BAGs before restoration may create a bonding substrate smooth and a cavity with rounded walls that can help in reducing the effect of polymerisation shrinkage of composite. However, Alumina seems to have no effect on the longevity of the bonding interface, while BAGs, can offer some possible benefits in terms of antibacterial effects and remineralisation/repair of the gaps at the bonding interface.
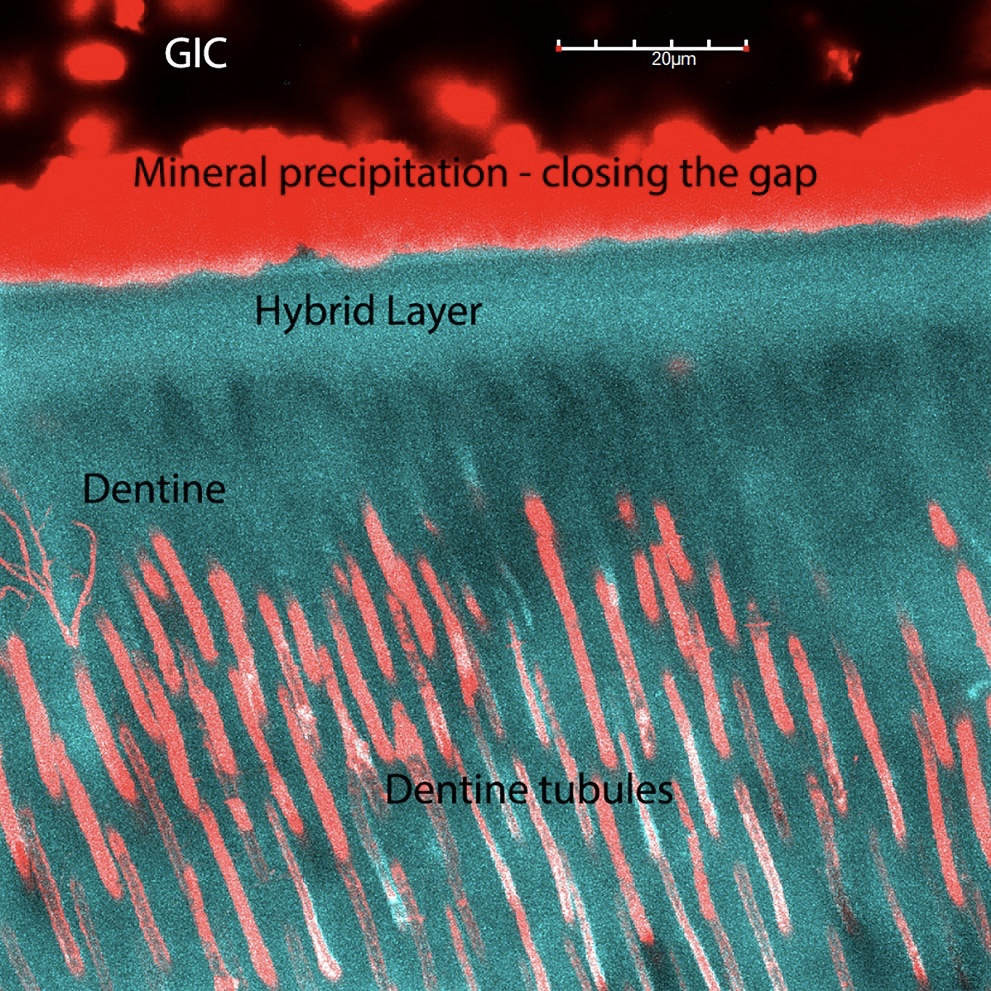
Figure 3: Confocal image of a bonding interface created with the application of a resin modified glass ionomer cement (GIC, Riva LC, SDI, Australia) on dentine air-abraded with SELECTA Kinetic, a polycarboxy-lated zinc-doped bioglass created by Velopex International, Harlesden, London, UK. It is possible to see the presence of minerals precipitation at the bonding interface that closed the gaps probably due to shrinkage of the material during light-curing procedure
The use of root canal posts in endodontically-treated teeth
Anterior teeth, premolars and molars are subjected to a different biomechanical stress in terms of load direction. For instance, maxillary anterior teeth are typically exposed to high shear stress, so making this area potentially at a higher risk of failure compared to posterior teeth [96]. This is the main reason why it is believed that posts should be used in this area; unfortunately, there is not much scientific evidence to support such an assumption [7]. Indeed, adhesive-luted root canal posts seem to offer very little reinforcement to the endodontically treated teeth [97, 98), but they may increase the anchorage of core build-ups and coronal restorations [99, 100]. However, the determination of when to use a post essentially depends on the coronal hard tissue loss, as well as the type of tooth and the restoration that will be performed; these are more normally used for indirect restorations rather than direct restorations [101]. The existing literature does not indicate any exact level of structure loss at which a post contributes to the survival of a root-canal treated teeth [7]. The clinical evidence for a positive effect of using post remains scarce and controversial. For instance, it was demonstrated that only a significant positive effect on survival rate of post used in teeth with no remaining dentinal walls [102]. Moreover, two further studies showed after 17 years no difference in outcome for post-retained and post-free restorations, both in indirect [103] and direct restorations [104]. Mannocci et al. [105] demonstrated that premolars with Class II cavities treated endodontically presented no difference in survival rate when restored using carbon fibre posts and direct composite or an amalgam Nayyar core.
It is also important to consider the type and the material that the posts are made of. For several years, metal-based posts such as gold alloy or cobalt-chromium-based cast posts and cores have been employed in clinic to restore endodontically-treated teeth, with a high success rate > 84% at 10 years [106, 107]. However, the main disadvantage of such posts is related to the amount of dental substrate that must be removed for the preparation of an adequate post space, along with the risk of coronal leakage during temporary restoration. Nowadays, clinicians have the possibility to decide between rigid post materials such as titanium, stainless steel, gold alloys, zirconia or elastic ones like carbon, glass or quartz fibres. In particular, posts based on glass and quartz fibre are typically embedded in an epoxy or methacrylate resin to achieve a level of aesthetic superior to that of metal-based or carbon fibre ones.
It has been advocated that post should form a monoblock with the root-dentine when applied using adhesive luting procedures [108], so that the similar modulus of elasticity of the different compartments (e.g. post, luting cement and dentine) may favour the distribution of stress more uniformly so reducing the incidence of fractures of roots compared to posts made of more rigid materials [109].
Unfortunately, there is scarce clinical evidence to support that the use of fibre posts will result in less incidence of fractures [110, 111]; prospective clinical also demonstrated the both rigid and flexible posts have no benefit on tooth survival and restoration success [107, 112]. Again, the main factors that influence the long-term survival of root-canal treated teeth is the amount of remaining coronal tooth substance; excessive removal of root dentine structure during post space preparations should be avoided [113, 114]. Recently, customized fibre bundles that can be adhesively adapted to irregular root canals even without post space preparation have been developed in order to avoid unnecessary dentine removal, but the evidence on the survival of teeth restored with such technique is scarce and inconsistent [115; 107].
Adhesion and luting of posts to root canal dentine
Some specific bonding issues related to imperfect polymerisation, inadequate adhesive application, along with incomplete and/or shrinkage of resin-based luting agents, are the main reasons why teeth restored with root canal posts commonly fail in clinical [116]. Root canal post can be luted using self-adhesive resin cements (SACs) or through the use of etch-and-rinse and self-etch adhesives. However, adhesive procedures inside the root canal results quite difficult because of restricted access and visibility in root canals [117]. Moreover, issues related to the high C-factor [108, 118] and those related poor light transmission through fibre posts during light-curing procedures [2019] should not be undervalued. Conversely, the use of dual-curing systems seems to guarantee a better level of proper polymerization with lower shrinkage, especially when materials based on glass ionomer cements are employed [212]. These latter cements are well known to undertake a dynamic ionic exchange with the surrounding microenvironment for a relatively long time [34, 120] and to create a stable chemical bonding to dental tissues [11, 9, 121]. Moreover, as previously described, the use of bioglass in air-abrasion system before followed by GIC restoration may protect the bonding interface and repair it in case of gaps via apatite remineralisation, so avoiding bacterial leakage and reinfection of the root-canal system [57, 91]. A recent randomized controlled clinical trial showed greater debonding after six years in conventional resin cements applied using an etch-and-rinse adhesive compared to SAC cements [122].
It is important to consider that during the preparation of the post space preparation inside the canal a specific smear layer is created and it is usually thicker than the smear layer created during endodontic procedures; it consists of dental debris and residues of gutta-percha as well as sealer particles [123]. This is the reason why it is often recommended the use of phosphoric acid to remove the smear layer; this latter can impair the bonding longevity of adhesive systems in root canal dentine due to enzymatic and hydrolytic degradation [87, 124]. Again, the use of air-abrasion may contribute in the decontamination of such a particular dentine substrate, as well as replacing that thick smear layer with a more “adhesive-friendly” smear layer, or with a bioactive one when bioglasses are used as abrasive powders [9, 76]
Application of adhesives and luting cements into the root canal should be performed carefully as the creation of porosities and voids within the cement layer may also affect the long-term stability of the bonding interface [125]. Moreover, the use of EDTA as dentine pre-treatment before bonding procedures seems to offer some benefits only when using self-adhesive systems [126], while it seems to reduce the bond strength of etch-and-rinse based adhesive systems [127]. Conversely, the use of ethanol and chlorhexidine as dentine pre-treatment before bonding procedures to improve the long-term bonding performance seems to be controversial [128 – 130]. In conclusion, no clinical recommendations can be provided, other than ensuring a clean and adequately dried dentinal surface to have an ideal and standardised adhesive luting procedure [7].
Bibliography
- Hickel R, Manhart J. Longevity of restorations in posterior teeth and reasons for failure. J Adhes Dent 2001;3:45–64.
- Demarco FF, Corrêa MB, Cenci MS, et al. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater 2012;28:87-101.
- Carvalho RM, Manso AP, Geraldeli S, et al. Durability of bonds and clinical success of adhesive restorations. Dent Mater 2012;28:72–86.
- Cenci MS, Donassollo TA, Loguércio AD, et al. A clinical evaluation of posterior composite restorations: 17-year findings. J Dent 2006;34:427-35.
- Mjör IA, Dahl JE, Moorhead JE. Age of restorations at replacement in permanent teeth in general dental practice. Acta Odontol Scand 2000;58:97–101.
- Collins CJ, Bryant RW, Hodge KL. A clinical evaluation of posterior composite resin restorations: 8-year findings. J Dent 1998;26:311–7.
- Bhuva B, Giovarruscio M, Rahim N, et al. The restoration of root filled teeth: a review of the clinical literature. Int Endod J. 2021;54:509-535.
- Mannocci F, Bertelli E, Sherriff M, et al. Three-year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restoration. J Pros Dent 2002;88: 297–301.
- Sauro S, Pashley HD. Strategies to stabilise dentine-bonded interfaces through remineralising operative approaches – State of The Art. Int J Adhes Adhes. 2016; 69: 39-57
- Pashley DH, Tay FR, Breschi L, et al. State of the art etch-and-rinse adhesives. Dent Mater 2011;27:1–16.
- Van Meerbeek B, De Munck J, Yoshida Y, et al. Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent 2003;28:215–35.
- Perdigão J, Reis A, Loguercio AD. Dentin adhesion and MMPs: a Comprehensive review. J Esthet Restor Dent 2013;25:219–41.
- Chen H, Feng S, Jin Y, et al. Comparison of bond strength of universal adhesives using different etching modes: A systematic review and meta-analysis. Dent Mater J. 2021.
- Perdigão J, Reis A, Loguercio AD. Dentin adhesion and MMPs: a Comprehensive review. J Esthet Restor Dent 2013;25:219–41
- Tjäderhane L, Nascimento FD, Breschi L, et al. Strategies to prevent hydrolytic degradation of the hybrid layer – A review. Dent Mater 2013;29:999–1011.
- Pashley DH, Tay FR, Breschi L, et al. State of the art etch-and-rinse adhesives. Dent Mater 2011;27:1–16.
- Tay FR, Pashley DH. Water treeing–a potential mechanism for degradation of dentin adhesives. Am J Dent 2003;16:6–12.
- Sauro S, Watson TF, Mannocci F, et al. Two-photon laser confocal microscopy of micropermeability of resin-dentin bonds made with water or ethanol wet bonding. J Biomed Mater Res :Appl Biomater 2009;90:327–37.
- Sauro S, Mannocci F, Toledano M, et al. Influence of the hydrostatic pulpal pressure on droplets formation in current etch-and-rinse and self-etch adhesives: a video rate/TSM microscopy and fluid filtration study. Dent Mater 2009;25:1392–402.
- Park JG, Ye Q, Topp EM, et al. Preparation and properties of novel dentin adhesives with esterase resistance. J Appl Polym Sci 2008;107:3588–97.
- De Munck J, Van Landuyt K, Peumans M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res 2005;84:118–32.
- Mazzoni A, Mannello F, Tay FR, et al. Zymographic analysis and characterization of MMP-2 and -9 forms in human sound dentin. J Dent Res 2007;86:436–40.
- Sulkala M, Wahlgren J, Larmas M, et al. The effects of MMP inhibitors on human salivary MMP activity and caries progression in rats. J Dent Res 2001;80:1545–9.
- Nishitani Y, Yoshiyama M, Wadgaonkar B, et al. Activation of gelatinolytic/collagenolytic activity in dentin by self-etching adhesives. Eur J Oral Sci 2006;114:160–6.
- Hashimoto M. A Review – A review–micromorphological evidence of degradation in resin-dentin bonds and potential preventional solutions. J Biomed Mater Res B: Appl Biomater 2010;92:268–80.
- Anchieta RB, Machado LS, Martini AP, et al. Effect of long-term storage on nanomechanical and morphological properties of dentin-adhesive interfaces. Dent Mater 2015;31:141–53.
- Schulze KA, Oliveira SA, Wilson RS, et al. Effect of hydration variability on hybrid layer properties of a self-etching versus an acid-etching system. Biomaterials 2005;26:1011–8.
- Yoshida Y, Yoshihara K, Nagaoka N, et al. Self-assembled nano-layering at the adhesive interface. J Dent Res 2012;91:376–81.
- De Munck J, Van Landuyt K, Peumans M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res 2005;84:118–32.
- Van Meerbeek B, Yoshihara K, Yoshida Y, et al. State of the art of self-etch adhesives. Dent Mater 2011;27:17–28.
- Sidhu SK, Watson TF. Interfacial characteristics of resin-modified glass-ionomer materials: a study on fluid permeability using confocal fluorescence microscopy. J Dent Res 1998;77:1749–59.
- Hegde NN, Attavar SH, Hegde MN, Priya G. Antibacterial activity of dental restorative material: An in vitro study. J Conserv Dent. 2018;21:42-46.
- Boeckh C, Schumacher E, Podbielski A, Haller B. Antibacterial activity of restorative dental biomaterials in vitro. Caries Res 2002;36:101-7.
- Pires PM, Neves AA, Makeeva IM, et al. Contemporary restorative ion-releasing materials: current status, interfacial properties and operative approaches. Br Dent J. 2020;229:450-458.
- Wilson AD. Glass-ionomer cement–origins, development and future. Clin Mater 1991;7:275–82.
- De Munck J, Van Meerbeek B, Yoshida Y, et al. Four-year water degradation of a resin-modified glass-ionomer adhesive bonded to dentin. Eur J Oral Sci 2004;112:73–83.
- Hoshika S, De Munck J, Sano H, et al. Effect of conditioning and aging on the bond trength and interfacial morphology of glassionomer cement bonded to dentin. J Adhes Dent 2015;17:141–6.
- Hoshika S, Ting S, Ahmed Z, et al. Effect of conditioning and 1 year aging on the bond strength and interfacial morphology of glass-ionomer cement bonded to dentin. Dent Mater 2021;37:106-112.
- Sato T, Takagaki T, Ikeda M, et al. Effects of Selective Phosphoric Acid Etching on Enamel Using "No-wait" Self-etching Adhesives. J Adhes Dent. 2018;20:407-415.
- van de Sande FH, Rodolpho PA, Basso GR, et al. 18-year survival of posterior composite resin restorations with and without glass ionomer cement as base. Dent Mater 2015;31:669-75.
- Arhun N, Celik C, Yamanel K. Clinical evaluation of resin-based composites in posterior restorations: Two-year results. Oper Dent 2010; 35: 397–404.
- Ferracane JL. Resin composite–state of the art. Dent Mater 2011; 27: 29–38.
- Kakaboura A, Rahiotis C, Watts D, et al. 3D-marginal adaptation versus setting shrinkage in light-cured microhybrid resin composites. Dent Mater 2007: 23: 272–278.
- Boaro LC, Froes-Salgado NR, Gajewski VE, et al. Correlation between polymerization stress and interfacial integrity of composites restorations assessed by different in vitro tests. Dent Mater 2014; 30: 984–992.
- Van Dijken JW, Lindberg A. A 15-year randomized controlled study of a reduced shrinkage stress resin composite. Dent. Mater 2015; 31:1150–1158.
- He Z, Shimada Y, Sadr A, et al. The effects of cavity size and filling method on the bonding to Class I cavities. J Adhes Dent 2008; 10: 447–453.
- Sakaguchi RL, Peters MC, Nelson SR, et al. Effects of polymerization contraction in composite restorations. J Dent 1992; 20: 178–182.
- Davidson CL, de Gee AJ, Feilzer A. The competition between the composite-dentin bond strength and the polymerization contraction stress. J Dent Res 1984; 63: 1396–1399.
- De Munck J, Van Landuyt K, Coutinho E, et al. Micro-tensile bond strength of adhesives bonded to Class-I cavity-bottom dentin after thermo-cycling. Dent Mater 2005; 21: 999–1007.
- Fleming GJ, Cara RR, Palin WM, Burke FJ Cuspal movement and microleakage in premolar teeth restored with resin-based filling materials cured using a ‘soft-start’ polymerisation protocol. Dent Mater 2007; 23: 637–643.
- Bernardo M, Luis H, Martin MD, et al. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J Am Dent Assoc 2007; 138: 775–783.
- He Z, Shimada Y, Tagami J. The effects of cavity size and incremental technique on micro-tensile bond strength of resin composite in Class I cavities. Dent Mater 2007; 23: 533–538.
- Nikolaenko SA, Lohbauer U, Roggendorf M, et al. Influence of c-factor and layering technique on microtensile bond strength to dentin. Dent Mater 2004; 20: 579–585.
- Irie M, Suzuki K, Watts DC. Immediate performance of self-etching versus system adhesives with multiple light-activated restoratives. Dent Mater 2004; 20: 873–880.
- Irie M, Suzuki K, Watts DC, Marginal gap formation of light-activated restorative materials: Effects of immediate setting shrinkage and bond strength. Dent Mater 2002; 18: 203–210.
- Sampaio PC, de Almeida Junior AA, Francisconi LF, et al. Effect of conventional and resin-modified glass-ionomer liner on dentin adhesive interface of Class I cavity walls after thermocycling. Oper Dent 2011; 36: 403–412.
- Sauro S, Faus-Matoses V, Makeeva I, et al. Effects of Polyacrylic Acid Pre-Treatment on Bonded-Dentine Interfaces Created with a Modern Bioactive Resin-Modified Glass Ionomer Cement and Subjected to Cycling Mechanical Stress. Materials 2018; 11: 1884.
- Toledano M, Cabello I, Aguilera FS, et al. Effect of in vitro chewing and bruxism events on remineralization, at the resin-dentin interface. J Biomech 2015; 48: 14–21.
- Khvostenko D, Salehi S, Naleway SE, Hilton TJ, Ferracane JL, Mitchell JC, Kruzic JJ. Cyclic mechanical loading promotes bacterial penetration along composite restoration marginal gaps. Dent Mater 2015, 31, 702–710.
- Carvalho RM, Pereira JC, Yoshiyama M, Pashley DH. A review of polymerization contraction: the influence of stress development versus stress relief. Oper Dent 1996;21:17-24. .
- Versluis A, Douglas WH, Cross M, Sakaguchi RL. Does an incremental filling technique reduce polymerization shrinkage stresses? J Dent Res 1996;75:871-8.
- Hansen EK. Effect of cavity depth and application technique on marginal adaptation of resins in dentin cavities. J Dent Res 1986;65:1319-21.
- Umer F, Khan FR. Postoperative sensitivity in Class V composite restorations: comparing soft start vs. constant curing modes of LED. J Conserv Dent. 2011;14:76-9.
- Hilton TJ, Schwartz RS, Ferracane JL. Microleakage of four Class II resin composite insertion techniques at intraoral temperature. Quintessence Int 1997;28:135-44. .
- Son SA, Park JK, Seo DG, et al. How light attenuation and filler content affect the microhardness and polymerization shrinkage and translucency of bulk-fill composites? Clin Oral Investig. 2017;21:559-65.
- Fronza BM, Ayres A, Pacheco RR, Rueggeberg FA, Dias C, Giannini M. Characterization of Inorganic Filler Content, Mechanical Properties, and Light Transmission of Bulk-fill Resin Composites. Oper Dent 2017;42:445-55.
- Moszner N, Fischer UK, Ganster B, et al. Benzoyl germanium derivatives as novel visible light photoinitiators for dental materials. Dent Mater 2008;24:901-7.
- Banerjee A. Minimal intervention dentistry: part 7. Minimally invasive operative caries management: rationale and techniques. Br Dent J 2013;214:107–11
- Black RB. Airbrasive: some fundamentals. J Am Dent Assoc 1950;41:701–10,
- Hegde VS, Khatavkar RA. A new dimension to conservative dentistry: air abrasion. J Conserv Dent 2010;13:4–8,
- McComb D. Systematic review of conservative operativecaries management strategies. J Dent Educ 2001;65:1154–61.
- Banerjee A, Kidd EA, Watson TF. In vitro evaluation of five alternative methods of carious dentine excavation. CariesRes 2000;34:144–50,
- Cook RJ, Azzopardi A, Thompson ID, Watson TF. Real-time confocal imaging, during active air abrasion — substratecutting. J Microsc 2001;203:199–207,
- Rafique S, Fiske J, Banerjee A. Clinical trial of anair-abrasion/chemomechanical operative procedure for therestorative treatment of dental patients. Caries Res 2003;37:360–4,
- Tan MH, Hill RG, Anderson P. Comparing the air abrasioncutting efficacy of dentine using a fluoride-containingbioactive glass versus an alumina abrasive: an in vitro study. Int J Dent 2015; 2015: 521901,
- Spagnuolo G, Pires PM, Calarco A, et al. An in-vitro study investigating the effect of air-abrasion bioactive glasses on dental adhesion, cytotoxicity and odontogenic gene expression. Dent Mater 2021;37:1734-1750.
- Wong FS, Willmott NS, Davis GR. Dentinal carious lesion inthree dimensions. Int J Paediatr Dent 2006;16:419–23
- Schneider LF, Cavalcante LM, Silikas N. Shrinkage stresses generated during resin-composite applications: a review. J Dent Biomech 2010;2010:131630
- Johnson EW, Castaldi CR, Gau DJ, Wysocki GP. Stress pattern variations in operatively prepared human teeth, studied by three-dimensional photoelasticity. J Dent Res1968;47:548–58,
- Ayad MF, Maghrabi AA, Saif RE, García-Godoy F. Influence of tooth preparation burs on the roughness and bond strengthof adhesives to human dentin surfaces. Am J Dent 2011;24:176–82.
- Sauro S, Watson TF, Thompson I, et al. Influence of air-abrasion executed withpolyacrylic acid-Bioglass 45S5 on the bonding performanceof a resin-modified glass ionomer cement. Eur J Oral Sci 2012;120:168–77.
- Sauro S, Watson TF, Thompson I, Banerjee A. One-bottleself-etching adhesives applied to dentine air-abraded usingbioactive glasses containing polyacrylic acid: an in vitromicrotensile bond strength and confocal microscopy study. J Dent 2012;40:896–905.
- ishimura K, Nikaido T, Foxton RM, Tagami J. Effect ofair-powder polishing on dentin adhesion of a self-etchingprimer bonding system. Dent Mater J 2005;24:59–65.
- Zhong JP, LaTorre GP, Hench LL. The kinetics of bioactiveceramics. Part VII: binding of collagen to hydroxyapatite andbioactive glass. In: Andersson ÖH, Yli-Urpo A, editors.Bioceramics, Vol. 7. 1994. p. 61–6.
- Hench LL, Paschall HA. Direct chemical bond of bioactiveglass-ceramic materials to bone and muscle. J Biomed MaterRes 1973;7:25–42.
- Efflandt SE, Magne P, Douglas WH, Francis LF. Interactionbetween bioactive glasses and human dentin. J Mater SciMater Med 2002;13:557–65.
- Osorio R, Yamauti M, Sauro S, et al. Experimental resin cements containing bioactive fillersreduce matrix metalloproteinase-mediated dentin collagendegradation. J Endod 2012;38:1227–32.
- Osorio R, Yamauti M, Sauro S, et. Zinc incorporation improves biological activity of beta-tricalciumsilicate resin-based cement. J Endod 2014;40:1840–5.
- Gubler M, Brunner TJ, Zehnder M, et al. Do bioactive glasses convey a disinfecting mechanism beyond a mere increase in pH? Int Endod J 2008;41:670–678.
- Allan I, Newman H, Wilson M. Antibacterial activity of particulate bioglass against supra- and subgingival bacteria. Biomaterials. 2001;22:1683–1687.
- Khvostenko D, Hilton TJ, Ferracane JL, et al. Bioactive glass fillers reduce bacterial penetration into marginal gaps for composite restorations. Dent Mater. 2016;32:73-81.
- Kidd E, Beighton D. Prediction of secondary caries around tooth-colored restorations: a clinical and microbiological study. J Dent Res 1996;75:1942–1946.
- Choi K, Condon J, Ferracane J. The effects of adhesive thickness on polymerization contraction stress of composite. J Dent Res 2000;79:812–817
- Pongprueksa P, Kuphasuk W, Senawongse P. Effect of elastic cavity wall and occlusal loading on microleakage and dentin bond strength. Oper dent 2007;32:466–475.
- Vandewalle KS, Ferracane JL, Hilton TJ, Erickson RL, Sakaguchi RL. Effect of energy density on properties and marginal integrity of posterior resin composite restorations. Dent Mater. 2004;20:96–106.
- Torbjorner A, Fransson B. A literature review on the prosthetic treatment of structurally compromised teeth. Int J Pros 2004; 17, 369–76.
- Brito-Junior M, Pereira RD, Verıssimo C et al. Fracture resistance and stress distribution of simulated immature teeth after apexification with mineral trioxide aggregate. Int End J 2014; 47: 958–66.
- Nikhil V, Jha P, Aggarwal A. Comparative evaluation of fracture resistance of simulated immature teeth restored with glass fibre posts, intracanal composite resin, and experimental dentine posts. The Scientific World Journal. 2015; 751425.
- Zicari F, Van Meerbeek B, Scotti R, Naert I. Effect of fibre post length and adhesive strategy on fracture resistance of endodontically treated teeth after fatigue loading. J Dent 2012; 40, 312–21.
- 100.Borelli B, Sorrentino R, Zarone F, Ferrari M. Effect of the length of glass fibre posts on the fracture resistance of restored maxillary central incisors. Am J Dent 2012; 25: 79–83.
- 101.Naumann M, Neuhaus KW, Kolpin M, Seemann R. Why, when, and how general practitioners restore endodontically treated teeth: a representative survey in Germany. Clin Oral Invest 2016; 20: 253–9.
- 102.Bitter K, Noetzel J, Stamm O et al. Randomized clinical trial comparing the effects of post placement on failure rate of postendodontic restorations: preliminary results of a mean period of 32 months. J Endod 2009; 35: 1477–82.
- 103.Fokkinga WA, Kreulen CM, Bronkhorst EM, Creugers NH. Up to 17-year controlled clinical study on postand-cores and covering crowns. J Dent 2007; 35:778–86.
- 104.Fokkinga WA, Kreulen CM, Bronkhorst EM, Creamers NH. Composite resin core-crown reconstructions: an up to 17-year follow-up of a controlled clinical trial. Int J Pros 2008; 21: 109–15.
- 105.Mannocci F, Qualtrough AJ, Worthington HV, et al. Randomized clinical comparison of endodontically treated teeth restored with amalgam or with fibre posts and resin composite: five-year results. Oper Dent 2005; 30: 9–15.
- 106.Ellner S, Bergendal T, Bergman B. Four post-and-core combinations as abutments for fixed single crowns: a prospective up to 10-year study. Int J Pros 2003; 16: 249–54.
- 107.Cloet E, Debels E, Naert I. Controlled clinical trial on the outcome of glass fibre composite cores versus wrought posts and cast cores for the restoration of endodontically treated teeth: a 5-year follow-up study. Int J Pros 2017; 30: 71–9.
- 108.Tay FR, Pashley DH. Monoblocks in root canals: a hypothetical or a tangible goal. J Endod 2007; 33: 391–8.
- 109.Zhou L, Wang Q. Comparison of fracture resistance between cast posts and fibre posts: a meta-analysis of literature. J Endod 2013;201339: 11–5.
- 110.Naumann M, Sterzenbach G, Dietrich T, et al. Dentin-like versus rigid endodontic post: 11-year randomized controlled pilot trial on no-wall to 2-wall defects. . J Endod 2017; 43: 1770–5.
- 111.Figueiredo FE, Martins-Filho PR, Faria ESAL. Do metal post-retained restorations result in more root fractures than fibre post-retained restorations? A systematic review and meta-analysis. . J Endod 2015; 41: 309–16.
- 112.Sarkis-Onofre R, Skupien JA, Cenci MS, Moraes RR, Pereira-Cenci T. The role of resin cement on bond strength of glass-fibre posts luted into root canals: a systematic review and meta-analysis of in vitro studies. Oper Dent 2014; 39: E31–44.
- 113.Lang H, Korkmaz Y, Schneider K, Raab WH. Impact of endodontic treatments on the rigidity of the root. J Dent Res 2006; 85: 364–8.
- 114.Ikram OH, Patel S, Sauro S, Mannocci F. Micro-computed tomography of tooth tissue volume changes following endodontic procedures and post space preparation. Int Endod J 2009; 42: 1071–6.
- 115.Ferrari M, Vichi A, Fadda GM et al. A randomized controlled trial of endodontically treated and restored premolars. Journal of Dental Research 2012; 91: S72–8.
- 116.Rasimick BJ, Wan J, Musikant BL, Deutsch AS. A review of failure modes in teeth restored with adhesively luted endodontic dowels. J Prosth 2010; 19: 639–46.
- 117.Mjor IA, Smith MR, Ferrari M, Mannocci F. The structure of dentine in the apical region of human teeth. Int End J 2001; 34, 346–53.
- 118.Tay FR, Loushine RJ, Lambrechts P, Weller RN, Pashley DH. Geometric factors affecting dentin bonding in root canals: a theoretical modeling approach. J Endod 2005; 31: 584–9.
- 119.Goracci C, Corciolani G, Vichi A, Ferrari M. Light transmitting ability of marketed fibre posts. J Dent Res 2008; 87, 1122–6.
- 120.Daneshpoor N, Pishevar L. Comparative evaluation of bioactive cements on biomimetic remineralisation of dentin. J Clin Exp Dent. 2020;12:e291-e299.
- 121.Owens B. Bioactivity, Biocompatibility and Biomimetic Properties for Dental Materials: Clarifying the Confusion? Modern Approaches in Dentistry and Oral Health Care. 2018 (2).
- 122.Bergoli CD, Brondani LP, Wandscher VF et al. A multicenter randomized double-blind controlled clinical trial of fibre post cementation strategies. Oper Dent 2018; 43: 128–35.
- 123.Breschi L, Mazzoni A, Dorigo ED, Ferrari M. Adhesion to intraradicular dentin: a review. J Adhes Sci Tech 2009; 23, 1053–83.
- 124.Goracci C, Sadek FT, Fabianelli A, et al. Evaluation of the adhesion of fibre posts to intraradicular dentin. Oper Dent 2005, 627–35.
- 125.Soares AP, Bitter K, Lagrange A, et al. Gaps at the interface between dentine and self-adhesive resin cement in post-endodontic restorations quantified in 3D by phase contrast-enhanced micro-CT. Int Endod J 2020; 53: 392–402.
- 126.Gu XH, Mao CY, Liang C, Wang HM, Kern M. Does endodontic post space irrigation affect smear layer removal and bonding effectiveness? Eur J Oral Sci 2009; 117: 597–603.
- 127.Bitter K, Hambarayan A, Neumann K, et al. Various irrigation protocols for final rinse to improve bond strengths of fibre posts inside the root canal. Eur J Oral Sci 2013; 121: 349–54.
- 128.Cecchin D, de Almeida JF, Gomes BP, et al. Influence of chlorhexidine and ethanol on the bond strength and durability of the adhesion of the fibre posts to root dentin using a total etching adhesive system. J Endod; 2011; 37: 1310–5.
- 129.Cecchin D, Giacomin M, Farina AP, et al. Effect of chlorhexidine and ethanol on push-out bond strength of fibre posts under cyclic loading. J Adh Dent 2014; 16: 87–92.
- 130.Bitter K, Aschendorff L, Neumann K, et al. Do chlorhexidine and ethanol improve bond strength and durability of adhesion of fibre posts inside the root canal? Clin Oral Inv 2014; 18: 927–34.



