Adhesive Direct Restoration in the Posterior Area with Subgingival Cervical Margins
26/09/2022
Davide Guglielmi
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Localized subgingival margins can complicate the use of direct adhesive restorations and subsequently hinder their durability and relation with the periodontal tissues. This article presents a technique involving placement of a modified matrix followed by immediate dentin sealing and coronal elevation of the deep margin to a supra- gingival position using a direct bonded composite resin base (DMR).
The deep margin elevation technique may be a useful non-invasive alternative to surgical crown lengthening.
Sub-gingival interdental margins may be encountered when replacing large class II restorations.
Such cases generate significant technical and operative challenges during isolation of the operatory field using rubber dam, adhesive procedures, impression taking (traditional or optical), and adhesive luting. When not properly executed, these procedures may affect the longevity of the restoration and its relationship with marginal periodontal tissues.
There are various clinical approaches to such challenges. The gingival margins can be surgically exposed by apical displacement of supporting tissues; however, this may lead to attachment loss and anatomical complications such as the proximity of root concavities and furcations. Once exposed to the oral environment, the gingival margins can be difficult to maintain and may generate additional challenges.
Another approach, presented by Dietschi and Spreafico in 1998, is to place a base of composite resin to coronally displace proximal margins: cervical margin relocation (CMR).
In a following paper, a new classification is based on these two clinical parameters:
- a technical-operative parameter (possibility of correct isolation through the dental dam)
- a biological parameter (depending on the biologic width).
Three different clinical situations and three different therapeutic approaches are identified (1st, 2nd, and 3rd, respectively): coronal relocation of the margin, surgical exposure of the margin, and clinical crown lengthening.
Frequently, cavities of large dimensions extend beyond the cemento enamel junction (CEJ) with margins more or less deeply located in the gingival tissue and with little or no residual enamel. While adhesion to mordant-treated enamel is predictable and safe, adhesion to dentin and cementum is dependent on numerous and complex phenomena. The formation of an efficient hybrid layer is influenced by many clinical steps (etching, drying, primer application, bonding application), including the polymerization of adhesive resin that stabilizes the structure of the hybrid layer itself. The operating procedure described by Dietschi and Spreafico was then defined by means of an in vitro study by Olsburgh30 and establishes the following: rigorous isolation of the field with a dental dam, positioning of a matrix to guarantee a cervical seal, thorough cleansing of the cavity finishing with a bicarbonate spray, adhesive phase with a three-step etch-and-rinse method, and raising of the cervical step with flowable composite of maxi- mum 1 mm thickness. Following this protocol, 98% of margins obtained by the author were excellent. As mentioned above, the technique requires the use of flowables. Different authors higlined that when flowable is applied as the first cervical increment in Class II restorations, gingival micro-leakage is reduced and marginal integrity is improved. In particular, in an article by Dietschi et al, the authors clearly suggest that the use of a medium-rigid flowable composite (7.6 GPa) is a potentially valid material to displace, in a coronal position, proximal margins.
In the absence of reliable scientific evidence, but on the basis of published data and clinical experience, the importance and the systematic use of flowable composite, at the cervical level in the absence of enamel, can be supported according to the following rationale:
- interposition of an “elastic layer” of controlled thickness (0.5 to 1 mm) between the dental substratum and restoration material: this allows contraction stress to be absorbed and the adhesive interface to be preserved;
- fluid adaptation to the cavity floor with absence of blisters and visual control of the cervical seal prior to correct positioning of matrix and wedge straightening of the cervical margin as a result of burring immediate dentin sealing.
The final restoration issues concern the relation with soft tissue and therefore the frequent presence of subgingival margins.
The supra-crestal tissue attachment (STA),formerly known as biologic width, consists in the junctional epithelium and supra-crestal connective tissue attachment.
STA violation is believed to trigger adverse periodontal effects, although the specific aetiology (which has been proposed to be biofilm, trauma, material toxicity or a combination of these factors) is not clear. Mean STA apico-coronal dimension is found to be 2.15–2.30 mm; however, considerable variability exists according to tooth type, site, periodontal health and periodontal phenotype.
In light of the above, a clinical case will be, step by step described, according with the Veneziani classification (Grade 2) in which the rubber dam does not allow a correct isolation of the field but the supra-crestal connective is respected. This situation is made possible by the fact that in the posterior areas, particularly in patients with a thick periodontal phenotype, may presents both a greater height of the junctional epithelium and the gingival sulcus.

Fig. 1
Case of a 28 years old patient referring pain in the left lower jaw when chewing.
Both sensibility testing and bleeding on probing were positive,
Pocket probing depth of the element was ≤ 5 mm circumferentially except for the disto lingual aspect (6 mm).
A: lateral view
B: occlusal view

Fig. 2
Peri-apical X-Ray
The distance between the lower margin of the decayed tissue and the inter proximal bone peak among the elements 3.6 and 3.7, is evident.

Fig. 3
Pocket probing depth in the disto-lingual aspect of the element 3.6 (6 mm).
It is evident the bleeding on probing that could be referred to the loss of the hard tissue of the above mentioned tooth and the food impaction.

Fig. 4
Before assessing the correct therapy for the patient, the clinician must remove entirely the decayed tissue from the most apical portion of the cavity, in order to understand which would have been the bone probing dimension in the distal aspect of the tooth.
If this results to be higher than 1.5 mm, (in the light of the recent definitions of the supra-crystal tissues attachment from the AAP and EFP Consensus), it is possible to precede to the restorative therapy without performing any of the crown-lengthening techniques.
The video describes step by step the passages
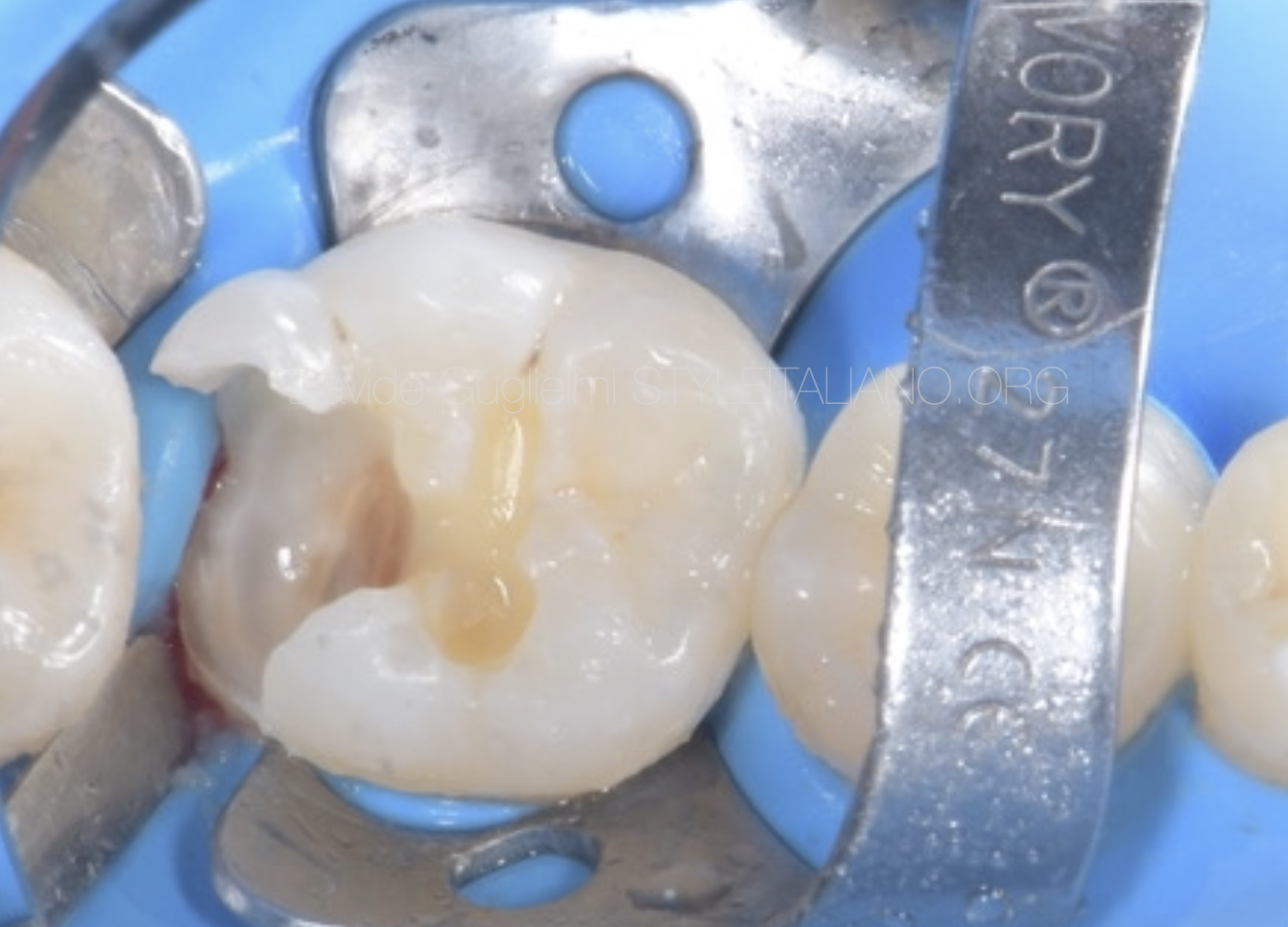
Fig. 5
Once the operative field is properly isolated (in this clinical case with 2 different clamps on the elements 3.6 and 3.7), the rubber dam must be heated into the sulcus in order to evince the most apical aspect of the cavity margin.
The video describes step by step the passages
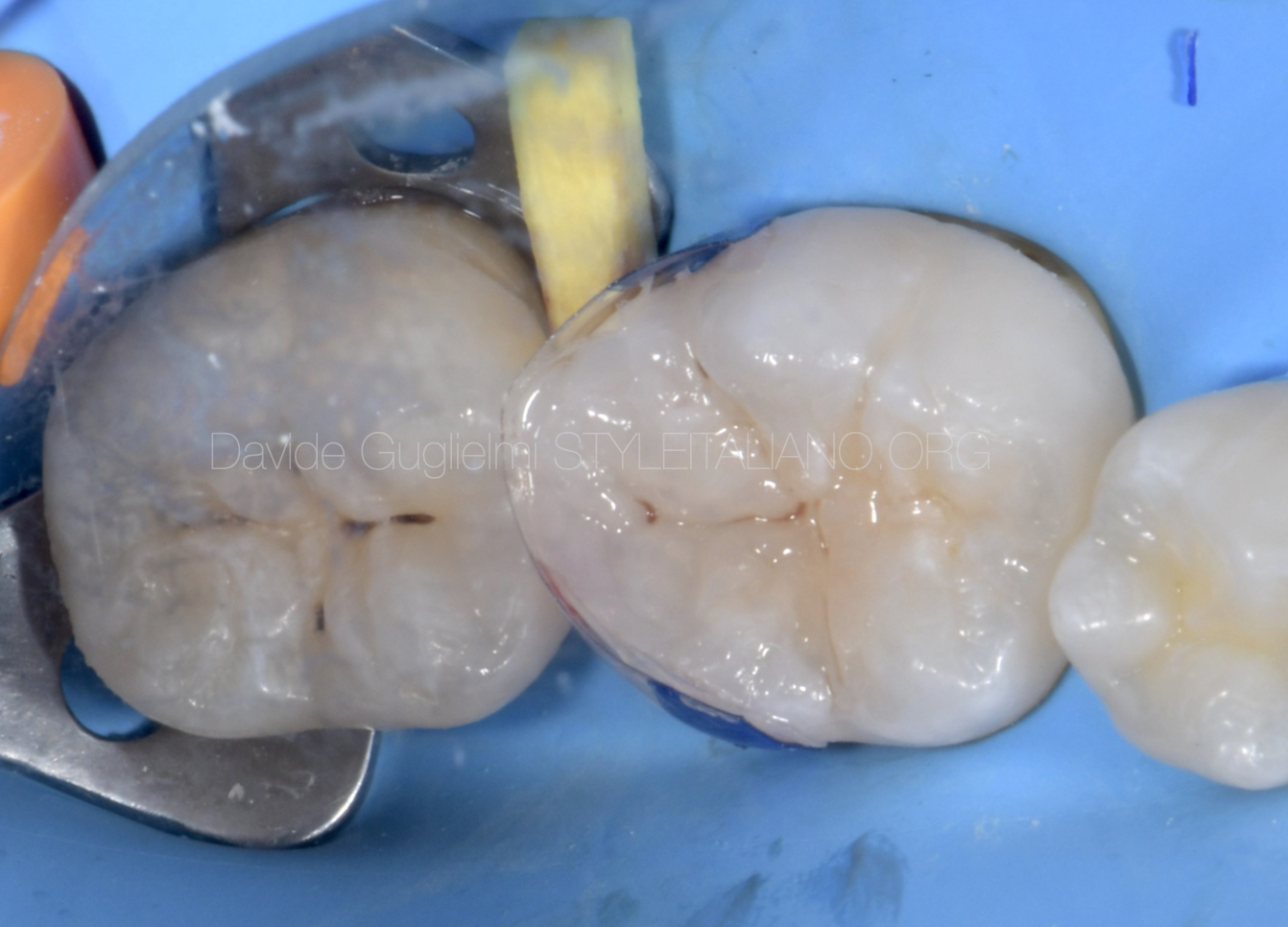
Fig. 6
A clinical occlusal picture of the reconstruction after the concluding adhesive passages and the cervical margin relocation techniques (before finishing and polishing).
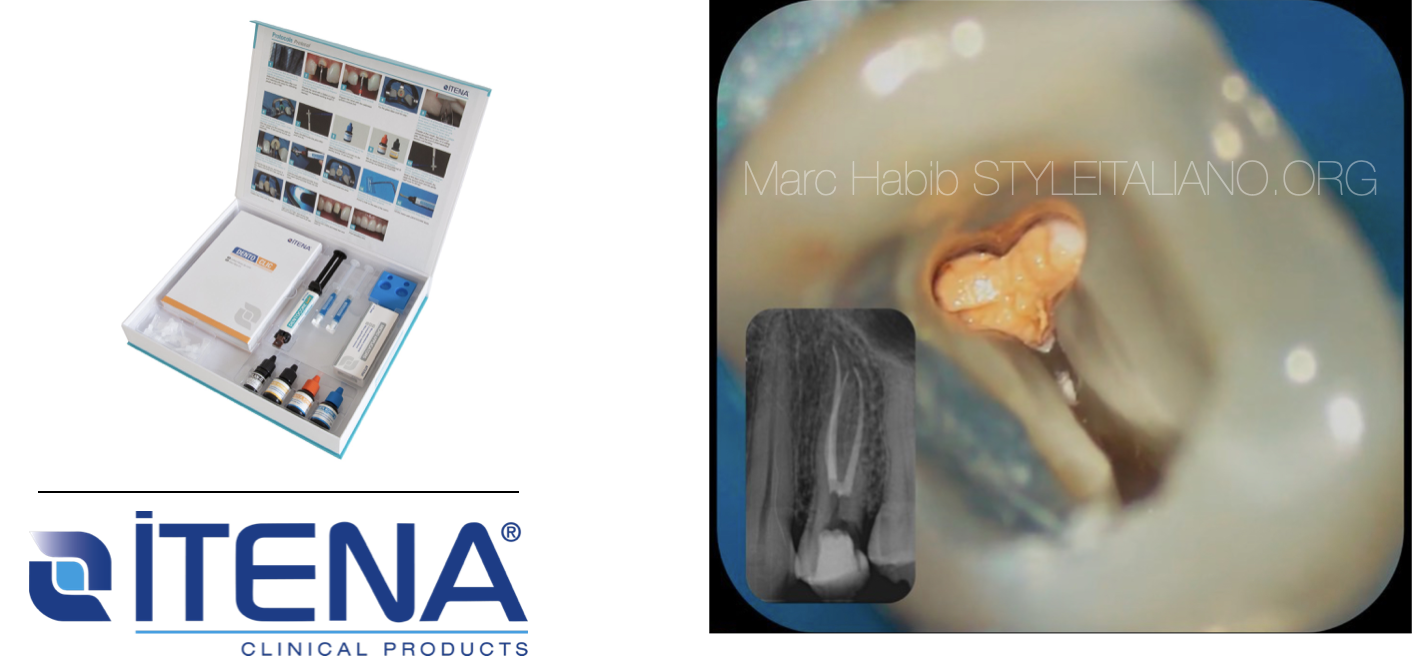
The materials used were:
- 37% ortho-phosphoric acid (Dentoetch, Itena Clinical)
- primer and bonding (QuickBond, Itena Clinical) (applied as suggested by the manufacturer)
- Nano - filled composite dual cure material(Dentocore Body, Itena Clinical) for the CMR technique.
- several layers of reflectys composite (Itena Clinical) for the restoration
- brown stain into the sulcus

Fig. 7
Occlusal view of the reconstruction before removing the rubber dam

Fig. 8
Products used for the restoration

Fig. 9
Post operative peri-apical X-ray.
Conclusions
Based on author knowledge and experience, the nano - filled composite dual cure material (Dentocore Body, Itena Clinical) may be used for the cervical margin restoration technique.
(ITENA CLINICAL) and ITENA Clinical's Reflectys Universal Restorative Composite seem to be perfect to achieve a strong structure and obtain an aesthetic satisfactory result.
However high-quality clinical trials are needed and , in clinical cases in which
It’s highly recommended to make the right diagnosis and the correct treatment plan before starting
Bibliography
- D. Dietschi, R. Spreafico, Adhesive metal-free restorations: current concepts for the esthetic treatment of posterior teeth, Quintessence 2 (1997) 60–77.
- D. Dietschi, R. Spreafico, Current clinical concepts for adhesive cementation of toothcolored posterior restorations, Pract. Periodontics Aesthet. Dent. 10 (1998) 47–54.
- Ercoli, C., & Caton, J. G. (2018). Dental prostheses and tooth-related factors. Journal of Clinical Periodontology, 45(5S), S207–S218.
- Veneziani M. Adhesive restorations in the posterior area with subgingival cervical margins: new classification and differentiated treatment approach. Eur J Esthet Dent. 2010 Spring;5(1):50-76.
- Discepoli N, Marruganti C, Santoro F, Mirra R, Fiorino F, Medaglini D, Pozzi G, Ferrari M, Grandini S. Impact of interproximal composite restorations on periodontal tissue health: Clinical and cytokine profiles from a pre-post quasi-experimental study. J Periodontol. 2022 Jun;93(6):911-923. Olsburg S. Graduation thesis. Geneva: Geneva University, 2000.
- Estafan D, Estafan A. Flow- able composite: a microleak- age study. J Dent Res 1998;77:938-942.
- Vacek JS, Gehr ME, Asad DA, Richardson AC, Giambarresi LI. The dimen- sions of the human dento- gingival junction. Int J Peri- odontics Restorative Dent 1994;14:154-165.
- De Sanctis M, Clementini M. Flap approaches in plastic periodontal and implant surgery: crit- ical elements in design and execution. (2014). Journal of Clinical Periodontology. 2014. 41(s15), S108–S122.