Management of Mandibular Incisor Tooth With Calcified Root Canal Anatomy
20/09/2023
Hayrullah Kaya
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Calcific metamorphosis or calcifications result from accelerated deposition of mineralized tissue into the root canal system due to trauma, external aggressors, orthodontic movements, caries lesions, occlusal imbalance, parafunctional habits, aging and previous restorative interventions. Pulp calcification can complicate the access cavity preparation and root canal identification. This can cause iatrogenic mishaps such as perforations and unnecessary dentin removal. There are various techniques to overcome the challenges of calcified root canals in a more predictable and less risky way. These following techniques assist the clinician in identifying canal orifices.
-Observation of different dentin colors and canal bleeding points
-Magnification tools; dental microscope, loupe,
-Dyes such as methylene blue, bubble test or "champagne effect",
-Pre-operative radiographs from different angulations ,
-CBCT with dynamic 3D navigation
-Periapical endodontic surgery
-Ultrasonic devices
The clinician must carefully evaluate the selection of imaging sources, instruments and tools to achieve success in treatment without excessive dentin wear and weakening of remaining coronal structure. In this case, DOM, CBCT and ultrasonic preparing were used to gain access the calcified root canal.

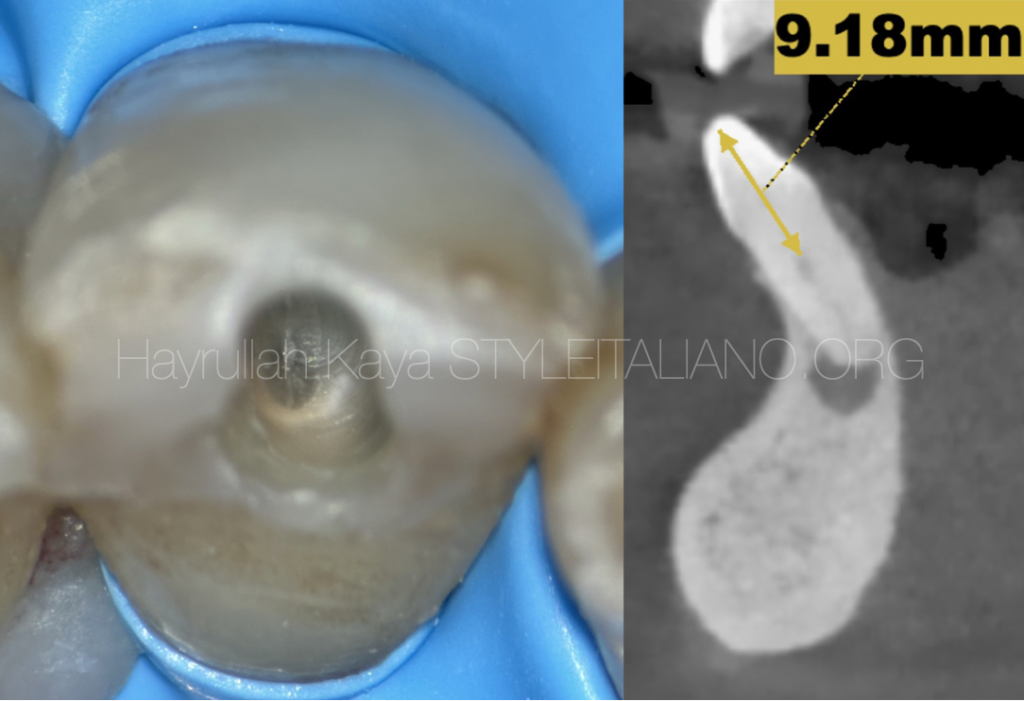
Fig. 1
Initial X-rays
When complete calcification of the coronal region was observed in the examined periapical film, a CBCT scan was requested from the patient to facilitate a more comprehensive examination
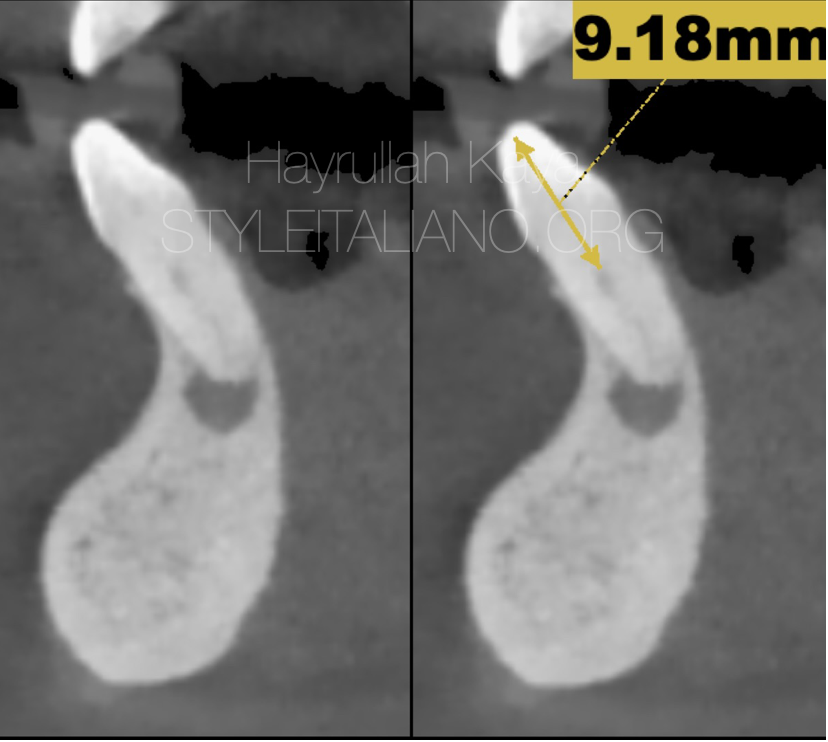
Fig. 2
It was determined that the position of the canal orifice began at a depth of 9.18 mm in the obtained tomography. The obtained findings indicate the presence of apical root resorption.

Fig. 3
Detection of the calcified part following access cavity preparation
After the identification of calcified area, it is tried to be advanced towards the canal orifice by using ultrasonic tips

Fig. 4
After the identification of calcified area, it is tried to be advanced towards the canal orifice by using ultrasonic tips
During the procedure, the stopper was removed to prevent interference with the working area while attempting to access the canal orifice. The stopper was reattached to the ultrasonic tip to check whether the desired length of 9.2 mm was reached.

Fig. 5
Determination of the canal orifice position after 9.2 mm
Determination of the canal orifice position after 9.2 mm

Fig. 6
Reductions in working length can occur following canal shaping procedures. It has been reported that measuring the canal length after pre-flaring reduces the canal length deviations.
Preflaring procedure before the working length determination
Preflaring process was made with file, the thickest part of which has a diameter of 0.8 mm.
The working length determination with Vdw 10 c pilot
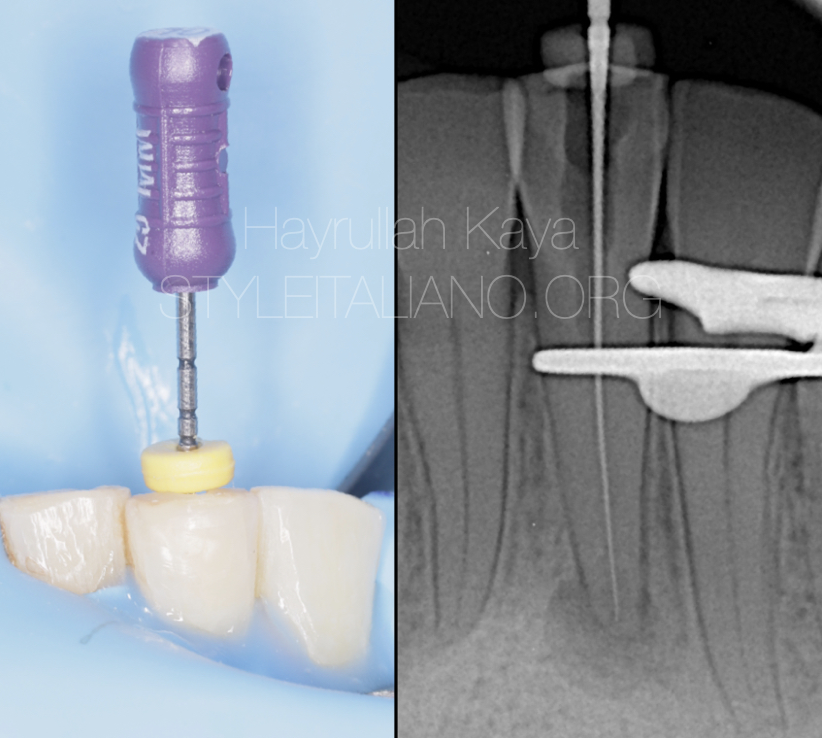
Fig. 7
The working length determination with the apex locator and confirmed with X-ray
Glide path process with reciprocal file
Following the glide path procedure, we completed the shaping process
After the completion of the shaping process, we carried out irrigation-activation procedures by applying our final irrigation protocol. Endo aspirator and paper points were used for the canal drying procedure
An apical plug was applied with MTA in the apical region due to the disruption of apical contraction. The MTA was placed in the root canal with MAP one system. It was advanced apically with the help of a pluger and gutta percha.

Fig. 8
Finishing X-ray
Conclusions
Conventional periapical radiographs and dental operating microscope could not provide sufficient information about the location of calcified canal orifices. The calcified area length was measured on CBCT then and placing a stopper on the ultrasonic tips. Therefore, the intraoperative use of CBCT was necessary and proved vital to successful positioning of calcified canal orifices.
Bibliography
1. Quaresma SA, da Costa RP, Ferreira Petean IB, Silva-Sousa AC, Mazzi-Chaves JF, Ginjeira A, Sousa-Neto MD. Root Canal Treatment of Severely Calcified Teeth with Use of Cone-Beam Computed Tomography as an Intraoperative Resource. Iran Endod J. 2022 Winter;17(1):39-47.
2. Floratos S, Miltiadous ME. Intraoperative Use of CBCT for Identification and Localization of Calcified Canals: A Clinical Technique. Case Rep Dent. 2017;2017:1265701.
3. Lara-Mendes STO, Barbosa CFM, Santa-Rosa CC, Machado VC. Guided Endodontic Access in Maxillary Molars Using Cone-beam Computed Tomography and Computer-aided Design/Computer-aided Manufacturing System: A Case Report. J Endod. 2018;44(5):875–9.
4. van der Meer WJ, Vissink A, Ng YL, Gulabivala K. 3D Computer aided treatment planning in endodontics. J Dent. 2016;45:67–72.