MG3 let's shape calcified and moderately curved root canals
24/08/2023
Viresh Chopra
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The process of root canal treatment involves the meticulous elimination of bacterial remnants within the canal through biomechanical techniques, encompassing thorough cleaning and precise shaping, all aimed at averting any potential reinfection1. The intricate nature of root canal anatomy necessitates the deployment of well-designed tools to effectively navigate and cleanse these intricate passages2. This endeavor of cleansing and sculpting the root canal systems employs a repertoire of methods, encompassing both manual and rotary instruments. The ultimate goal of this treatment modality is to craft a progressively tapered funnel-like configuration, wherein the apex boasts the narrowest diameter while the canal's orifice exhibits the widest span.
A profound understanding of root canal anatomy stands as an essential prerequisite for achieving successful outcomes in endodontic treatments. Mastery over the intricate nuances of both external and internal root canal morphology significantly contributes to the triumphant execution of root canal procedures. Within the realm of maxillary molars, a noteworthy aspect surfaces – the existence of an additional canal, namely MB2, nestled within the mesio buccal root. This distinctive trait, while bearing the semblance of an anomaly, is indeed a prevalent variation.
Notably, the significance of acknowledging the presence of this second mesiobuccal canal cannot be overstated. Weine (2004) insightfully posited that the recurrence of unsuccessful endodontic treatments in maxillary first permanent molars could be attributed, in part, to the oversight in locating and effectively filling the second mesiobuccal canal. This assertion was bolstered by Wolcott et al., whose findings illuminated the direct correlation between the omission of MB2 canal identification and subsequent reduction in long-term prognostic efficacy.
Stropko, a meticulous researcher, embarked on a comprehensive study involving 1096 maxillary first molars over an extensive 8-year span. His discerning investigation unveiled an intriguing trend – MB2 canals were discovered in an impressive 93% of first molars, a figure that slightly receded to 73.2% without the incorporation of surgical operating microscopes.
Traditionally, the radiographic medium has been the diagnostic mainstay for delineating complex root canal anatomies. However, the inherent limitations of periapical and panoramic radiography become palpable when seeking to unravel intricacies along the bucco-lingual dimension, even though their portrayal of mesio-distal details remains satisfactory.
In this narrative, we unveil a captivating case study, a portrait of a maxillary first molar that defies convention. A distinctive peculiarity in the form of an atypical MB2 orifice and canal location comes to light, a phenomenon heretofore absents from the annals of existing literature. An additional orifice, inconspicuously positioned adjacent to the palatal orifice, emerges as an unprecedented occurrence, further enriching the ever-evolving tapestry of endodontic exploration.

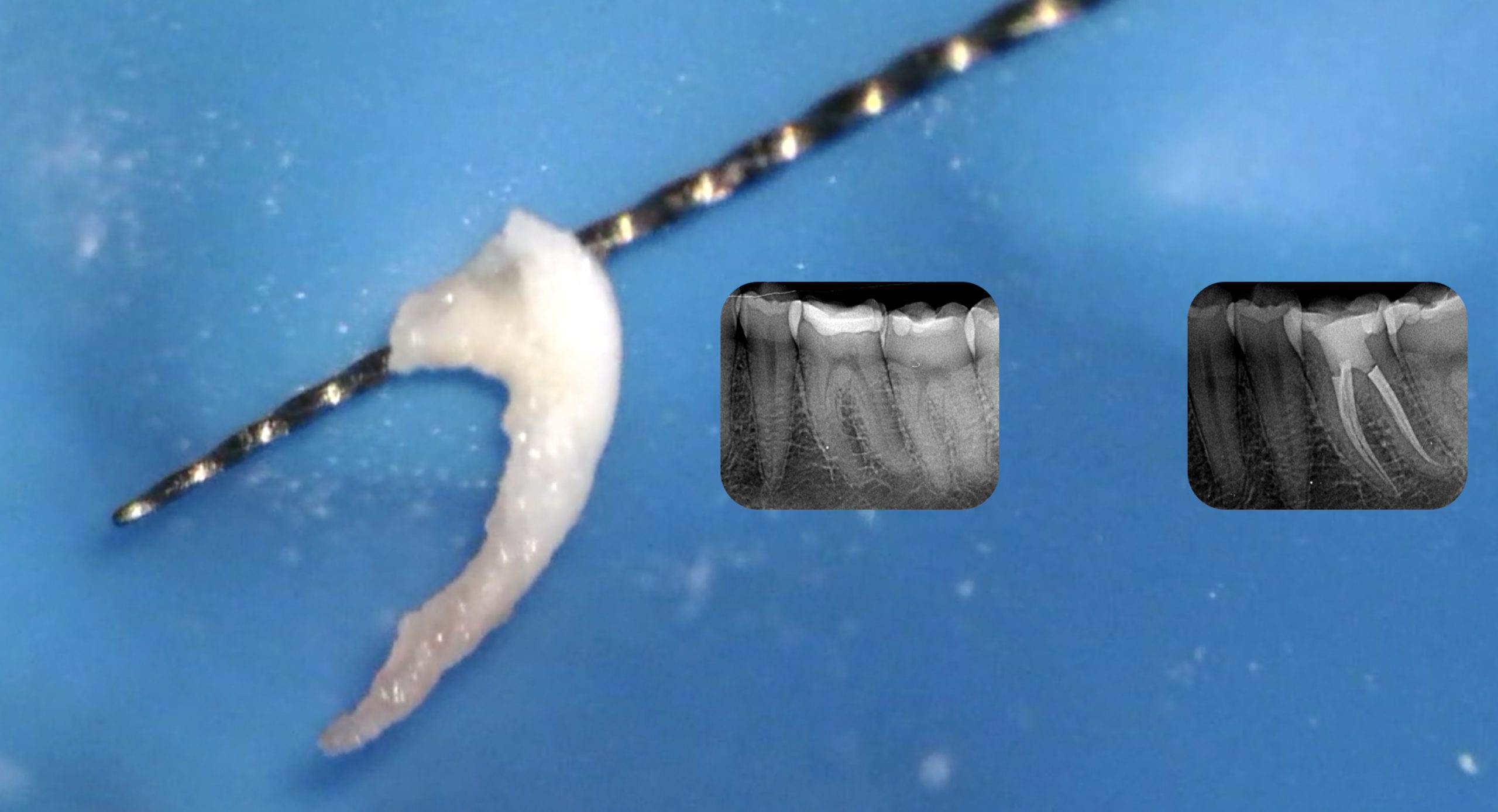
Fig. 1
Description of the case
Patient information
- ïAge:32-year-old
- ïGender: Male
- ïMedical history: non-contributory
- ïIdentification: Right maxillary molar (Tooth 26)
Clinical examination findings:
The tooth 26 has a metallic restorations done around 2 years back. However, the patient complains of severe pain while biting that disturbs his sleep and lifestyle. The tooth is tender to percussion with periodontal probing within normal limits.
Radiographic findings:
The periapical radiograph revealed suspected metallic restorations well within superficial dentin (Fig 1). Radiographically, the pulp chamber and root canals seemed to be constricted. Degenerative changes in the pulp chamber as well as root canals are evident on the radiograph.
Fig 1. Periapical radiograph showing 26 with deep mesio-occlusal carious lesion.
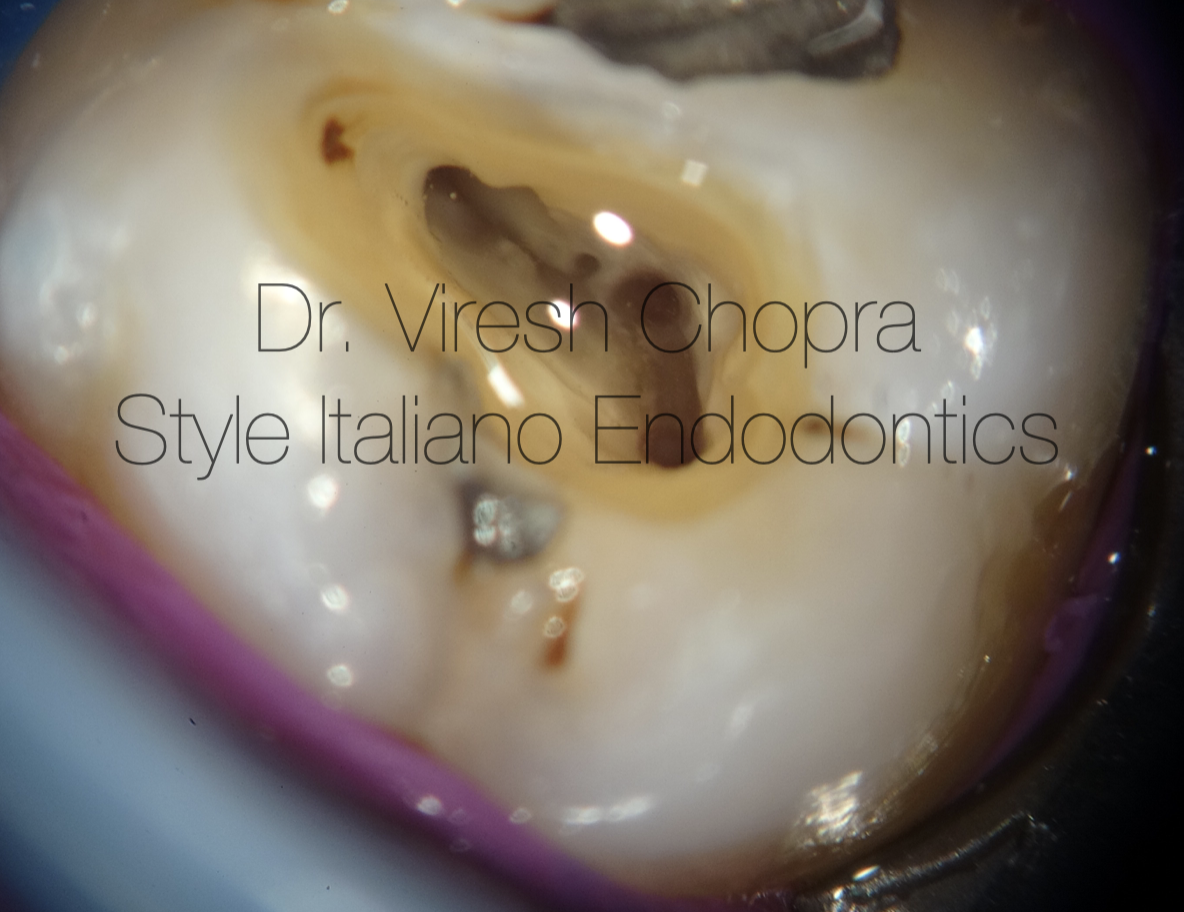
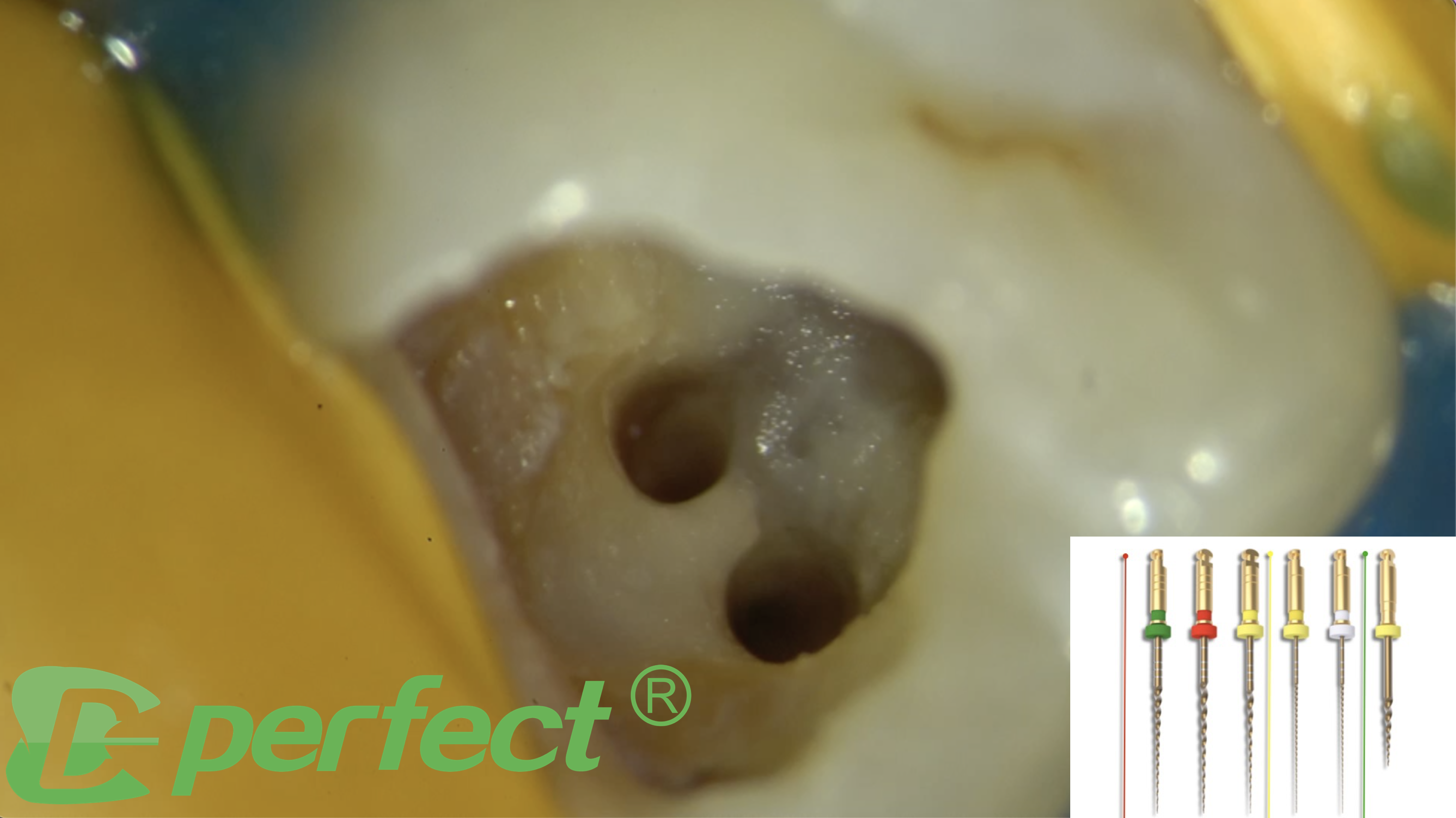
Fig. 2
Investigations:
- Tenderness to percussion present
- Pulp vitality testing showed delayed response.
Treatment plan: Root canal treatment followed by post-endodontic full coverage restoration.
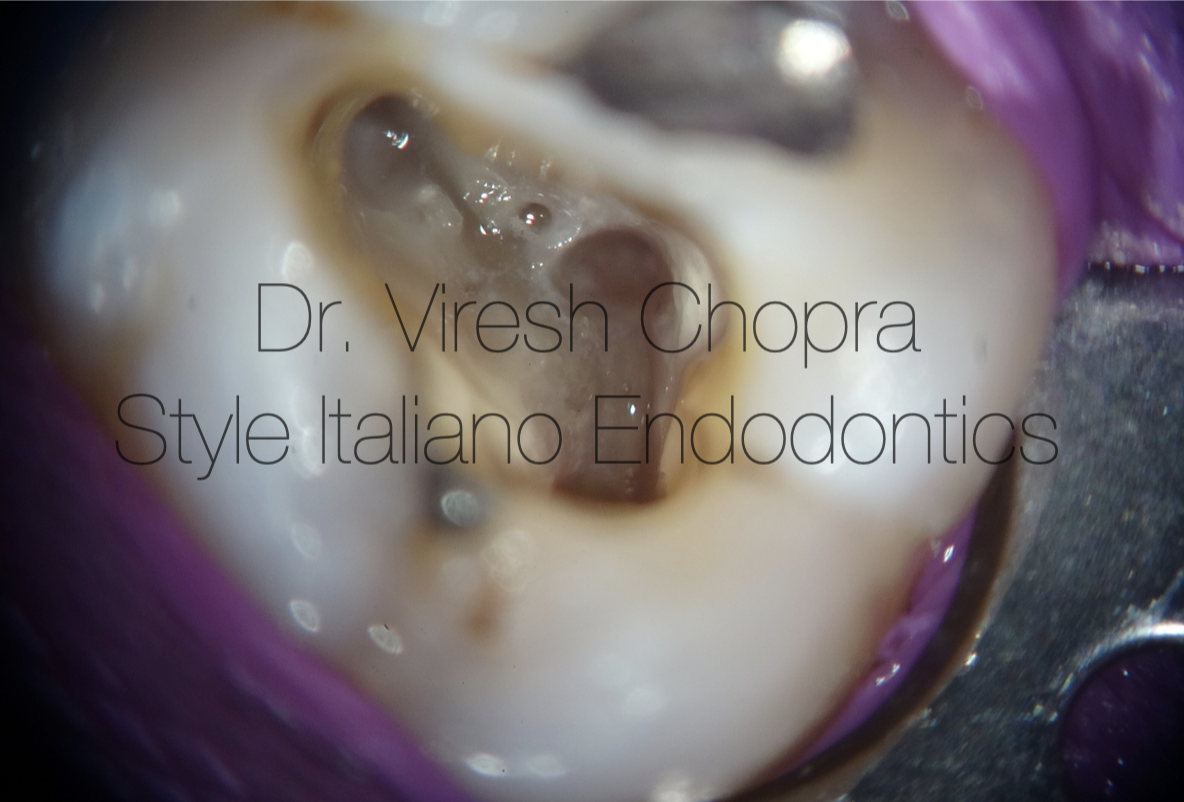
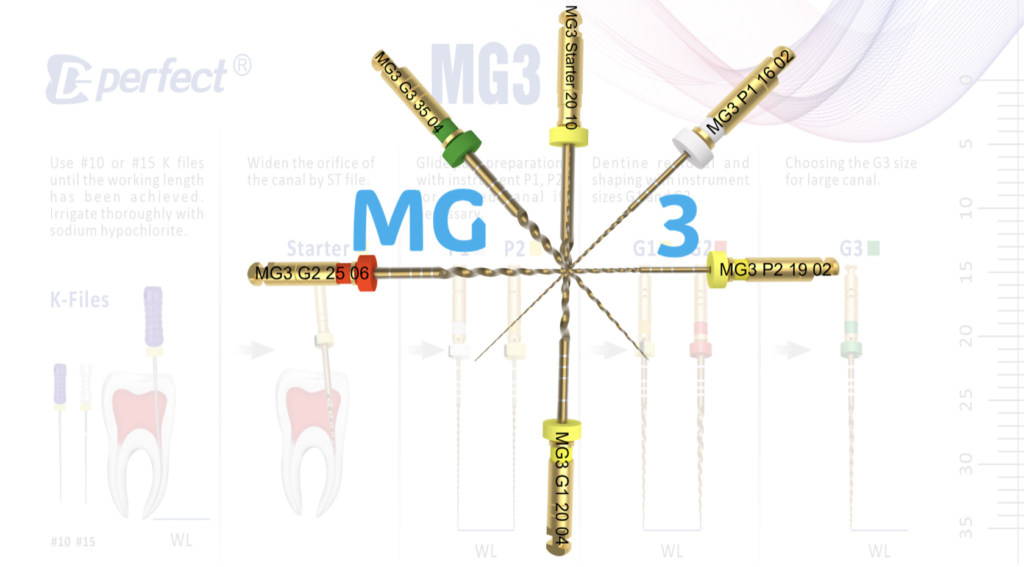
Fig. 3
Root canal treatment protocol followed:
The procedural journey embarked with the meticulous administration of buccal infiltration anaesthesia, ushering in a realm of numbing comfort. The tooth, a focal point of precision, was elegantly cloaked in the embrace of a rubber dam isolation, effectively segregating it from its surrounding environment. Under the watchful gaze of a microscope, its intricacies unfurled, revealing a miniature landscape brimming with potential.
As the initial steps paved the way, the choreography of care took centre stage. Carious excavation unfolded, a dance of precision that artfully liberated the tooth from its ailment. This entrée was succeeded by the grand performance of endodontic access cavity preparation, orchestrated by the Endo access burs. The result was an opening, a gateway into the inner sanctum of the tooth's secrets(Fig 2a)
With finesse and dexterity, the Endodontic explorer emerged as the lead actor, gracefully tracing the contours of the terrain. Four orifices, like celestial constellations, were unveiled, each a portal to the heart of the tooth's labyrinthine passages. These delicate orifices, akin to nature's intricate sculptures, awaited further exploration.
The unfolding narrative led to an interlude, a pause to widen the orifices. Here, the orifice opener, a 20/.10 file from the MG3 kit, assumed the role of an artisan, carefully expanding the pathways with a delicate touch (Fig 2b). This symphony of instrumentation harmoniously balanced precision and gentleness, a delicate cadence that celebrated the artistry of dentistry.
The glide path till the established Working length was established using P1 and P2 files (Video 1). The MB2 canal finished in the initial 10mm distance and could not be negotiated furthur. The canals were finally cleaned and shaped with using the MG3 files in the following sequence.
- Initial glide path using P1 and P2 files (video 1).
- Final shaping using G1 and G2 files (video 2).
Profuse irrigation was performed in between every instrument using 3% sodium hypochlorite for adequate disinfection. The canals were finally shaped using G2 file as the master apical file (video 2). Master cone fit was checked clinically as well as radiographically (Fig 3) and the canals were prepared for obturation. Obturation was performed using Calcium silicate sealer along with the Gutta percha cones (Fig 3) (video 3). Recommended single cone obturation technique was used with Calcium silicate sealers. The obturation was verified Clinically (Fig 4, video 4) and radiographically (Fig 5)
Video 2: Cleaning and shaping with G1 and G2 files

Fig. 4
Radiographic verification of the master cones.
Video 3: Obturation using Bioceramic sealer with GP
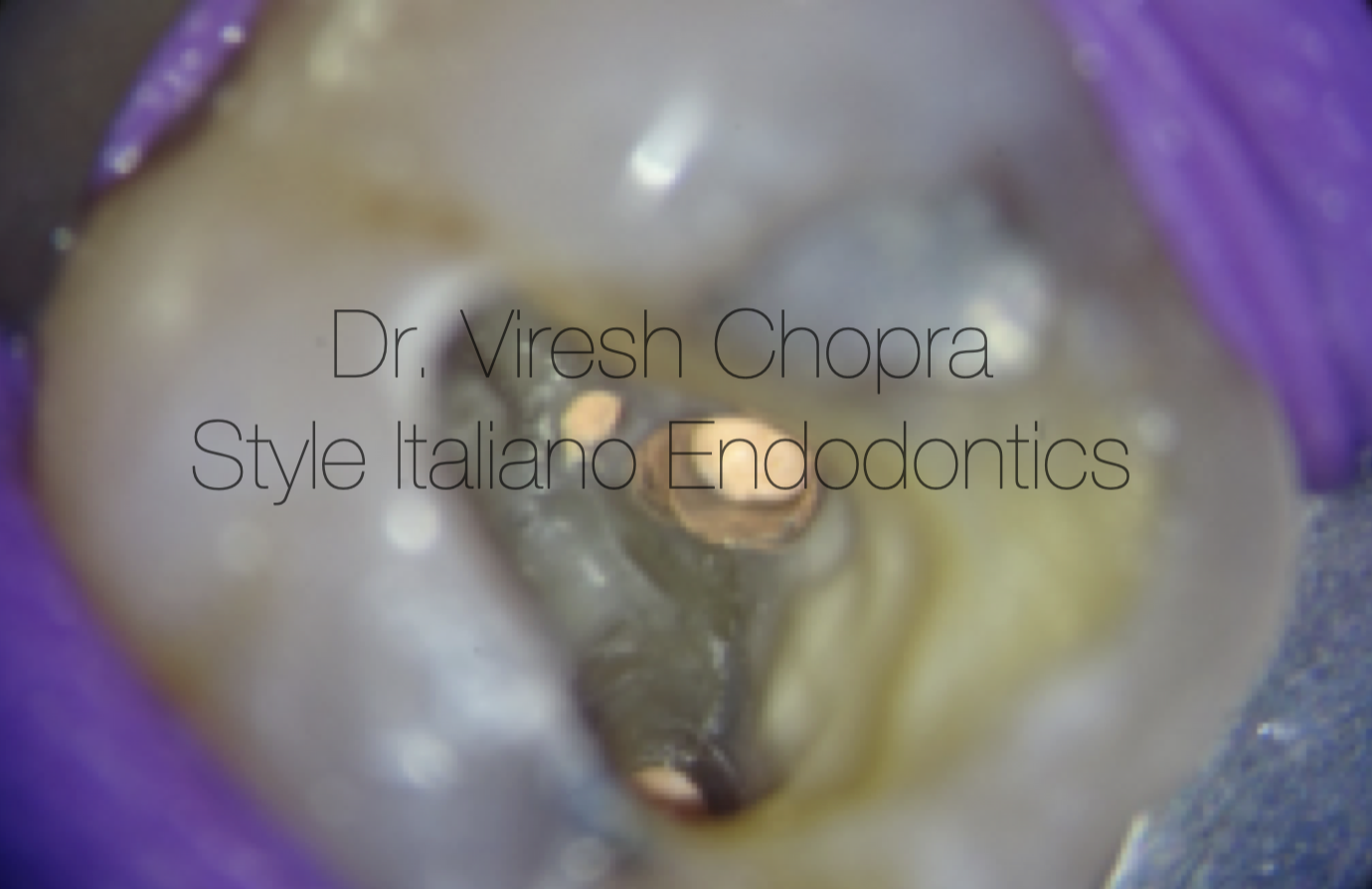
Fig. 5
Fig 4 Clinical picture showing Obturation of the root canal space.

Fig. 6
Fig 5: Radiograph immediately after the obturation.
Video 4: Clinical verification of Obturation
Conclusions
The pathway to triumphant endodontic success is paved with meticulous care and precision, with the root canal system serving as the canvas upon which the masterpiece of treatment is painted. A comprehensive approach encompasses four pivotal phases: thorough cleansing, precise shaping, effective disinfection, and the crowning achievement of a three-dimensional obturation.
The very foundation of this journey lies in the profound understanding that each canal within the intricate network demands meticulous attention. A failure to unearth all the hidden passages casts a shadow, leaving a haven for lingering microorganisms. This incomplete cleansing and shaping ritual inadvertently lay the groundwork for the eventual undoing of the initial root canal endeavor.
Indeed, the canvas of endodontic care is a delicate interplay of science and art, where success is the harmonious fusion of technique and comprehension. The traversal from the initial exploration to the final obdurate seal requires a mastery of all canal’s twists and turns, an intimate embrace of their idiosyncrasies.
In closing, the axiom is clear: to triumph over endodontic challenges is to embark on a journey where each canal, each juncture, and each microorganism is acknowledged and addressed. Only through this meticulous approach can the symphony of cleansing, shaping, disinfection, and obturation truly resonate, culminating in the crescendo of endodontic success.
Bibliography
Al-Haddad A, Che Ab Aziz ZA. Bioceramic-based root canal sealers: a review. International journal of biomaterials. 2016 May 3;2016.
Lee JK, Kwak SW, Ha JH, Lee W, Kim HC. Physicochemical properties of epoxy resin-based and bioceramic-based root canal sealers. Bioinorganic chemistry and applications. 2017 Oct;2017
Cardinali F, Camilleri J. A critical review of the material properties guiding the clinician’s choice of root canal sealers. Clinical Oral Investigations. 2023 Jul 17:1-9.
Camilleri J. Characterization and Properties of Bioceramic Materials for Endodontics. Bioceramic Materials in Clinical Endodontics. 2021:7-18.
Stewart GG. Gaining access to calcified canals. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 1995 Jun 1;79(6):764-8.