Selective root canal retreatment of an upper first molar: A 12 months CBCT-assessed outcome
04/09/2025
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Retreatment is a common procedure in Endodontics and has been shown to offer a favourable long-term outcome, with success rates ranging from 80% to 90%.
The conventional approach to retreating an infected tooth involves the removal of all restorations and obturating materials from all canals, followed by thorough disinfection of the endodontic space. After this phase, the tooth is then re-obturated and fully restored in its form and function.
This approach, has traditionally relied on conventional two-dimensional (2D) imaging and has not accounted for the fact that apical periodontitis does not necessarily affect all roots.
With the introduction of cone-beam computed tomography (CBCT), it is now possible to tailor the retreatment to selected root/s, making the procedure less invasive and more predictable by focusing only on roots associated with apical pathology.
This modern approach is referred to as Selective Root Retreatment, representing a more conservative strategy in managing persistent disease in root-filled teeth.
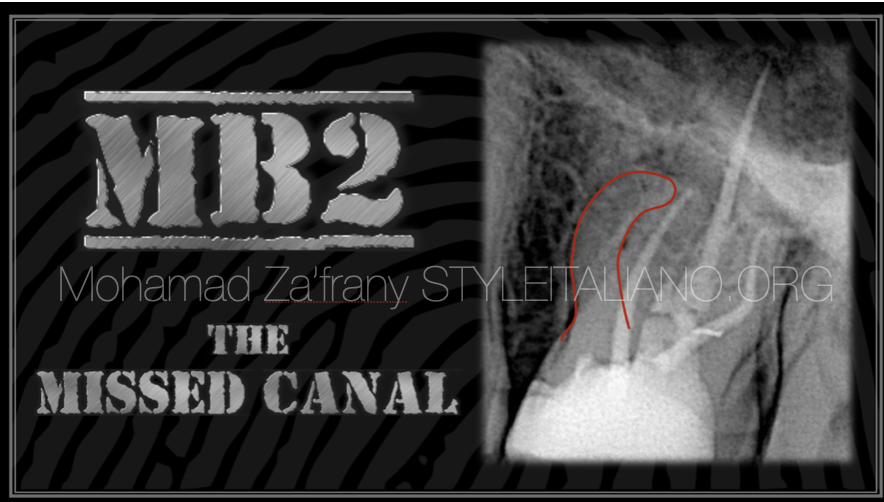
The case presented shows a 12-month follow-up of a selective root retreatment of an upper first molar, in which the MB2 canal had been previously missed.

Fig. 1
Pre-operative Radiograph of upper left first molar UL6
Symptomatic to pressure and buccal palpation.
A scantly condensed root filling was visible in the MB root however no clear evidence of apical lesion was noted.

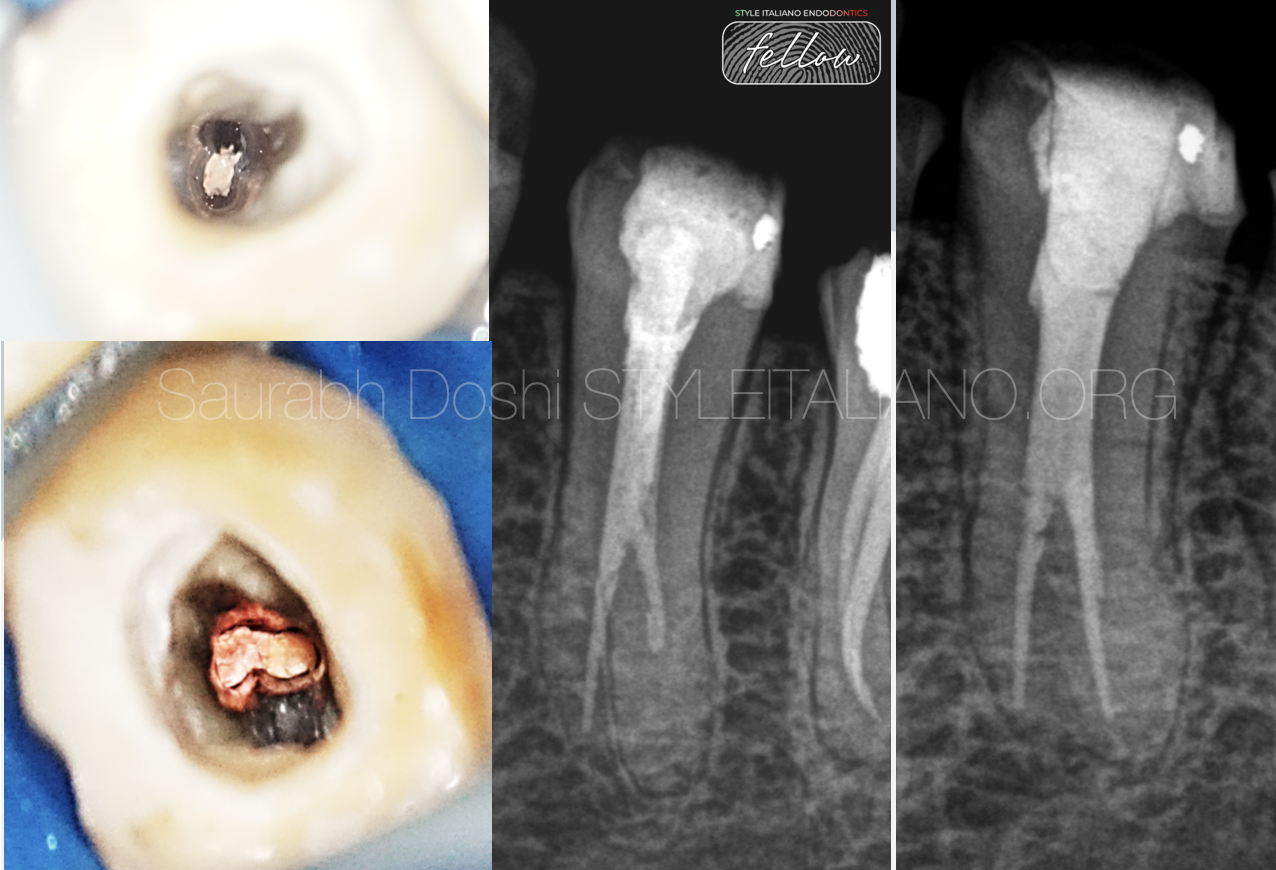
Fig. 2
Pre-operative sagittal view
The CBCT showed the presence of apical lesion with expansion of apical bone hence the symptoms.
A traceable missed canal was noted
A diagnosis of chronic apical periodontitis associated to a previously root treated tooth was confirmed.

Fig. 3
Pre-operative CBCT image axial view
The presence of a missed MB2 was now clear.
It was also noted complete separation of the MB root from the P and DB root that were joining in the same root trunk.
This was a favourable anatomic configuration which allowed the use of a Selective Root Re-treatment.

Fig. 4
Pre-operative CBCT coronal view of P and DB root
The absence of pathology on the P and DB root was confirmed

Fig. 5
Access cavity and selective re-treatment of MB root.
A conservative access cavity was performed and the MB2 was located, shaped and disinfected.
It was decided to re-treat the MB1 as well as part of the infected root.

Fig. 6
Obturation of the MB root and the presence of 2 independent canals

Fig. 7
Post operative radiograph
The MB root has been well filled using GP and Bioceramic sealer
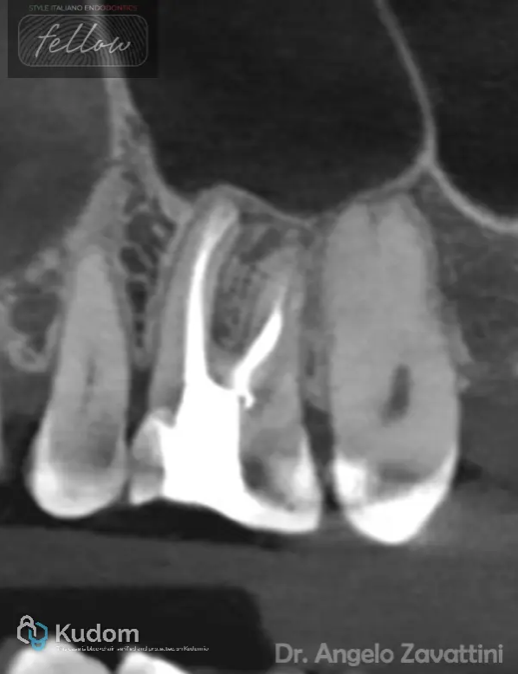
Fig. 8
CBCT 12 months post treatment
The sagittal view showed complete resolution of the apical pathology and evidence of two separated MB canals with independent apices.
The patient was completely asymptomatic with no evidence of persistent or new disease.
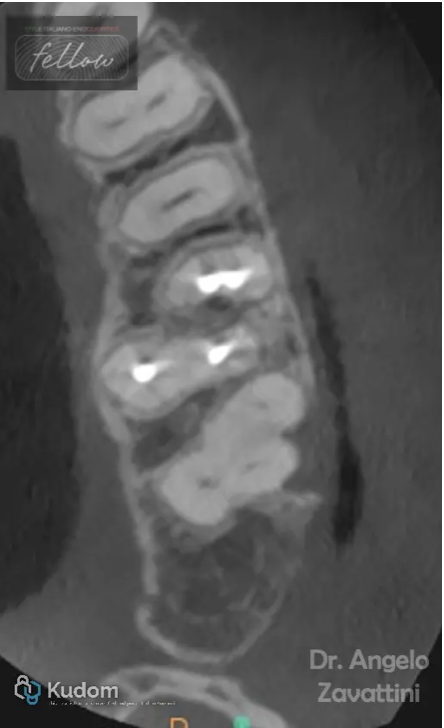
Fig. 9
CBCT 12 months post treatment
Axial view showed well obturated MB root and no evidence of new lesion
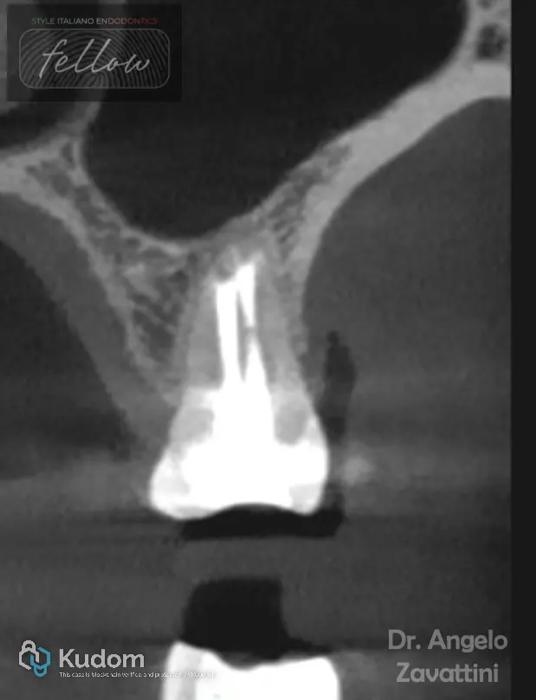
Fig. 10
CBCT 12 months post treatment
Coronal view showed the presence of well obturated MB1 and MB2 to apex with complete resolution of apical lesion

Fig. 11
About the author;
Dr.Angelo Zavattini graduated with Honours from the University of Rome Tor Vergata in 2012.
He has started his career as a general dentist in Rome focusing on Restorative Dentistry and Endodontics.
Upon moving to London in 2013, he undertook further training in Restorative Dentistry, Oral surgery, and Endodontics, eventually earning Membership to the Faculty of Dental Surgery at the Royal College of Surgeons of England.
He obtained a PhD in Dental Material in 2017 from the University of Rome Tor Vergata and since than he has published numerous scientific papers in international journals.
He is actively involved in clinical and in-vitro research with a focus on bioactive materials in Endodontics.
He has completed a comprehensive three-year full-time academic clinical training program in Endodontics at Guy's Hospital, King's College London, and obtained specialised membership in Endodontics from the Royal College of Surgeons of Edinburgh.
Dr.Angelo Zavattini is a registered Specialist in Endodontics and a part time Senior Lecturer at Queen Mary University of London teaching at the postgraduate program in Endodontics.
Conclusions
The decision to selectively re-treat one or more roots must be based on a thorough assessment of the tooth presenting with persistent disease. This includes a pre-operative CBCT assessment, clinical examination, and evaluation of the existing restoration.
In the author’s opinion, intraoperative exploration of the status of the previously filled canal at the orifice level is also of significant importance as sings of leakage may be present.
A Selective root treatment not only has the advantage of a more conservative access cavity directed to the affected root, more preservation of tooth structure and reduced time and cost but also minimize procedural errors and iatrogenic mishaps.
When assessing the outcome of surgical or non-surgical endodontic interventions, it is important to acknowledge the limitations of conventional radiographs.
In this case, due to significant anatomical noise, it was not possible to accurately identify the pre-operative lesion or subsequently evaluate its resolution.
The CBCT scan proved to be valuable for diagnosis, treatment planning, and technical execution in this case.
However, the routine use of CBCT for outcome evaluation remains a topic of ongoing debate. In clinical practice, the decision to employ a 3D imaging exam should be carefully considered, balancing the diagnostic benefits with the principle of using the lowest radiation dose reasonably achievable ( ALARA).
Bibliography
Nudera WJ. Selective Root Retreatment: A Novel Approach. J Endod. 2015 Aug;41(8):1382-8. doi: 10.1016/j.joen.2015.02.035. Epub 2015 Apr 21. PMID: 25906919.
Gorni FG, Gagliani MM. The outcome of endodontic retreatment: a 2-yr follow-up. J Endod. 2004 Jan;30(1):1-4. doi: 10.1097/00004770-200401000-00001. PMID: 14760899.
Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009 Jul;35(7):930-7. doi: 10.1016/j.joen.2009.04.023. PMID: 19567310.
Brochado Martins JF, Guerreiro Viegas O, Cristescu R, Diogo P, Shemesh H. Outcome of selective root canal retreatment-A retrospective study. Int Endod J. 2023 Mar;56(3):345-355. doi: 10.1111/iej.13871. Epub 2022 Nov 27. PMID: 36403111; PMCID: PMC10100215.