Root perforations: from breakdown to breakthrough
19/07/2023
Fellow
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
In retreatments, one of real endodontic challenges comes when disassembly is complete and what remains is a root canal system that has been perforated.
What is the critical thinking required to solve such impediment to success?
In this article, I am describing the management of a root perforation using absorbable collagen membrane as an internal matrix and MTA to seal the perforation site.
Perforation is an artificial communication between the root canal system and the external tooth surface (American Association of Endodontists Glossary, 2016). Root perforation complicates the treatment and deprives the prognosis if not properly managed.
Some factors may predispose to operative procedural accident or errors.The presence of pulp stones and root canal calcification are factors that may make root canal access difficult, and predispose to root perforation. (Esterla et al, 2017).
Root perforation might result in a serious complication which needs to be diagnosed early and treated immediately and appropriately (Seltzer et al, 1970 ). The consequences of root perforation may result in an inflammatory response associated with periodontal tissue and alveolar bone destruction. Depending on the severity of the injury, and possible chronic inflammatory reaction, it may cause the development of granulomatous tissue, proliferation of the epithelium, and, eventually, the development of a periodontal pocket ( Bueno et al, 2011).

Fig. 1
A 22 year old male has visited my office complaining of discolouration in the upper left central incisor and a swelling in the soft tissue surrounding this tooth. He mentioned that he is under orthodontic treatment and his orthodontist has performed a root canal treatment on this tooth a month ago, and is now suggesting a retro surgery to treat the persistent localised swelling in this area.
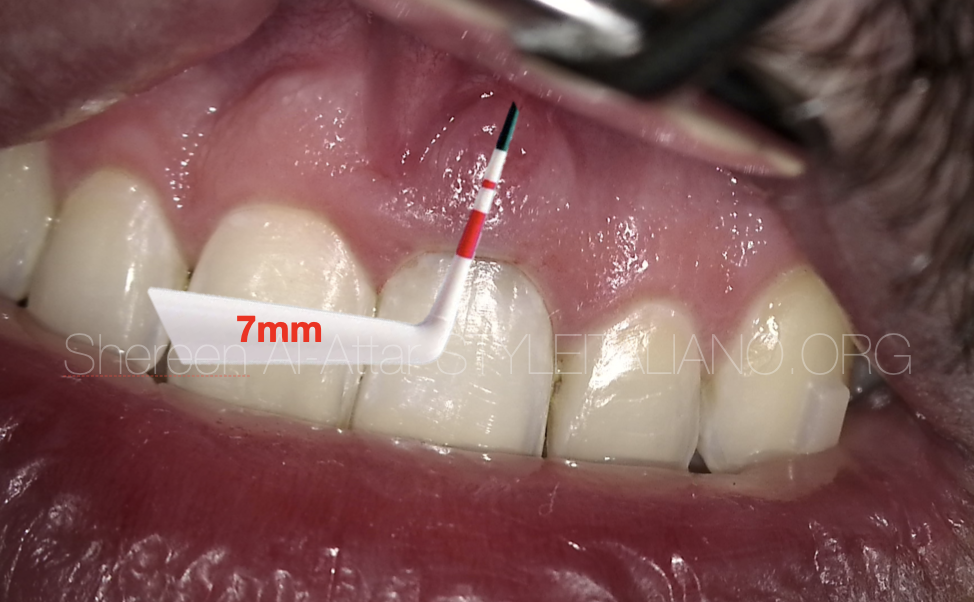
Fig. 2
After clinical examination, a periodontal pocket was present buccally (7mm) and a sinus tract was observed buccally at mid-root level.
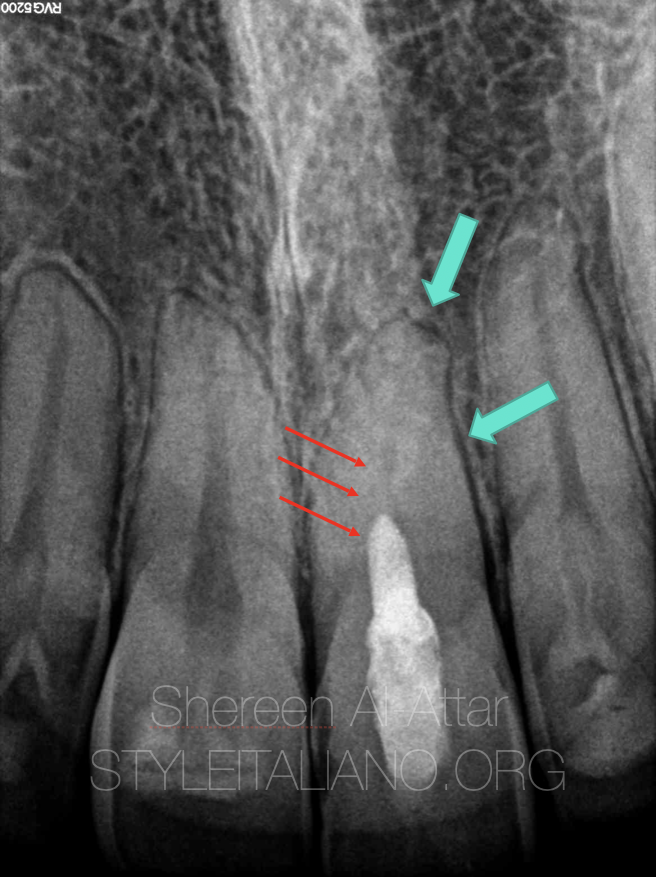
Fig. 3
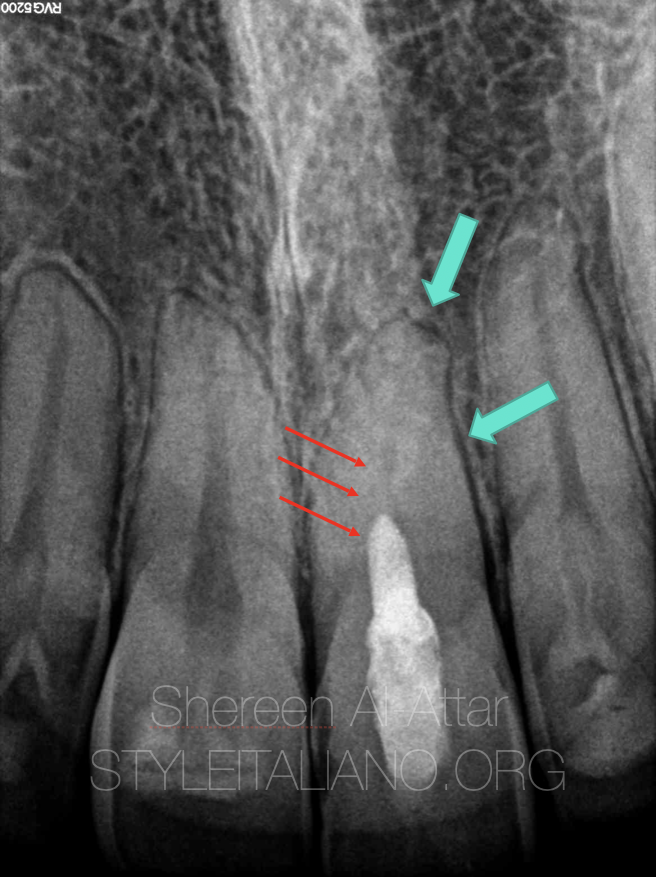
An intraoral periapical radiograph showed a previously treated root canal on tooth 21. The root canal filling was incomplete and seemed to be not following the original root canal path. A periapical lesion was evident at the apex and widened periodontal ligament space was clearly noticed.
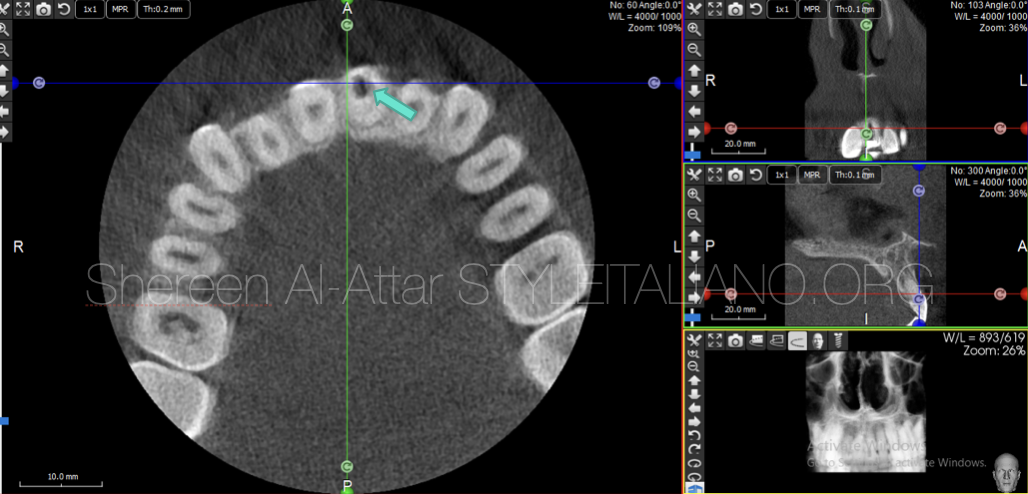
Fig. 4
CBCT radiography revealed the off-centred access created in the coronal third of the root
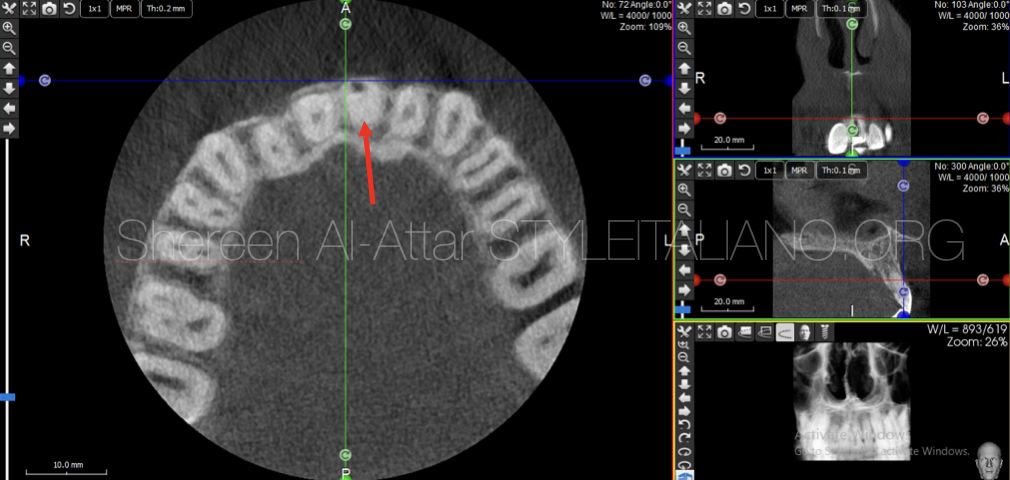
Fig. 5
Moreover, CBCT sections have revealed the presence of a perforation in the buccal wall at mid root level that is associated with significant bone loss as well as interrupted buccal plate starting at the level of the perforation.
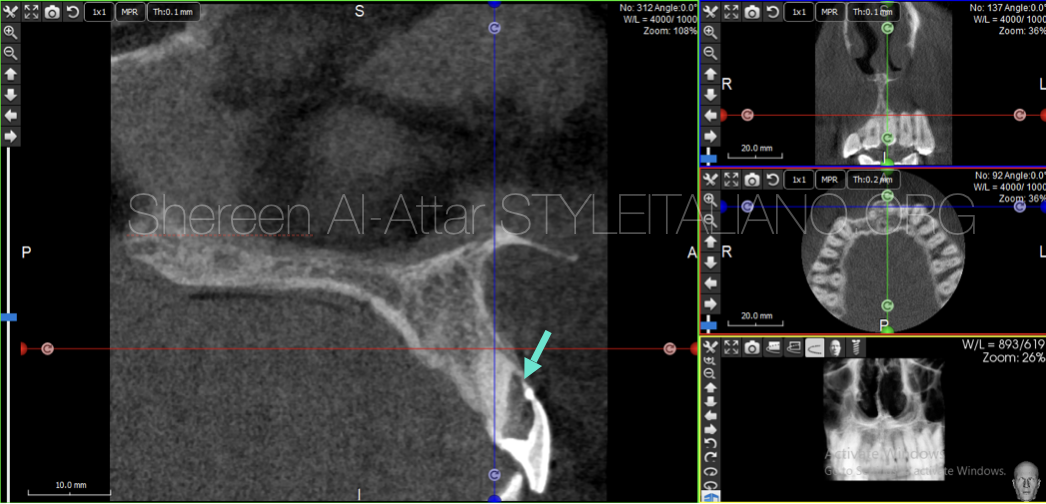
Fig. 6
The root canal of this tooth was found to be completely calcified (arrow).
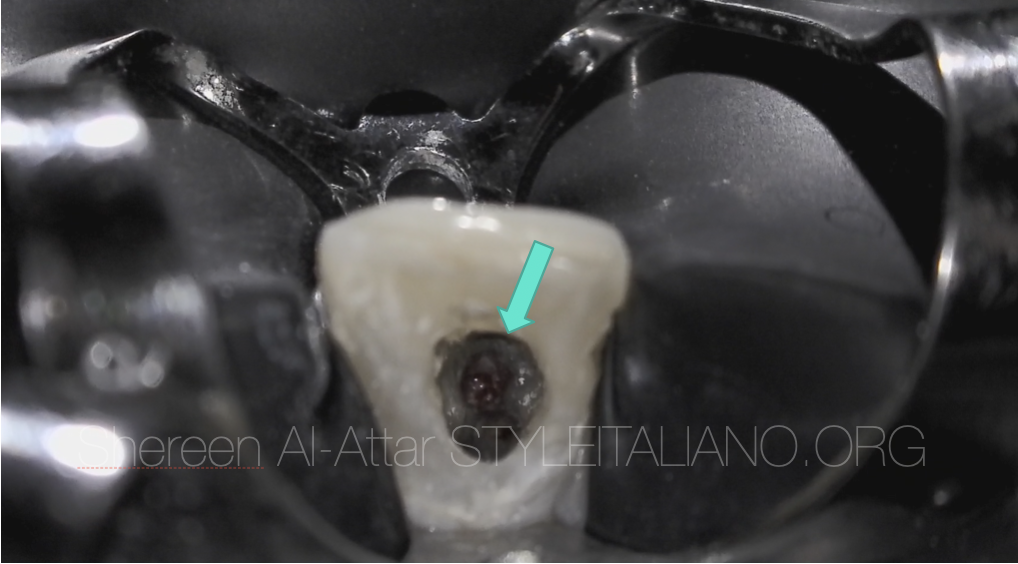
Fig. 7
The main problems with this perforation were (1) the angle of access is not in alignment with the angle of incidence; (2) bleeding; and (3) difficult to compact due to lack of a backstop. Therefore, a retreatment was suggested to remove the old filling in the false route followed by sealing the perforation using resorbable collagen membrane as carrier to provide complete haemostasis, to act as a controlled barrier, and to pack the MTA against to seal the perforation site.
The previous Gutta percha was removed, remaining tooth structure was assessed and the perforation site was localised precisely under microscope.

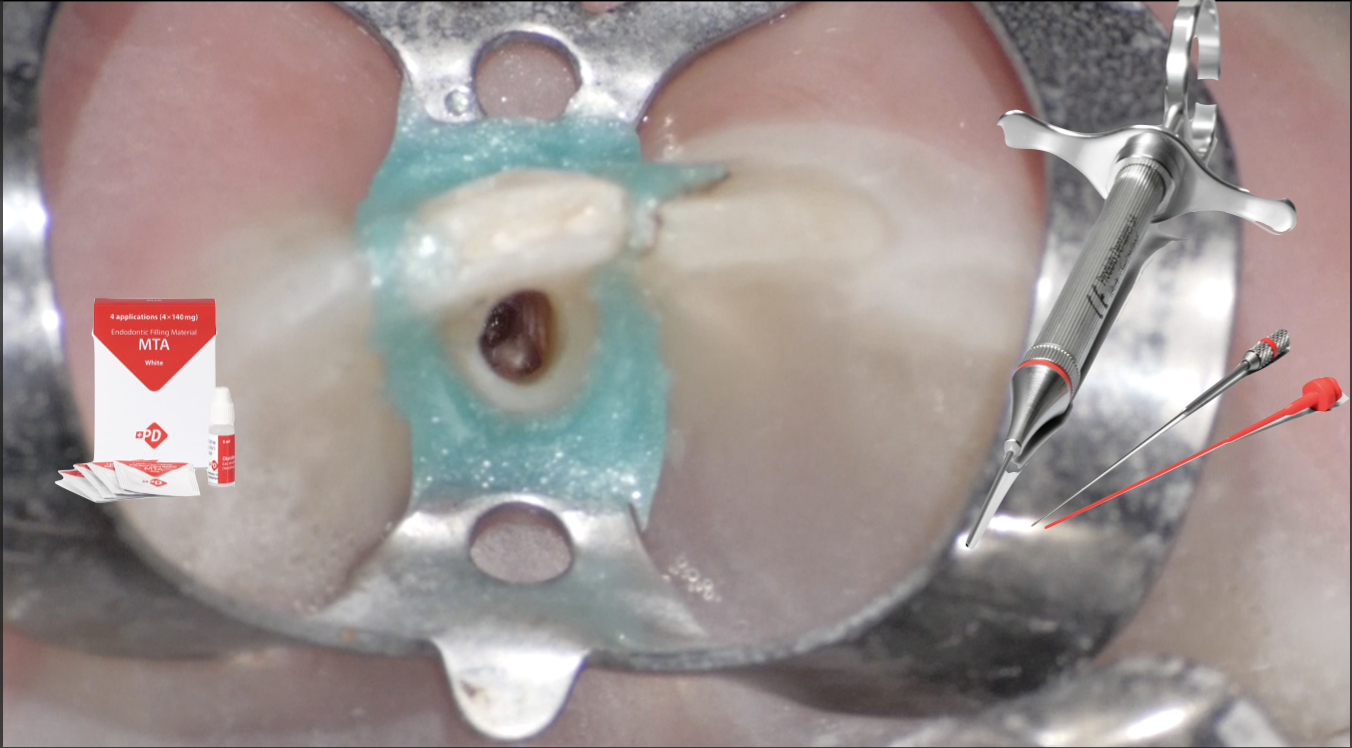
Fig. 8
Prior to MTA (ProRoot MTA, Densply) , a piece of resorbable CollaCote (Sulzer/Zimmer Dental; Carlsbad, California, USA), was cut to appropriate size and carried into the access cavity.
The material was incrementally placed through the tooth and into the osseous defect until a solid barrier is established at the cavo surface of the root.
This membrane was progressively placed into the chamber with Machtou plugger (size 1/2) and firmly pressed through the perforation defect. Hemostasis was achieved in five minutes.
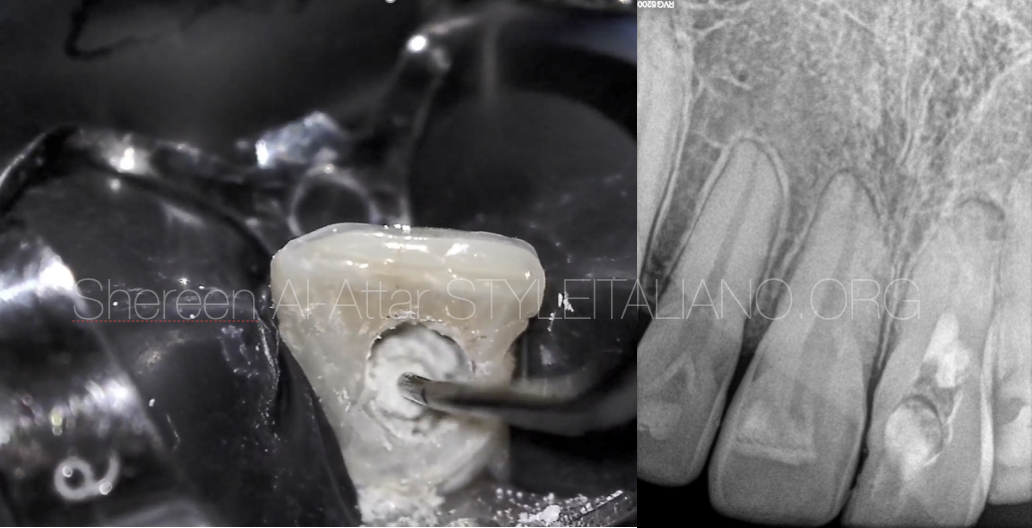
Fig. 9
MTA was then compacted against the collagen barrier at the perforation site. After setting, the rest of the canal was filled with gutta percha using back fill obturator.

Fig. 10
After one month the patient was recalled and was asymptomatic.

Fig. 11
At the 3-month recall, radiographic findings showed adequate sealing of the perforation region

Fig. 12
At the 6-month recall, clinical examinations showed that the tooth had no pain and no response to percussion, palpation and there were no probing depths and adequate clinical function.

Fig. 13
About the author:
Dr Shereen Alattar (DDS, MSc) has graduated from Saint Joseph University in Beirut, Lebanon, where she received her Master’s Degrees in the specialisation of Endodontics. She works in a referral-based practice limited to endodontics in Amman, Jordan.
She is a fellow member in Style Italiano Endodontic Group and an active member in the Jordanian Scientific Committee of the Jordanian Dental Association and in the Jordanian endodontic society
Conclusions
The purpose of this article is to present a case report in which absorbable collagen membrane was used as an internal matrix, and MTA was used to seal the perforation. Immediate repair with good repair material and trying to be minimally invasive ensures successful outcome despite complexity of the condition.
Furthermore, like all endodontic challenges, perforations are also opportunities. They are opportunities for all of us to master our clinical artistry further and take such breakdowns and turn them into successful breakthroughs.
Bibliography
- American Association of Endodontists. Glossary of endodontic terms. 9th ed. Chicago: American Association of Endodontists; 2016.
- Seltzer S, Sinai I, August D. Periodontal effects of root perforations before and during endodontic procedures. J Dent Res. 1970 Mar-Apr;49(2):332-9.
- Bueno MR, Estrela C, De Figueiredo JA, Azevedo BC. Map-reading strategy to diagnose root perforations near metallic intracanal posts by using cone beam computed tomography. J Endod. 2011 Jan;37(1):85-90.
- Estrela C, Pécora JD, Estrela CRA, Guedes OA, Silva BS, Soares CJ et al. Common operative procedural errors and clinical factors associated with root canal treatment. Braz Dent J. 2017 Jan-Apr;28(2):179-90.