Root perforation management
05/09/2020
Bartłomiej Karaś
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
This article is a short summary and a guideline for all dentists who want to manage different types of root perforation in an easy and predictable way. This article will emphasize the importance of the diagnosis and accessories that will be helpful during the treatment.
Root perforations are one of the common complications that can occur in primary treatment or retreatment cases. Of course it would be better avoiding this kind of complication, on the other hand a good management of this kind of cases can improve our success rate and will let us to treat more complex cases.
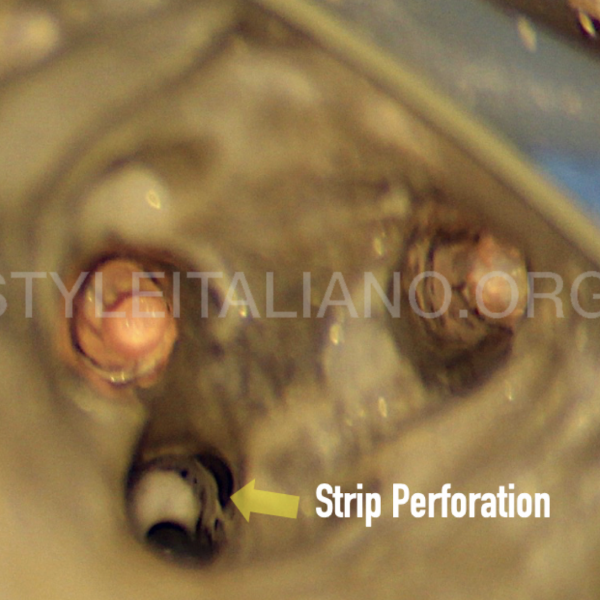
Perforation is a kind of connection between two areas that, in normal conditions, are not connected. It can be performed during different stages of the root canal treatment, from the access cavity creation to the shaping protocol. The instruments that are able to cause a perforation are several: drills, ultrasonic tips, Gates Glidden burs, hand files or rotary/reciprocating files.
In case of perforation, there are three most important factors that have to be estimated for the correct treatment plan.

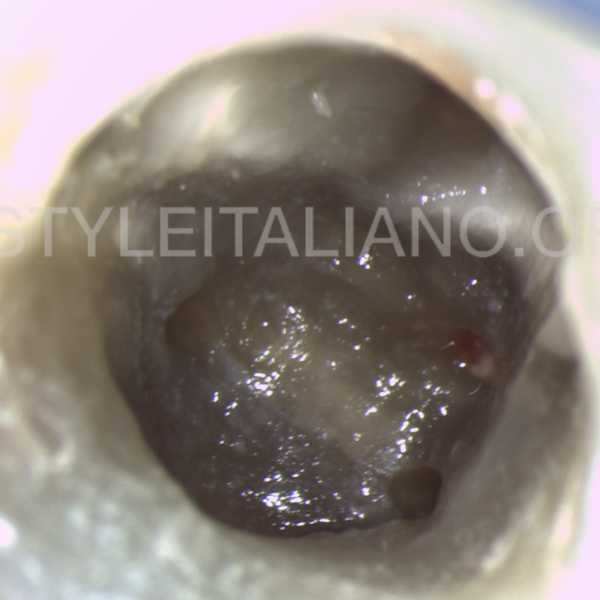
Fig. 1
Factors to be evaluated

Fig. 2
Time and lesion are connected in a certain way. In many cases we don’t know where did the perforation was performed, but in a certain way we can make a prognosis during the radiological examination.
In many cases, when the perforation is infected, the longer the time it exist, the bigger the lesion around the perforation will be. If the perforation is an old one but there is no lesion in the bone it means that it should be not infected, which is a good prognostic factor. The more recent the perforation is, the better the prognosis is.
The presence and the type of lesion are also important. If there is no lesion it means that there is no infection in the root canal system or the perforation was made recently. If the lesion is present we have to be aware that we are dealing with the infection in the root canal system. If the endo-perio type of lesion appears, we need to remember that the extraradicular biofilm can be present, so the periodontal treatment can be required.
The prognosis is directly connected with mentioned factors:
-
- no lesion - the best prognosis
- lesion is present - moderate prognosis
- endo-perio lesion - unfavorable prognosis

Fig. 3
The place and size of the perforation is mostly related with the biomechanical properties of the tooth. The prognosis is bad when the perforation is closer to the furcation and its size is big.
There are some available researches and observations which can give us some important data on this topic. Gorni et al. performed a long term observations (8 years and more) of 110 patients in a prospective study. On of the most important data analyzed by this article is the the size of the perforation: with perforations whose size is
0-1mm - prognosis is the best
2-3mm - failures were present
3mm and more - percentage of the failures was highest.
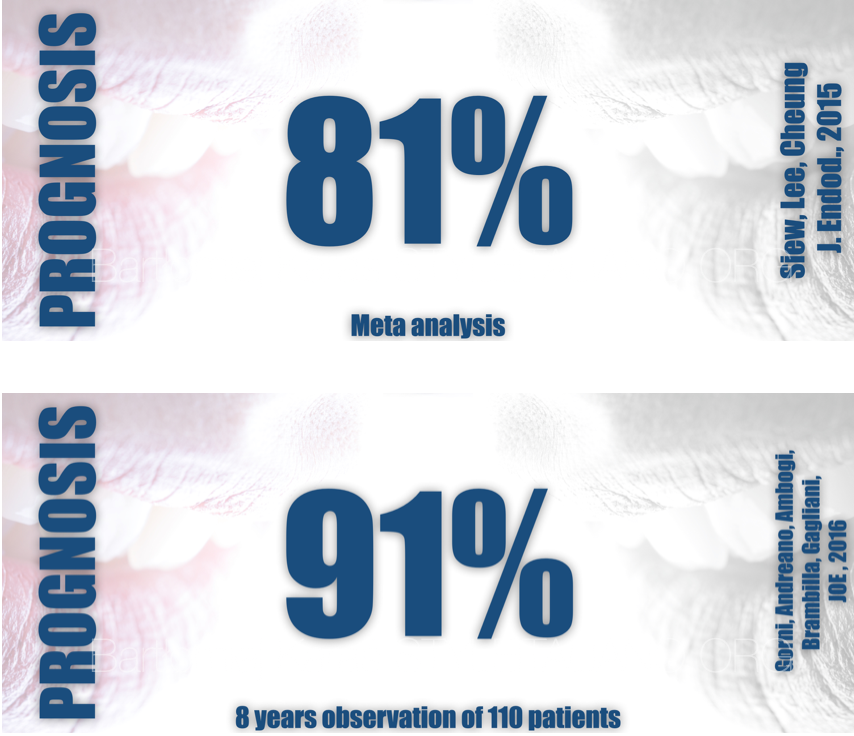
Fig. 4
According to some available researches, nowadays the long term success becomes a standard for endodontists. Of course we need to remember that in all articles which show the high success rate there are some standards such as working with the surgical microscope, rubber dam, MTA/Bioceramic materials, proper irrigation protocol. These are factors will help the operators to achieve high success rates and good long term outcomes.
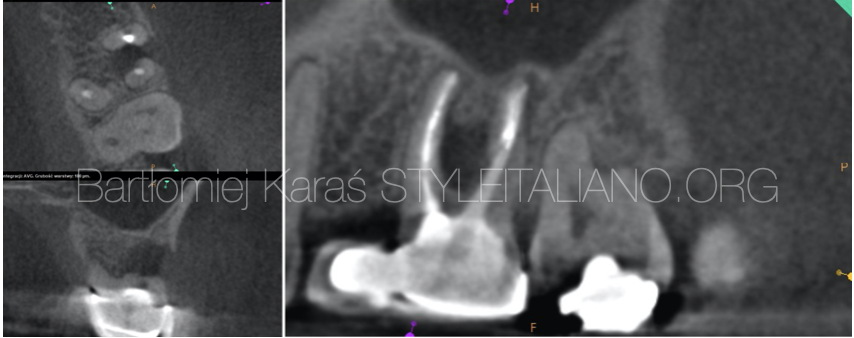
Fig. 5
Patient was referred to my office because she felt pain and the fistula was present.
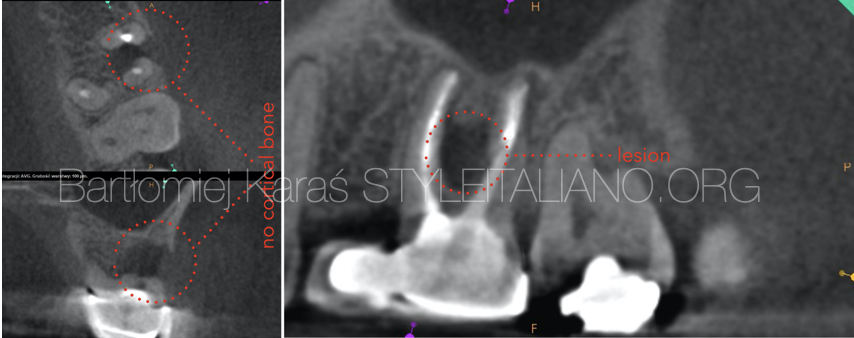
Fig. 6
During the radiological examination, the CBCT image revealed that there was a large lesion in the furcal area which damaged the crestal bone. The most probable reason of this lesion is the perforation, which I believe was performed during the post space preparation.
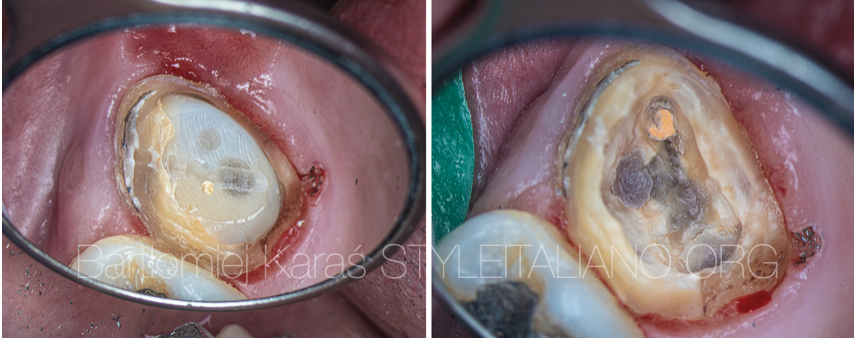
Fig. 7
View of the tooth after crown removal on the left and composite removal on the right.

Fig. 8
View of the chamber after the temporary restoration was done and the removal of the fiber post from the palatal canal.

Fig. 9
View during the removal of the fiber posts and after removal of the guttapercha.

Fig. 10
View of the MTA-carrier and the sealed perforation.

Fig. 11
The view of the chamber after obturation with warm gutta-percha and the periapical x-ray.
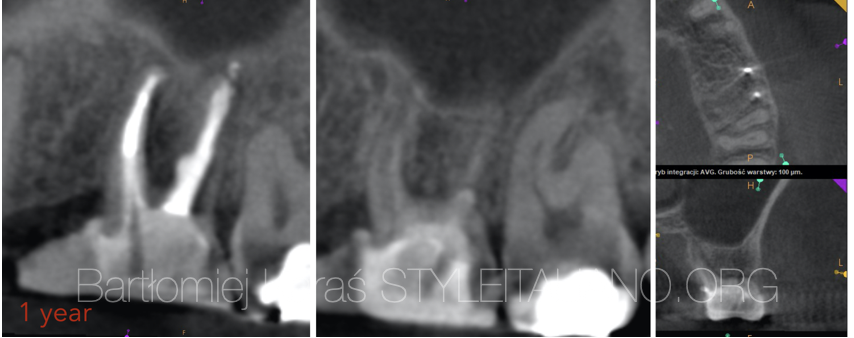
Fig. 12
This is the recall image after 12 months. There are no symptoms and no visible lesions.
Conclusions
The main advantage of modern endodontics is the possibility of saving the teeth that were hopeless 20-30 years ago. One of the biggest step was done in the management of the perforations. Thanks to the research of Prof. Torabinejad we can seal the perforations and have very satisfying long term resulst.
As it was shown in the article, we need to know the criteria to estimate the prognosis. The most important factors for prognosis are the size of the perforation, location of the perforation and presence and type of the lesion (if present). We also need to have a good communication with the patient because this type of cases are difficult and the patient has to understand this situation. We also need some accessories like proper tools and materials to make our treatment easier and more comfortable for us.
Bibliography
Gorni FG, Andreano A, Ambrogi F, Brambilla E, Gagliani M. Patient and Clinical Characteristics Associated with Primary Healing of Iatrogenic Perforations after Root Canal Treatment: Results of a Long-term Italian Study. J Endod. 2016;42(2):211‐215.
Tsesis I., Fuss Z. (2006). Diagnosis and treatment of accidental root perforations. Endodontic Topics. 13. 95 - 107. 10.1111/j.1601-1546.2006.00213.x.
Estrela C, Decurcio D, Rossi-Fedele G, Silva J, Guedes O, Borges ÁH. Root perforations: a review of diagnosis, prognosis and materials. Braz. oral res. Epub Oct 18, 2018.
Fuss, Z., Trope,M. Root perforations: classification and treatment choices based on prognostic factors. Endod Dent Traumatol 1996, 12:255 264
Siew K, Lee AH, Cheung GS. Treatment Outcome of Repaired Root Perforation: A Systematic Review and Meta-analysis. J Endod. 2015;41(11):1795‐1804. doi:10.1016/j.joen.2015.07.007