Mysterious pathology, fascinating anatomy & healing- a case of NSRCT of tooth 44
05/05/2024
Garima Poddar
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
With an endodontic treatment, we aim at treating patient’s pain, inflammation, swelling, aim for healing and to prevent recontamination after the treatment. After careful examination and diagnosis, a treatment plan should be made for the patient which would be predictable.
Case report
Patient information
Age: 25
Gender: Male
Medical history: Non contributory.
Tooth identification: Mandibular right first premolar (tooth number 44).
Chief complaint:
- Patient Complaint of pain and a draining sinus, in relation with tooth number 44.
- Patient had earlier visited multiple dentists ( about 6 months prior to getting referred to us) with complaint of intermittent pain in mandibular right posterior region. During those visits, dentists could not diagnose the tooth related problem. The case was referred to our office after draining sinus developed in relation with 44.

Fig. 1
Intraoral examination-
On clinical examination, the following observations were made-
A draining sinus was observed buccally in relation with tooth number 44.
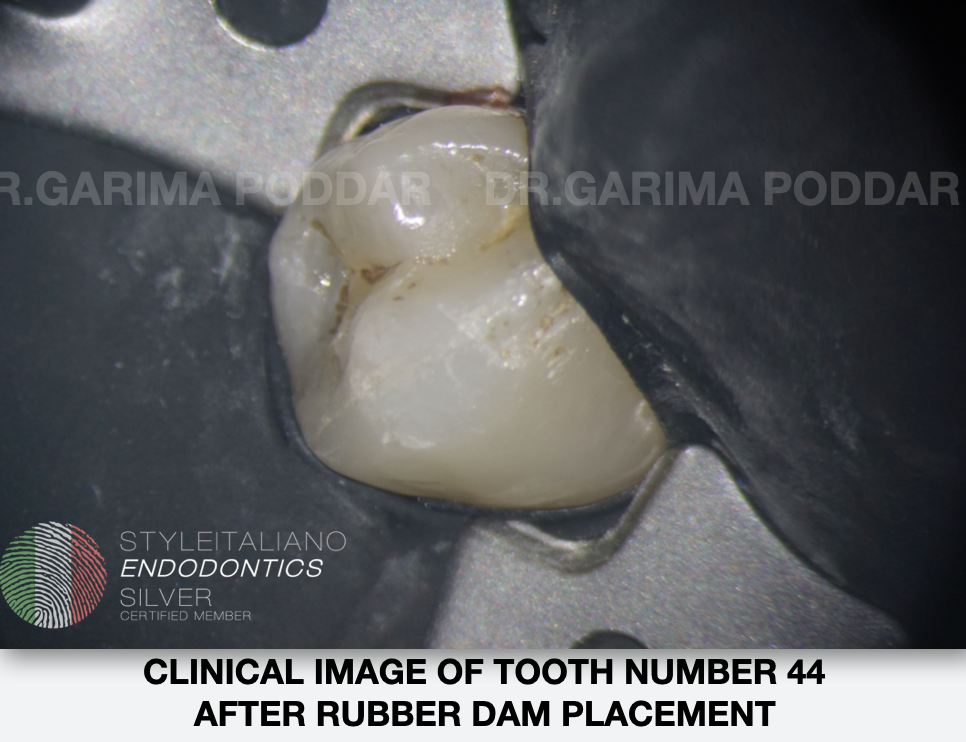
Fig. 2
There was no caries found on the tooth surface of tooth number 44 on any aspect. Only some stains could be appreciated in the fissures and grooves.

Fig. 3
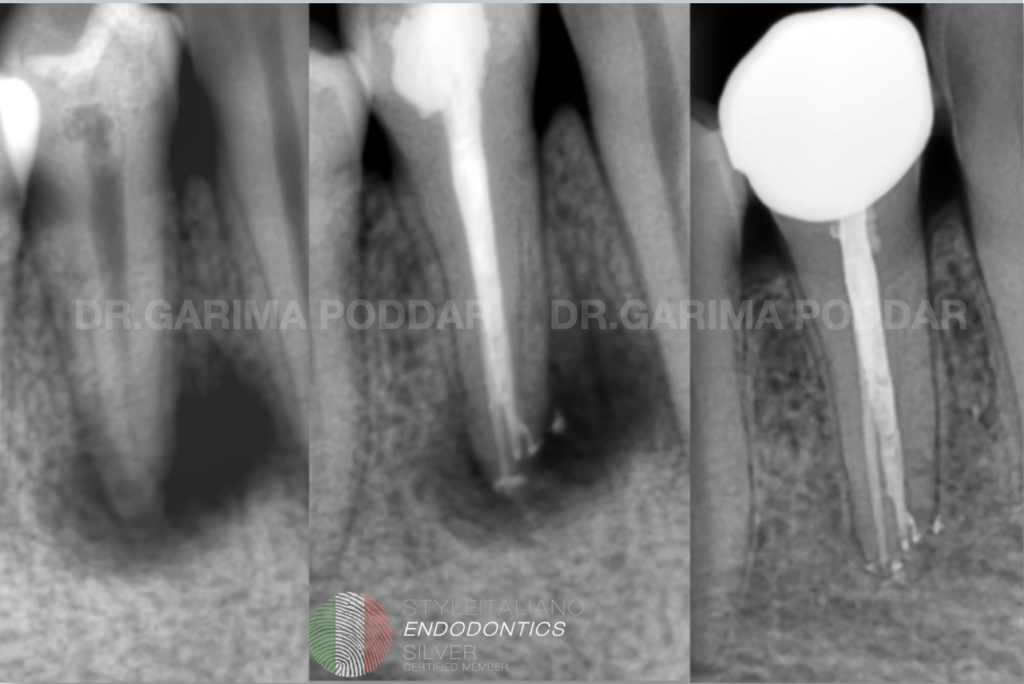
Radiographic examination-
Pre-operative intraoral radiograph showed the following-
Straight view radiograph-
- A large peri-apical radiolucent lesion could be seen with respect to tooth number 44.
- In the deeper layer of the tooth, a radiolucency was observed.

Fig. 4
Angulated view radiograph-
On another pre-operative radiograph which was made with buccal tube shift technique, the following details were observed-
- A circular, radiolucent lesion was seen in the dentinal layer approaching pulp.
- Another whitish circular lesion was seen in dentin.
- Mid- root split of one canal into two was seen. The root canal anatomy appeared to be 1-2 on the radiograph.
- Periapical radiolucency was evidently present.
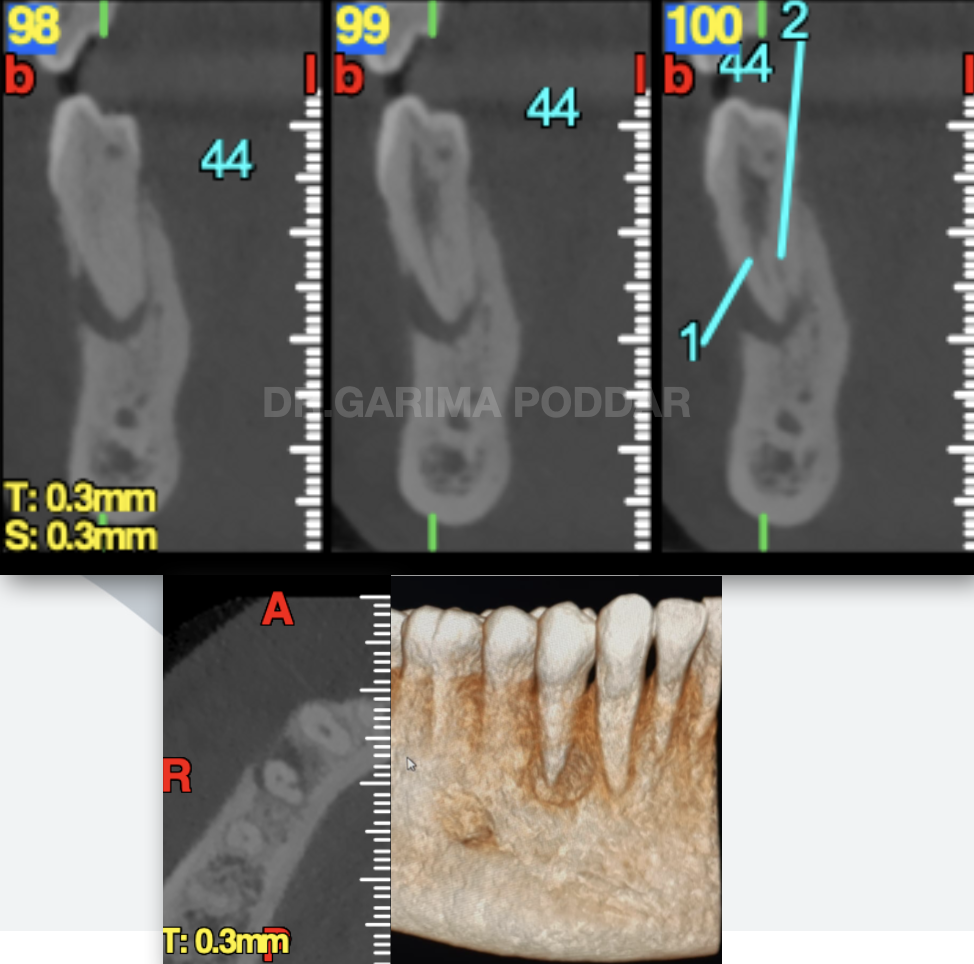
Fig. 5
Pre-operative CBCT
The following details could be confirmed with the help of cbct imaging-
- Peri-apical radiolucency was observed with 44.
- 1-2 canal configuration was confirmed.
- Radiolucent circular area in deeper layer of the tooth was seen. The radiolucency could be indicative of external resorption
- Bone resorption seen on bucco mesial side. Buccal cortical plate appeared to be disrupted in relation with 44.
Treatment Plan-
1. Non surgical RCT.
2. Periodic follow ups
3. Patient was informed that in case healing is not initiated, then surgery could be thought of as an alternative.

Fig. 6
Preliminary procedure-
- Local anesthesia- Inferior alveolar nerve block was given using 2% lignocaine with adrenaline injection.
- Rubber dam isolation- tooth number 44 was isolated using rubber dam isolation.
- Magnification- The root canal treatment was done under a dental operating microscope for better visualization. 25X and 16X magnification was used during the treatment.
- Access preparation was done. A conservative approach was adopted for the same.
Working length was determined using an electronic apex locator and was confirmed with radiographs.
Shaping protocol:
Coronal flaring was done.

Fig. 7
8k, 10k file was used to instrument the canal till in became loose in the canals.
Glide path preparation was done, then the canals were shaped up till 25-06%.
Calcium hydroxide dressing was placed in canals and temporary dressing was given.
Patient was recalled after one week.
On next visit, it was observed that draining sinus had healed and pain had subsided.
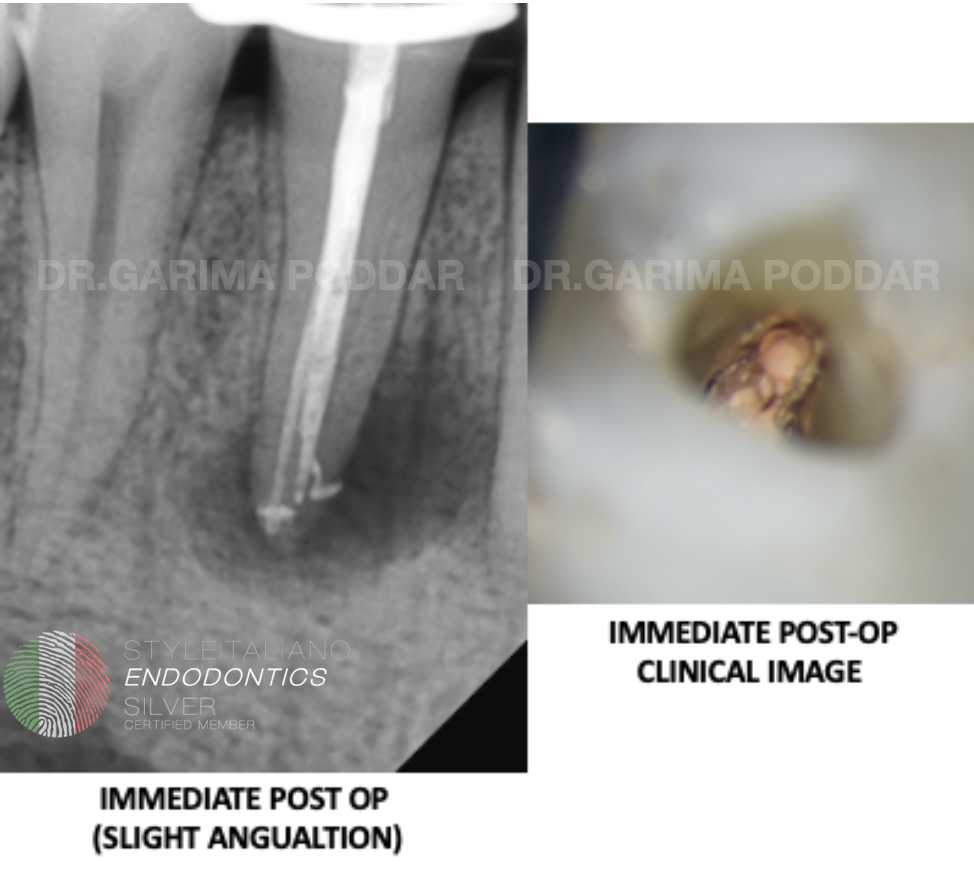
Fig. 8
Irrigation protocol-
Throughout shaping, 5.25% sodium hypochlorite was used after each file. Side vented 30 gauge needles were used for irrigation.
After shaping, the following protocol in each canal, was used for irrigation and activation of irrigants-
1) 17% EDTA – 1ml per canal was used which was activated with an ultrasonic activator.
2) Distilled water used to flush the canals.
3) 5.25 % sodium hypochlorite was then injected in the canal, intracanal heating was done and was ultrasonically activated.
4) Distilled water.
Obturation protocol:
Cone fit intra oral radiograph was made.
Canals were dried with paper points.

Fig. 9
Canals were obturated with warm vertical compaction technique
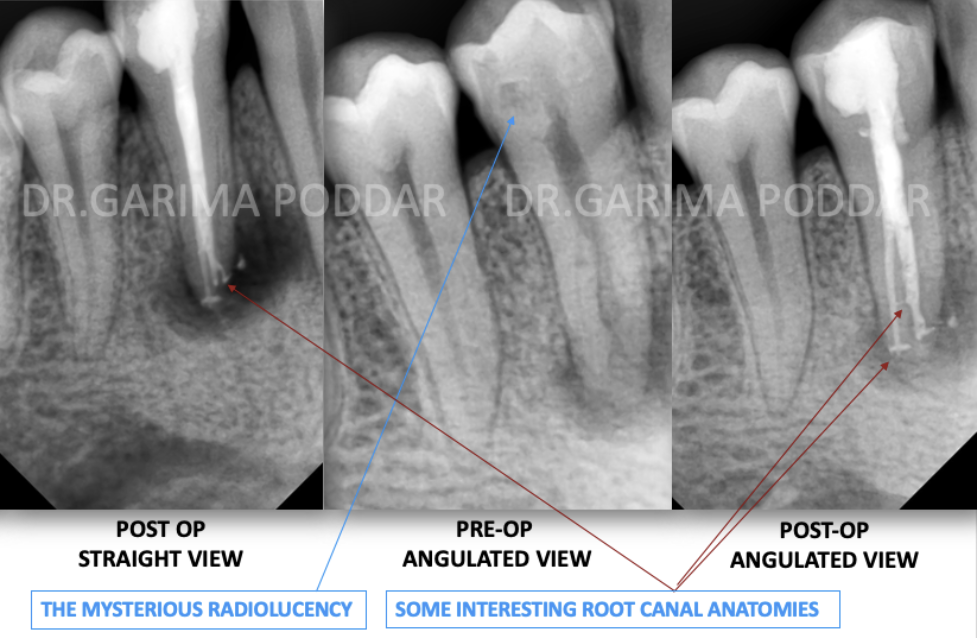
Fig. 10
As a result of thorough irrigation and tri dimensional obturation, a lateral canal and apical delta was also obturated.
An anastomosis was also seen in between the two splits on post operative radiograph.

Fig. 11
At different angulations of the radiograph, different anatomy could be appreciated to on the post operative intra oral radiographs.
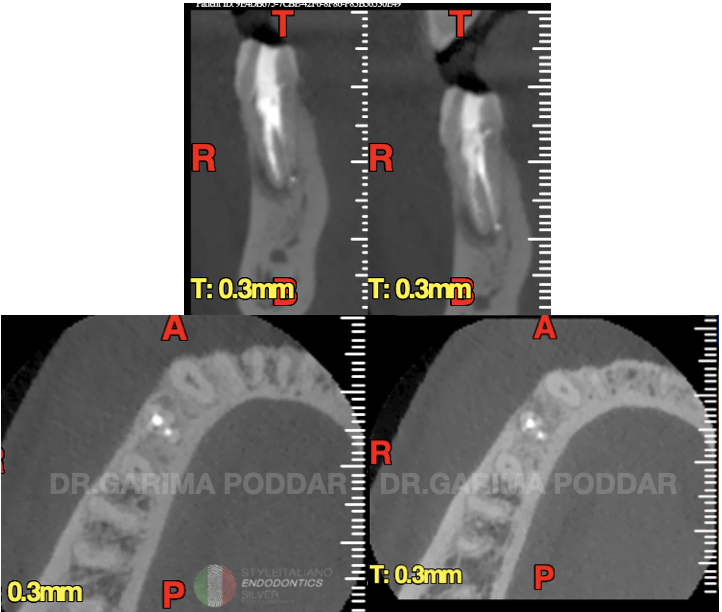
Fig. 12
Follow up
Follow up CBCT showed ongoing healing.
It was evident on the CBCT, that the peri-apical radiolucency had reduced considerably.

Fig. 13
It could be appreciated on immediate post-op radiographs, that the shaping and obturation was conservative in nature. Care was taken not to remove extra dentin of the root canal walls.
At the same time, irrigation protocol was not compromised. 30 gauge side vented irrigation needles were used, which could reach till apical third of the canals and thus irrigation solutions could perform its action properly.

Fig. 14
3 Month follow up-
3 month control, showed reduction in the size of the peri-apical radiolucency, indicative of ongoing healing process.

Fig. 15
The referring dentist, did the prosthetic rehabilitation of the tooth with a zirconia full coverage crown.
6 months follow up-
It showed further healing of the lesion.
The patient and tooth was absolutely symptom free.
1 and a half year follow up-
The tooth appeared to have completely healed at this time.
Conclusions
For preforming a predictable root canal treatment, it’s essential to diagnose the case correctly and plan the treatment which would lead us towards success. The operator should have sound knowledge of root canal anatomy, skill to manage anatomies like splits and curvatures, proper cleaning, shaping and obturation. A good apical seal as well as coronal seal, is very important part of a root canal treatment. Good irrigation and activation plays a vital role in such cases being treated non surgically. Use of magnification and precise tools also plays an important role in making the treatment precise and more predictable. Proper modification of access opening is essential for both ease of carrying out the steps of root canal treatment procedure, and also for successful treatment outcome. When each step of the treatment procedure is performed following the required protocols, treatment outcome is most likely to be successful.
Bibliography
Zillich R, Dowson J. Root canal morphology of mandibular first and second premolars. Oral Surg Oral Med Oral Pathol. 1973;36:738–44.
Vertucci FJ. Root canal morphology of mandibular premolars. J Am Dent Assoc. 1978;97:47–50.
Velmurugan N, Sandhya R. Root canal morphology of mandibular first premolar in Indian population: A laboratory study. Int Endod J. 2009;42:54–8.
Zillich R, Dowson J. Root canal morphology of mandibular first and second pre- molars. Oral Surg Oral Med Oral Pathol. 1973;36:738–44.
Fernandes M, de Ataide I. Nonsurgical management of periapical lesions. J Conserv Dent. 2010;13(4):240-245. doi:10.4103/0972-0707.73384



