Four canals maxillary second molars
11/01/2024
Enrico Cassai
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Maxillary molars have one of the most complex root canal anatomies. Six different variations of a second maxillary molar have been reported in a retrospective study by Peikoff et al. These variations include 1) three separate roots and canals (56%), 2) three separate roots and four canals (two canals in mesiobuccal) (22.7%), 3) Three roots and canals with union of mesiobuccal and distobuccal canals to form a common buccal canal (9%), 4) Two separate roots and canals (6.9%), 5) A single root and canal (3.1%) and 6) Four distinct roots and four canals including two palatal canals (1.4%).
Rostein and Libfild have reported a prevalence of 0.4% for second maxillary molar with four roots in a large series of 1200 teeth radiographic assessment. However there are several case reports in literature which report the treatment of second maxillary molar with two palatal canals.
Second maxillary molars with three buccal roots, five roots and canals (two palatal and three buccal), as well as first maxillary molar with three palatal canal have been reported as abnormalities. These variations confirm unexpected root canal morphology in maxillary molars.
Negin Ghasemi et al with a systematic review evaluated the papers published in the field of root canal anatomy and configuration of the root canal system in permanent maxillary second molars. Results of this research are summarized in the table 1, 2 ,3, 4.
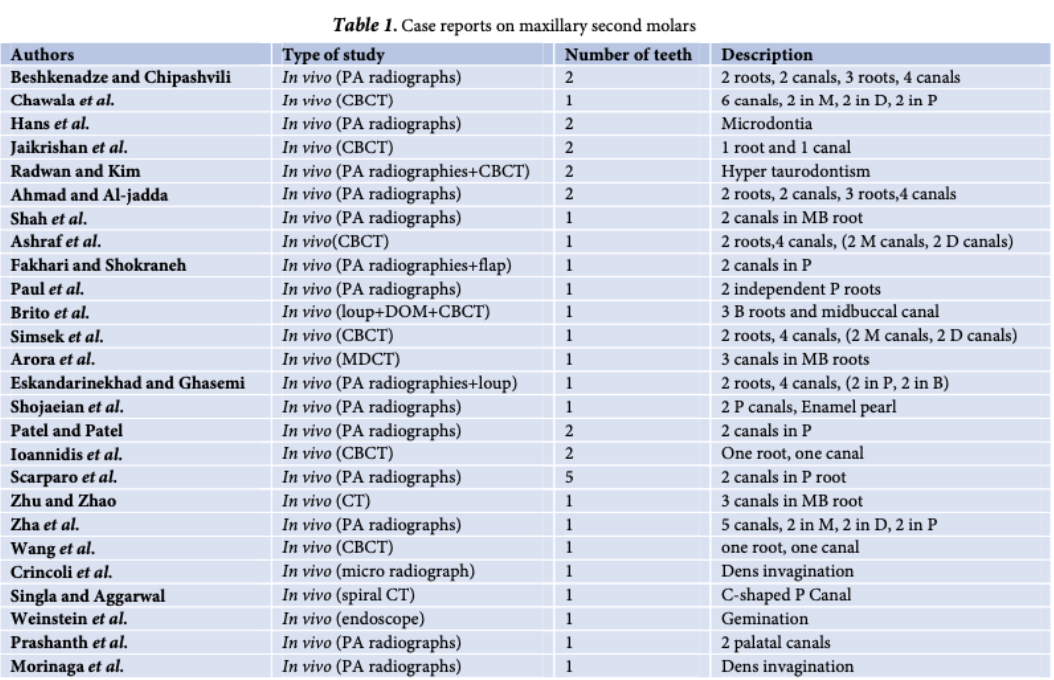
Fig. 1
Negin Ghasemi a, Saeed Rahimi a*, Shahriar Shahi a, Mohammad Samiei b, Mohammad Frough Reyhani b, Bahram Ranjkesh c :A Review on Root Anatomy and Canal Configuration of the Maxillary Second Molars, IEJ 2017
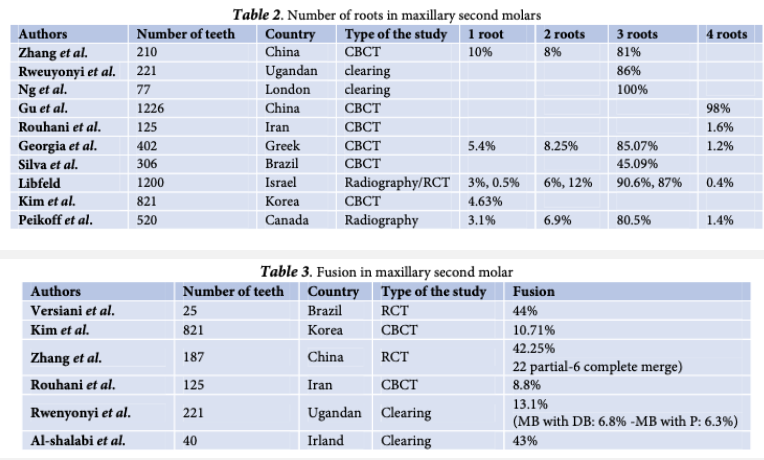
Fig. 2
Negin Ghasemi a, Saeed Rahimi a*, Shahriar Shahi a, Mohammad Samiei b, Mohammad Frough Reyhani b, Bahram Ranjkesh c :A Review on Root Anatomy and Canal Configuration of the Maxillary Second Molars, IEJ 2017
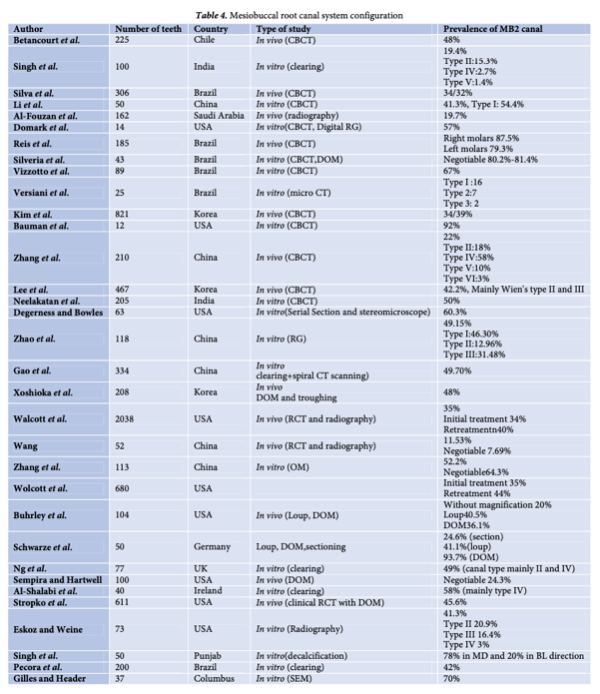
Fig. 3
Negin Ghasemi a, Saeed Rahimi a*, Shahriar Shahi a, Mohammad Samiei b, Mohammad Frough Reyhani b, Bahram Ranjkesh c :A Review on Root Anatomy and Canal Configuration of the Maxillary Second Molars, IEJ 2017
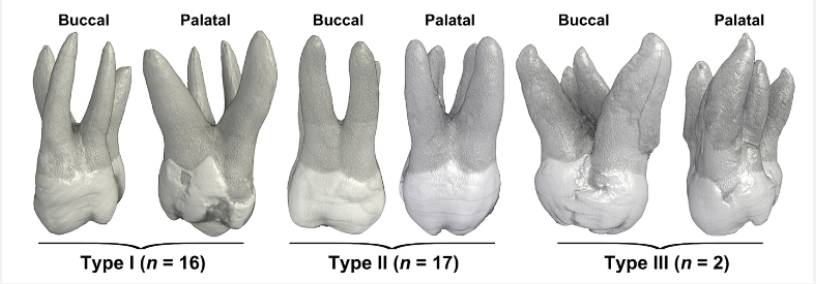
Fig. 4
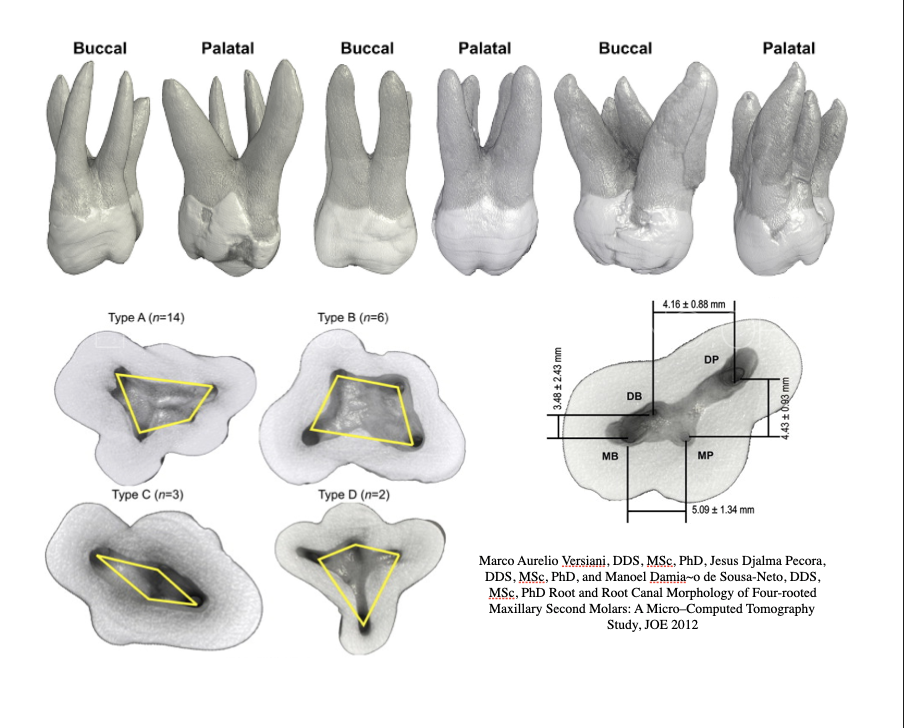
Versiani, Pecora et al classified the external morphology of 4-rooted maxillary second molars into 3 types according to the divergence of their roots.
In type I, palatal roots were widely divergent and often longer and more tortuous than buccal roots that were less divergent and often ‘‘cow-horn’’ shaped.
In type II, roots had blunt apices, run almost parallel to each other, and were often shorter than type I tooth.
In type III, palatal roots were less divergent and often shorter than buccal roots that were widely divergent. Then, the size of the mesiobuccal (MB), mesiopalatal (MP), distobuccal (DB), and disto- palatal (DP) roots and the distance between the anatomical apexes were measured by using a digital caliper with a resolution of 0.01 mm (Mitutoyo MTI Corporation, Tokyo, Japan). The direction of root curvature and the occurrence of fusion and enamel structures at the root were also evaluated.
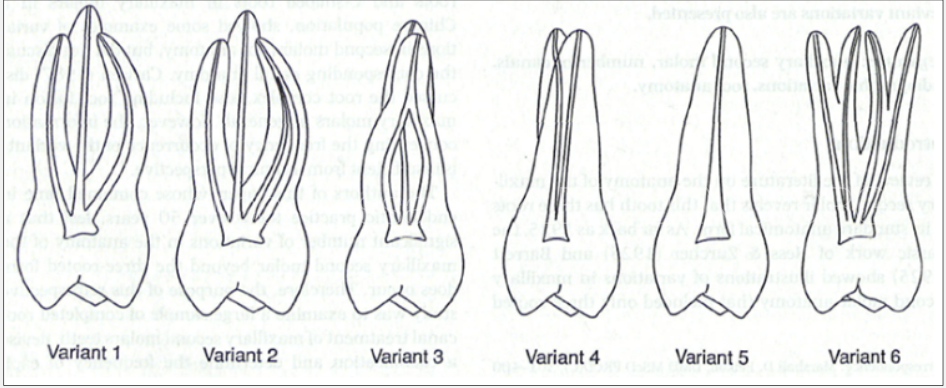
Fig. 5
X-Ray & CBCT INVESTIGATION
Before starting the endodontic treatment it is necessary to perform an intraoral x-ray to understand the anatomy of the upper second molar to be treated. The interpretation of the x-ray should allow the clinician to understand whether the molar has 3 or 4 roots, fused, divergent and the anatomical features of the root canal to study an adequate endodontic treatment plan (shaping, cleaning, filling). Initial radiographic interpretation of the second maxillary molar root anatomy may be more complicated because of superimposition of roots on each other or adjacent bony structures. Clinicians encounter a dilemma when additional abnormality presents in the area. Thorough knowledge of anatomical variations and frequent anomalies in the region besides multiple radiographs with different angles or cone- beam computed tomography (CBCT) can be helpful.
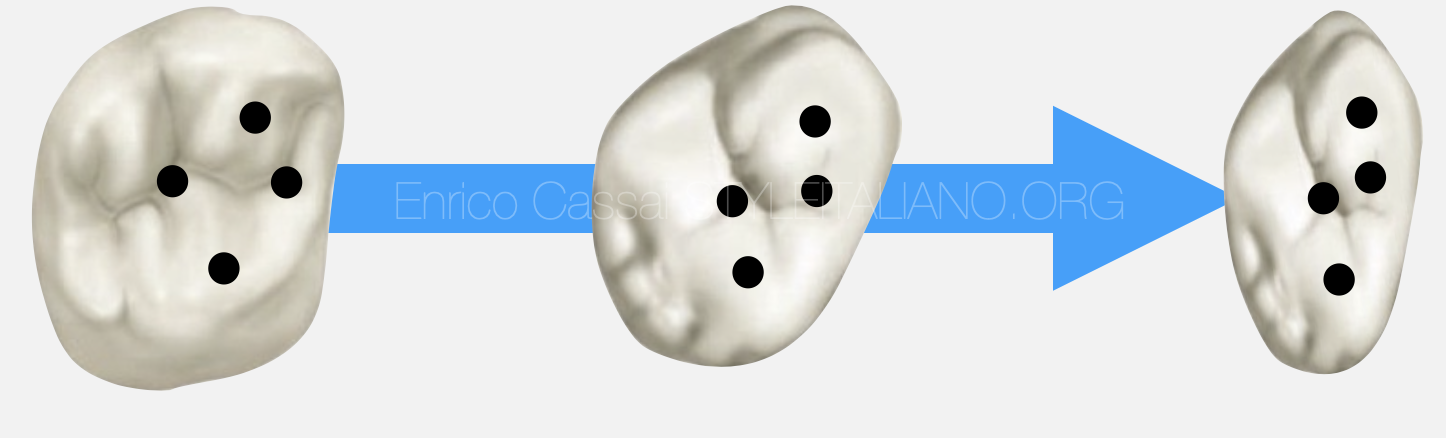
Fig. 6
OCCLUSAL SURFACE INVESTIGATION
Looking to the M-D occlusal surface it is possible to guess the positions of the orifices: more likely the anatomy of the second molar is similar to that of the first molar, more the disposition of the orifices is similar to those of first molar. Conversely, the more the M-D extension of the occlusal surface is reduced and flattened and similar to the third molar, the canals will tend to be arranged almost along a B-P line.

Fig. 7
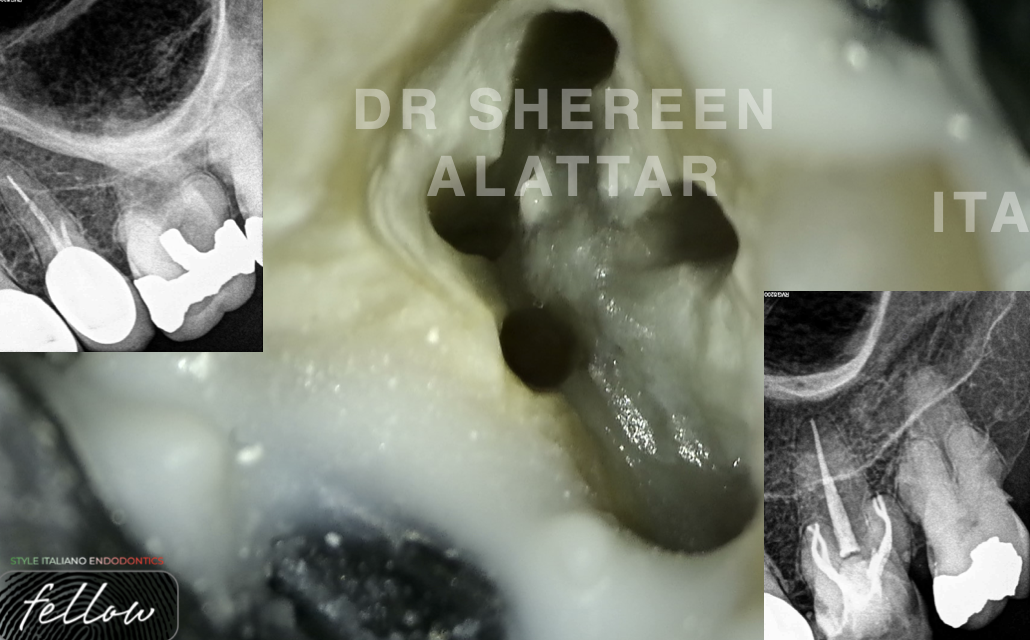
Case report 1: Second upper molar with four canals and two palatal roots
A 45-year-old woman came to my clinic complaining of sever toothache especially during mastication.
The patient medical history was negative.
Clinical examination revealed tenderness to percussion and palpation of peri-radicular zone of the left maxillary second molar.
Vitality tests were negative.
Radiographic image (periapical) revealed radiolucency around palatal apex of DB and palatal canal; moreover, from an accurate x-ray investigation it is possible to detect the presence of 4 separated roots.
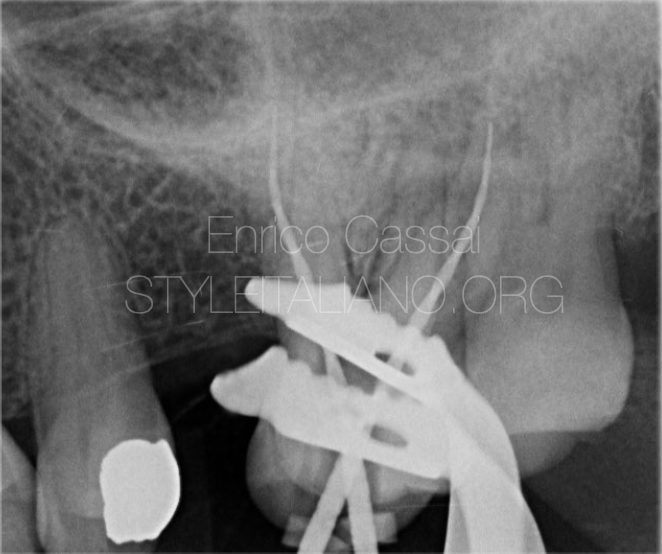
Fig. 8
Palatal roots: MP and DP
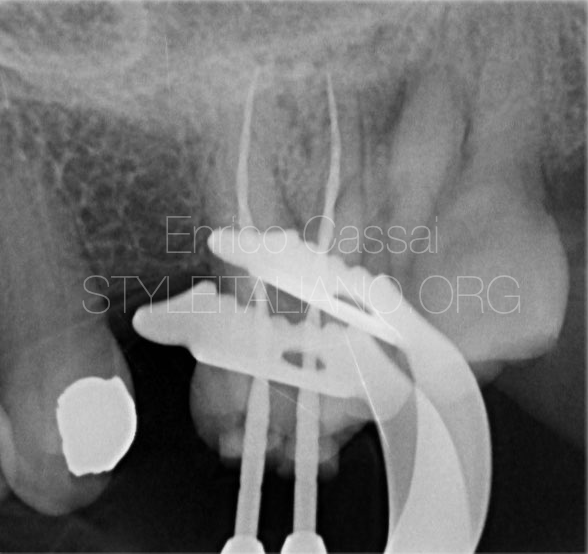
Fig. 9
Buccal roots: MB and DB

Fig. 10
Shaping: VDW rotate (MP,DP) and Reciproc Blue (MB,DB)
Cleaning: NaClO activated, EDTA, Clorexidine
Obturation: continous wave of condensation

Fig. 11
Final restoration: direct composite restoration

Fig. 12
Case report 2: Second upper molar with four canals under a crown
A 63-year-old man comes to my observation after a definitive bridge 17-15 cemented a few months ago by his dentist.
The patient reports pulpal pain affecting tooth 17 and the colleague who refers the patient to me asks me to perform the endodontic treatment through the crown.
Considerations: in this case it is necessary to create a larger access cavity than that which would be created for a normal second molar considering that the underlying dental abutment could have been prepared to make it parallel to the mesial prosthetic abutment.
Radiographic image (periapical) revealed radiolucency around MB canal; moreover, from an accurate x-ray investigation it is not so clear the identification of roots and canals, so a CBCt could be helpfull in this case before starting the endodontic therapy.
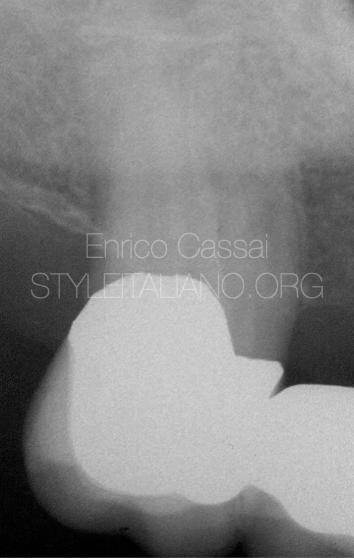
Fig. 13
Pre operative

Fig. 14
Shaping: Reciproc Blue 25, 50(P)
Cleaning: NaClO activated, EDTA, Clorexidine
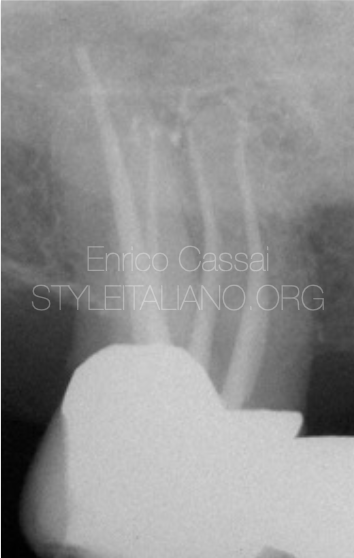
Fig. 15
Obturation: continous wave of condensation
Final restoration: direct composite restoration
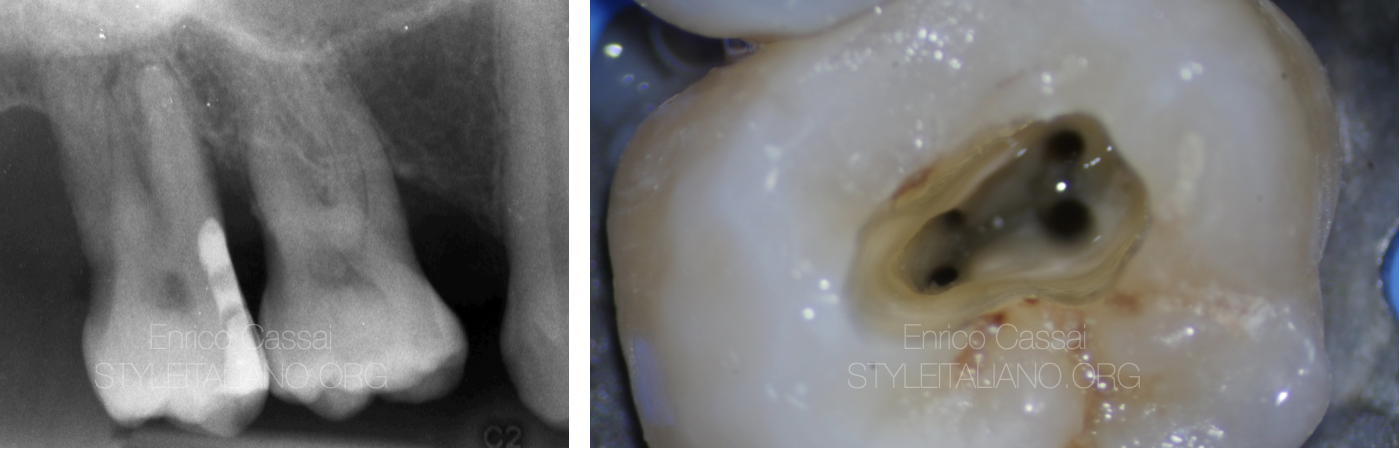
Fig. 16
Case report 3: second upper molar with four canals
A 65-year-old man came to my clinic complaining of sever toothache during mastication and revealed an acute pain in the days before.
Clinical examination revealed tenderness to percussion and palpation of peri-radicular zone of the MB root of the right maxillary second molar.
Vitality tests were negative.
Radiographic image (periapical) revealed radiolucency around MB canal.

Fig. 17
MB1 and MB2

Fig. 18
DB and P
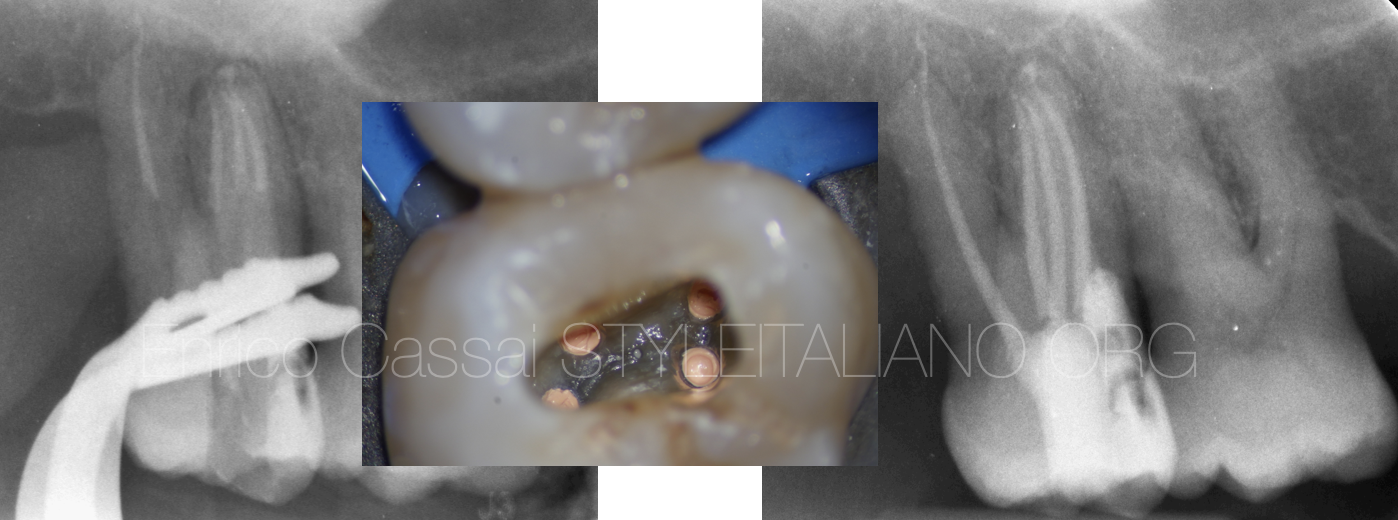
Fig. 19
Shaping: Reciproc Blue
Cleaning: NaClO activated, EDTA, Clorexidine
Obturation: continous wave of condensation
Final restoration: direct composite restoration
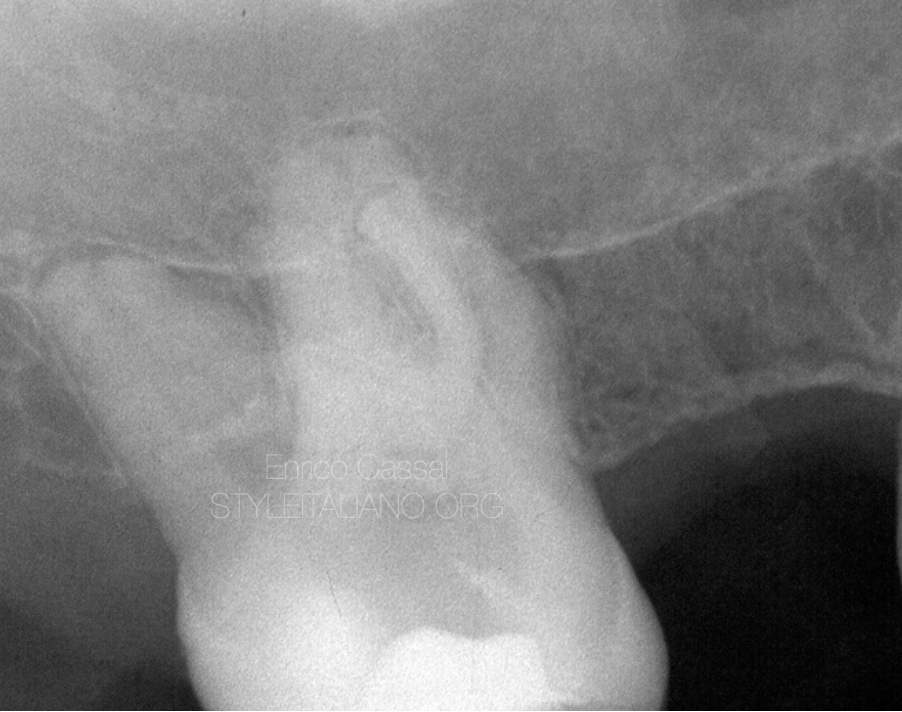
Fig. 20
Case report 4: second upper molar with four canals under calculus
A 70 year old patient is referred to me by a colleague because he cannot find the canals.
The tooth has already been opened but from a careful x-ray analysis it can be observed the presence of a pulp stone on the the pulp chamber floor which prevents the correct finding of all the canal orifices.
Furthermore, the presence of at least 4 independent roots is noted. It would therefore be of great help in this case to perform a pre-operative CBCT in order to correctly plan the subsequent steps of endodontic therapy.

Fig. 21
Shaping: Reciproc Blue 40/50
Cleaning: NaClO activated, EDTA, Clorexidine
Video of the procedure

Fig. 22
Obturation: continous wave of condensation
Final restoration: direct composite restoration

Fig. 23
Case 5: Second upper molar with 4 canals and first upper molar retreatment
A 50 year old patient comes to my observation while I was doing endodontic consultation in a dental office.
The patient reports pain in the upper left second molar.
Clinical examination revealed tenderness to percussion and palpation of peri-radicular zone of the left maxillary second molar and first molar.
Radiographic image revealed the presence of a decay affecting the right maxillary second molar.
Based on clinical and radiographic findings chronic irreversible pulpitis of right maxillary second molar was diagnosed, which required endodontic management.
in the same appointment also the retreatment of first molar is planned.

Fig. 24
Shaping: VDW Rotate 25.06 (17), Reciproc Blue (16)
Cleaning: NaClO activated, EDTA, Clorexidine
Obturation: continous wave of condensation
Final restoration: direct composite restoration
Conclusions
This article aims to give indications on the treatment of upper second molars, which can present considerable anatomical variability. Missed canals, incorrect execution of the access cavity, ... can lead to failure of endodontic therapy over time. Therefore, knowledge of the canal anatomy is mandatory. This can be assessed by performing a pre-operative x-ray and a CBCT in case of persistence of further diagnostic doubts.
It is also very important to pay attention to the anatomy of the occlusal surface: the more similar it is in terms of M-D extension to the first molar, the more likely the anatomy of the second molar is similar to that of the first molar. Conversely, the more the M-D extension of the occlusal surface is reduced and flattened and similar to the third molar, the canals will tend to be arranged almost along a B-P line.
The preoperative evaluation must then allow the clinician to choose the most appropriate shaping system for the canal anatomy, preferring instruments with low taper and treated alloy in cases of particularly difficult anatomy. This also applies to the cleaning system to be used (metal needles vs. plastic needles) and to the irrigant activation system (US or sonic with plastic tips) and to the endocanal obturation (continuous wave of condensation VS carrier based VS single cone and bioceramic).
Bibliography
Negin Ghasemi a, Saeed Rahimi a*, Shahriar Shahi a, Mohammad Samiei b, Mohammad Frough Reyhani b, Bahram Ranjkesh c :A Review on Root Anatomy and Canal Configuration of the Maxillary Second Molars, IEJ 2017
Alrahabi M, Sohail Zafar M. Evaluation of root canal morphology of maxillary molars using cone beam computed tomography. Pak J Med Sci. 2015;31(2):426-30.
Benenati FW. Maxillary second molar with two palatal canals and a palatogingival groove. J Endod.1985;11(7):308-10.
Marco Aurelio Versiani, DDS, MSc, PhD, Jesus Djalma Pecora, DDS, MSc, PhD, and Manoel Damia~o de Sousa-Neto, DDS, MSc, PhD Root and Root Canal Morphology of Four-rooted Maxillary Second Molars: A Micro-Computed Tomography Study, JOE 2012
Peikoff MD, Christie WH, Fogel HM. The maxillary second molar: variations in the number of roots and canals. Int Endod J. 1996;29(6):365-9.
Libfeld H, Rotstein I. Incidence of four-rooted maxillary second molars: literature review and radiographic survey of 1,200 teeth. J Endod. 1989;15(3):129-31.