Deep split management, tips and tricks
17/08/2023
Ivan Mirovic
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Deep split, also known as Vertucci type V canal anatomy, is one of the most challenging anatomies in root canal treatment.
It presents a situation where one canal leaves the pulp chamber and divides short of the apex into two separate apical foramina (1-2). Treatment of deep split could be a significant challenge for the clinicians in terms of diagnosis, preparation of canals and obturation.

Fig. 1
Deep split anatomy. Courtesy of Dr. Marco Versiani

Fig. 2
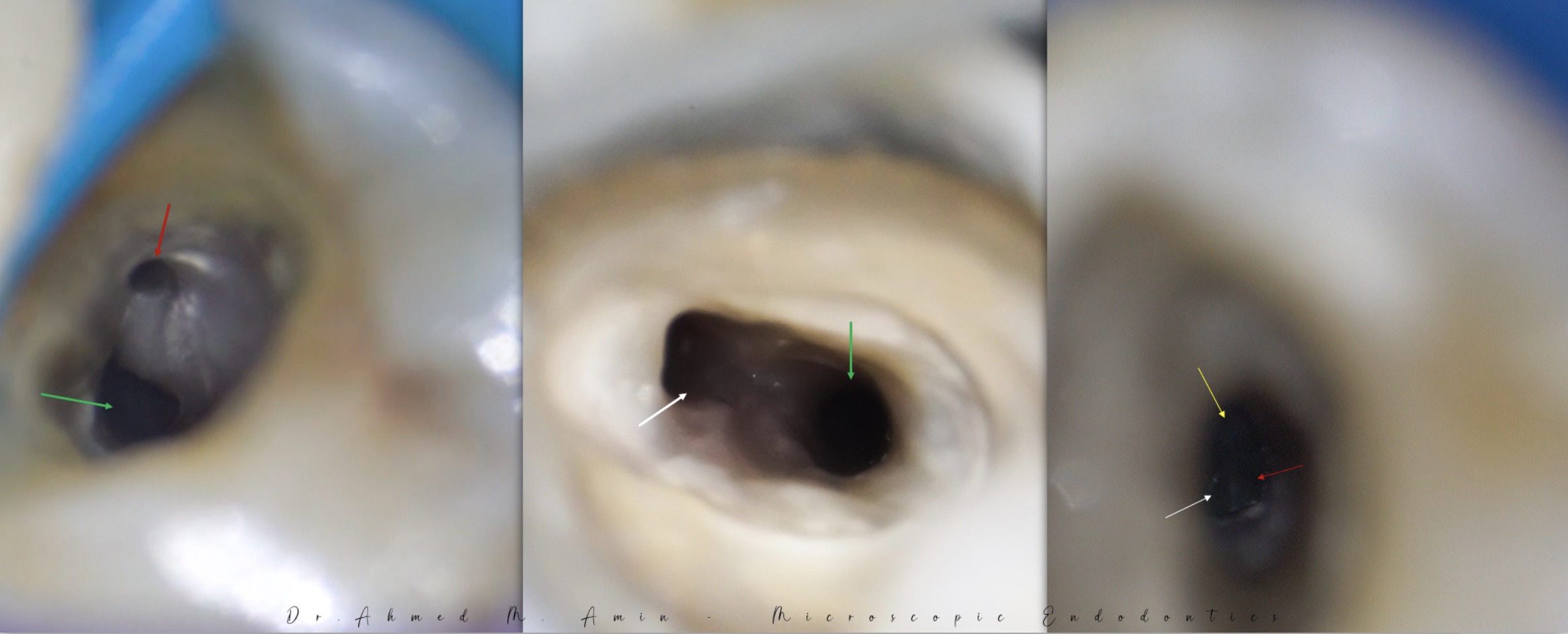
The most useful tips for diagnosis of deep split are: radiographs, magnification and tactile sensation. Radiographs, especially cbct, could be of great help in diagnosis. But keep in mind that deep split is not necessarily visible on periapical x rays. Magnification and illumination, preferably dental operating microscope, are of great help in diagnosis of deep split. Remember, if you can see it you can do it.
The figure, courtesy of Dr José Conde Pais, shows a deep split seen under the microscope
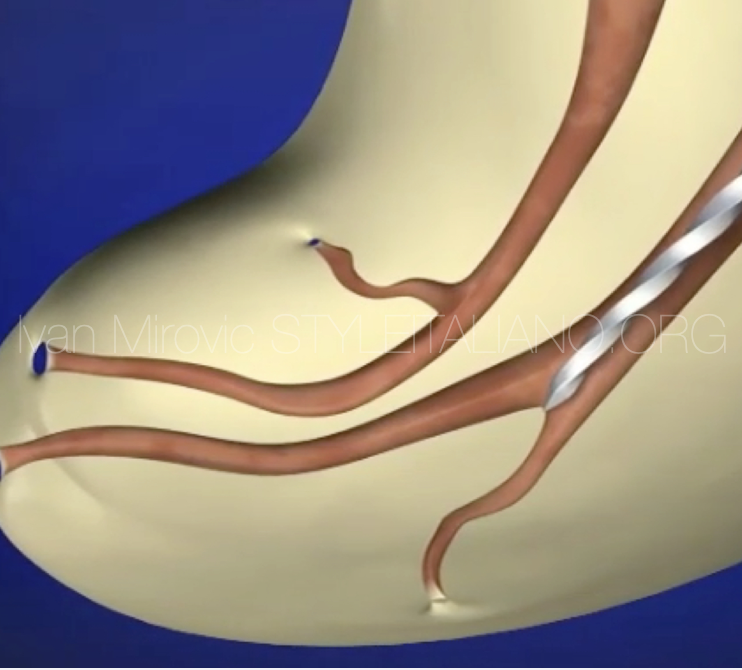
Fig. 3
But in many cases the only way to diagnose deep split anatomy is tactile sensation. In case there is no reproducible glide path, always suspect deep split!

Fig. 4
If the apex locator shows confused reading and it is reading two different working lengths in the same canal this could be an indication of deep split.
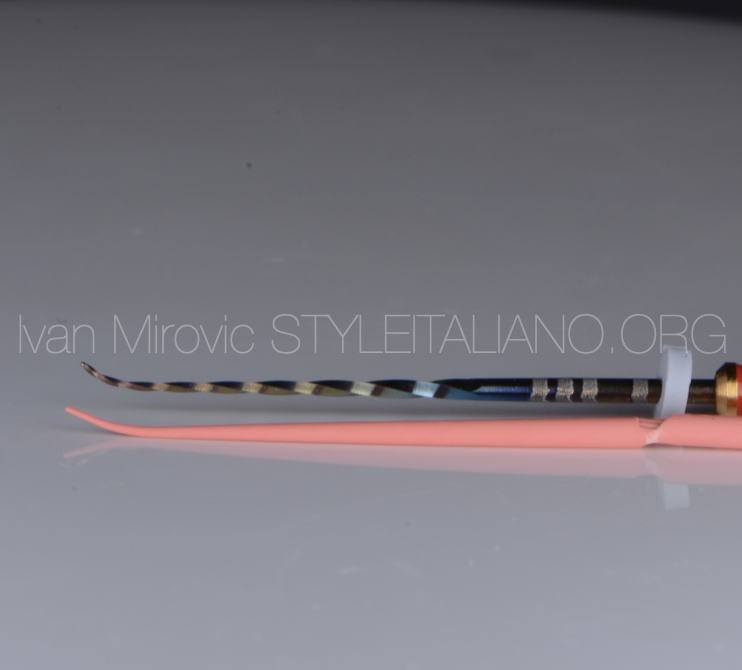
Fig. 5
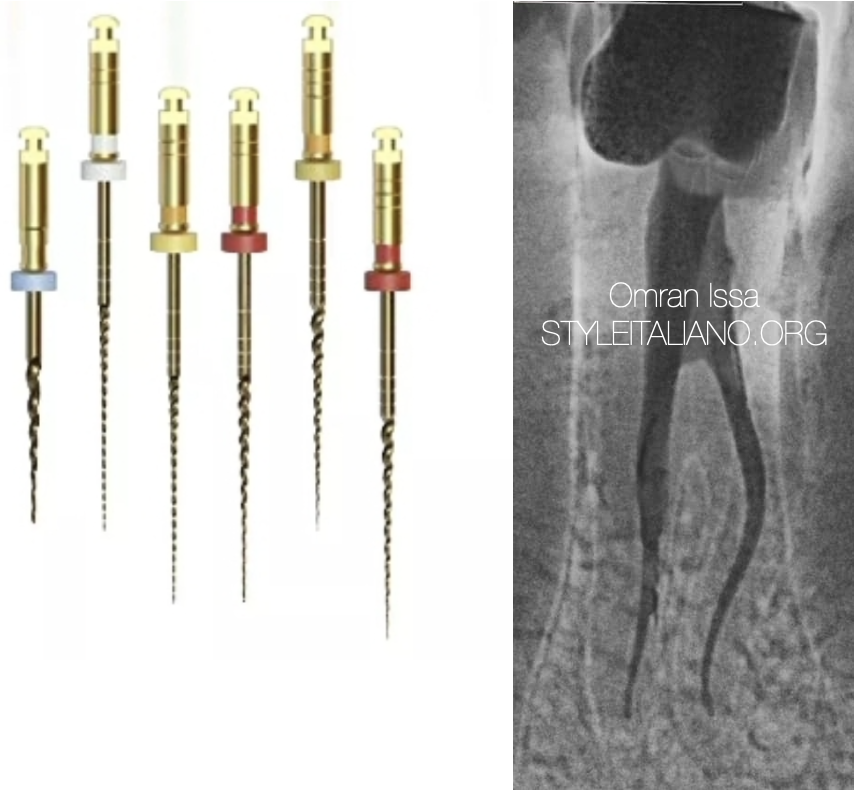
When preparing canals usually there is a more straight canal, which could be prepared with straight instruments, and a branching canal which requires pre curving both hand and rotary files, and usually master gutta percha point.

Fig. 6
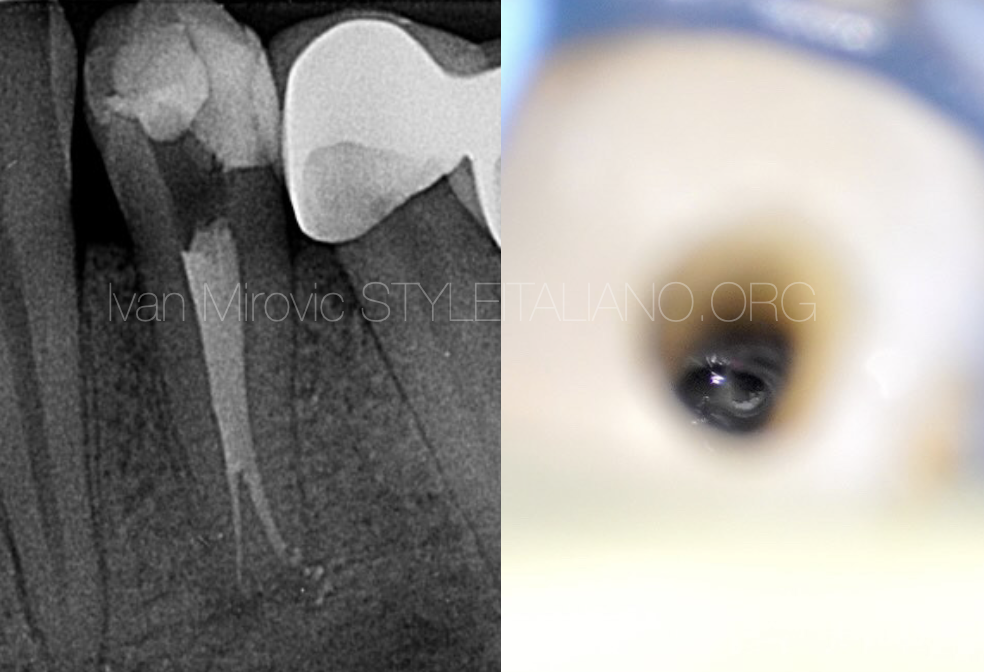
Preoperative radiograph of lower first premolar with typical deep split anatomy.
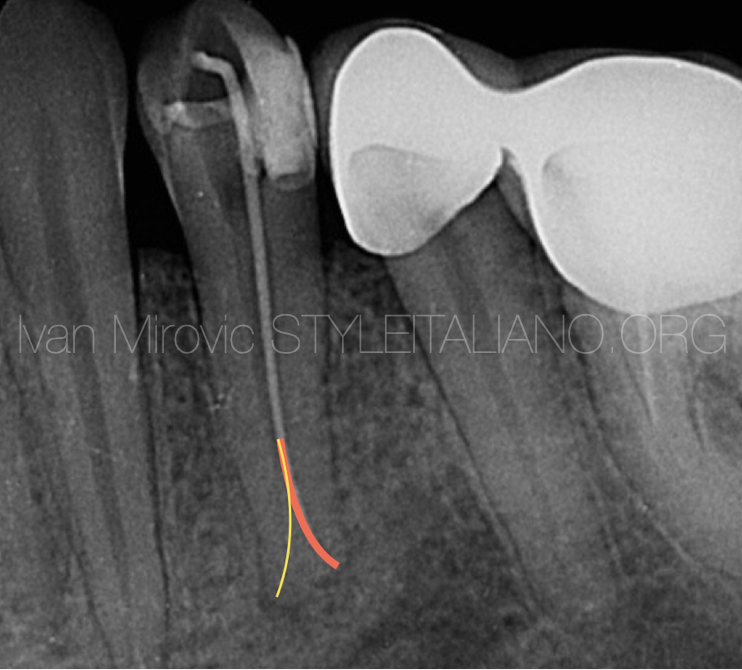
Fig. 7
Straight branch, marked by red, was prepared up to 25/06. Lingual branch was prepared to 20/04 and required pre curving hand, rotary files and master gutta percha point.

Fig. 8
Postoperative radiograph

Fig. 9
Obturation of deep split anatomies presents significant challenges and requires specific technique modifications. The ideal scenario is to fit gutta percha cones in both branches simultaneously which is usually an impossible task. If we fit a cone in one canal first and downpack to the level of the split in most of the cases we will end up blocking other branch. The tip I use in those cases is that I fit the cones in both branches separately. Then I make a small cut with a blade on one gp point at the level of the split (Fig 9.), coat it with sealer and place it in the canal. Rotating the cone with fingers the same way we are rotating files will break the end of the cone at the split level. After that I place the other cone in other branch without a problem, downpack to the level of the split and backfill.
Conclusions
Using these simple tips and tricks the clinicians should be more effective and confident in diagnosis and treatment of deep split anatomies.
Bibliography
- Bertani P, Gagliani M, Gorni F: Retreatments. Milan: Edra S.p.A; 2020
- Roda RS, Gettleman BH: Nonsurgical retreatment. In: Hagreves KM, Cohen S, editors. Cohen’s pathways of the pulp, ed 10. New York: Elsevier; 2011.
- Berutti E, Castellucci A: Cleaning and shaping the root canal system. In Castellucci A, editor. Endodontics, Vol. II. Florence: Tridente S.r.l; 2006. p. 396-437