
Deep Margin Elevation and Clinical Crown Lengthening: Biological considerations and clinical procedures
04/01/2025
Davide Guglielmi
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
.
The workshop conducted by the AAP (American Academy of Periodontology) and the EFP (European Federation of Periodontology) confirms that placing the margin of the restoration within the supracrestal connective tissue attachment fibers poses a significant risk for patients to develop periodontal complications.
It is crucial to highlight that the supracrestal tissue attachment exhibits considerable dimensional variability both inter- and intra-patient, ranging from 0.2 to 6.73 mm.
The relatively constant component is the connective attachment, which averages 1 - 1.5 mm; thus, the portion associated with the junctional epithelium demonstrates the greatest variability between the two.
In clinical scenarios where the dental lesion presents a margin extending apically to the gingival sulcus, it is imperative to assess whether this margin is located within the junctional epithelium space, deeper into the connective attachment, or even apical to the osseous crest. In instances where the lesion encroaches upon the connective attachment or is apical to the osseous crest, surgical crown lengthening becomes necessary to expose the restoration margin, ensuring the proper execution of restorative/prosthetic reconstruction, and mitigating the risk of future periodontal damage.

Fig. 1
Preoperative views of the IVth sextant: buccal, lingual and occlusal

Fig. 2
Pre-operative peri-apical x-ray.

Fig. 3
Post Non Surgical retreatment (3.6) peri-apical x-ray.

Fig. 4
Flap design and primary incision (buccal view)

Fig. 5
Flap design and primary incision (lingual view)

Fig. 6
Flap elevation

Fig. 7
Removal of the secondary flap
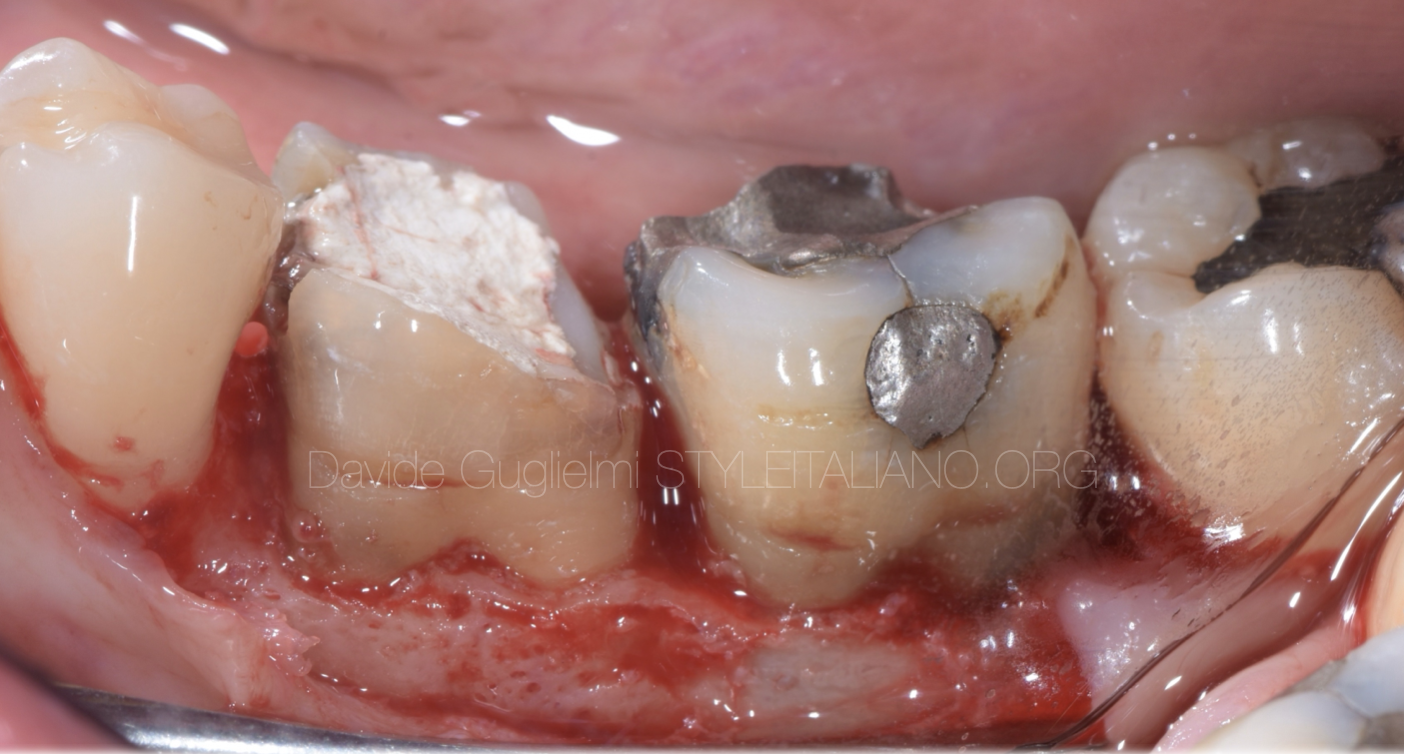
Fig. 8
Buccal aspect before the osseous resective surgery

Fig. 9
Use of bone probing to define the distance between the bone crest and the healthy margin.
It can be noticed a iatrogenic perforation at the 3.6 apical to the cej
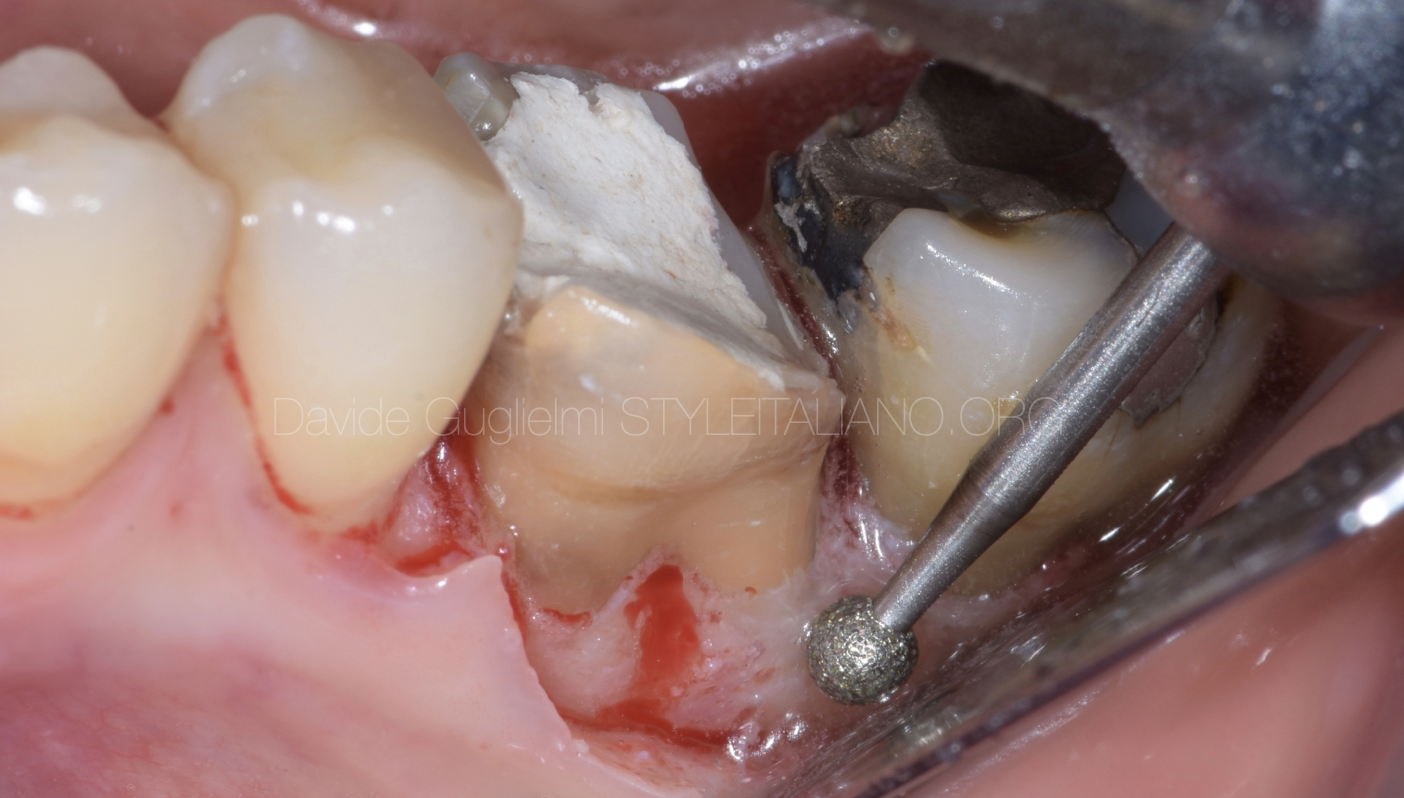
Fig. 10
Osteoplasty performed with a diamond bur mounted on a red handpiece

Fig. 11
Ostectomy conducted utilizing a hand-held chisel

Fig. 12
Buccal aspect of the modified bone thickness and height, after osteoplasty and ostectomy

Fig. 13
Vertical mattress sutures anchored to the periosteum with the flap positioned apically

Fig. 14
Healing at one week and removal of the sutures

Fig. 15
After isolating the operative field, the cleaning of elements 3.6 and 3.7 is performed: the iatrogenic perforation results evident

Fig. 16
Occlusal view of the elements 3.6 and 3.7 cleaned, sandblasted and etched .

Fig. 17
Post-endodontic reconstruction with the insertion of a fiber post and the execution of a build-up with dual composite resin

Fig. 18
Occlusal views of the cavities morphology

Fig. 19
3.6 3.7 composite overlays

Fig. 20
Overlays cementation phases 3.6, 3.7 and occlusal restoration of the wisdom tooth are performed.

Fig. 21
Post operative periapical x ray

Fig. 22
The final image of the overlays highlights an excellent integration of the soft tissues with the prosthetic restoration, ensuring the stability of the results in the long term.
Conclusions
Crown lengthening is one of the procedures traditionally performed to expose the margins of dental tissue positioned apically to the gingival sulcus in severely compromised teeth.
However, it has significant limitations such as invasiveness, anatomical complications (exposure of root concavities or furcations), and postoperative discomfort for the patient. Therefore, it is important to understand the indications for this approach and when it may be possible to avoid it. The availability of modern materials, such as composite resins, and the need to follow strict operational protocols, along with an interdisciplinary approach that also considers periodontal health, allows for the achievement of high-quality and long-lasting results.
This clinical case, along with the cited studies, underscores the importance of accurate planning and the use of appropriate techniques to ensure the success of treatments in restorative dentistry.
Bibliography
- Juloski J, Köken S, Ferrari M. Cervical margin relocation in indirect adhesive restorations: A literature review. J Prosthodont Res. 2018 Jul;62(3):273-280.
- Bertoldi C, Monari E, Cortellini P, Generali L, Lucchi A, Spinato S, Zaffe D. Clinical and histological reaction of periodontal tissues to subgingival resin composite restorations. Clin Oral Investig. 2020 Feb;24(2):1001-1011.
- Pittaluga A, Minoli M, Diana C, Bovio M, Guglielmi D. Rilocazione del margine e allungamento di corona clinica. Considerazioni biologiche, strutturali e procedure cliniche. Parte 1. Quintessenza Int. 2024;38(1):34-42.
- Veneziani M. Adhesive restorations in the posterior area with subgin- gival cervical margins: new classification and differentiated treatment approach. Eur J Esthet Dent. 2010 Spring;5(1):50-76.
- Schmidt JC, Sahrmann P, Weiger R, Schmidlin PR, Walter C. Biologic width dimensions--a systematic review. J Clin Periodontol. 2013 May;40(5):493-504.
- Smith SC, Goh R, Ma S, Nogueira GR, Atieh M, Tawse-Smith A. Peri- odontal tissue changes after crown lengthening surgery: A systematic review and meta-analysis. Saudi Dent J. 2023 May;35(4):294-304.
- Gupta G, Gupta R, Gupta N, Gupta U. Crown lengthening procedures-a review article. IOSR J Dental Medical Sciences. 2015;14(4):27-37.
- Marzadori M, Stefanini M, Sangiorgi M, Mounssif I, Monaco C, Zucchelli G. Crown lengthening and restorative procedures in the esthetic zone. Periodontol 2000. 2018 Jun;77(1):84-92.




