The advantages of pre-operative radiograph in the diagnosis and in formulating the proper treatment plan
12/04/2020
Ahmed Alwaidh
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Correct diagnosis is the key to all predictable endodontic treatment. Root canal treatment depends largely on IOPA (Intra-oral periapical) radiographs to assess the anatomy of the tooth and periapical structures (Forsberg 1987a, b, Cotton et al. 2009, Patel at al. 2009).
A 23 years old male presented complaining of moderate dull pain in his UL5 (Upper left second premolar) that increases with biting and eating. History of restoration 3 months ago. The patient reported that he had a sudden pain during previous treatment, with discomfort since then.
Clinical examination:
UL5 with DO Amalgam restoration. Negative response to cold test, moderate tenderness to percussion. UL4 and UL6 responded normally to cold test with negative tenderness to percussion.
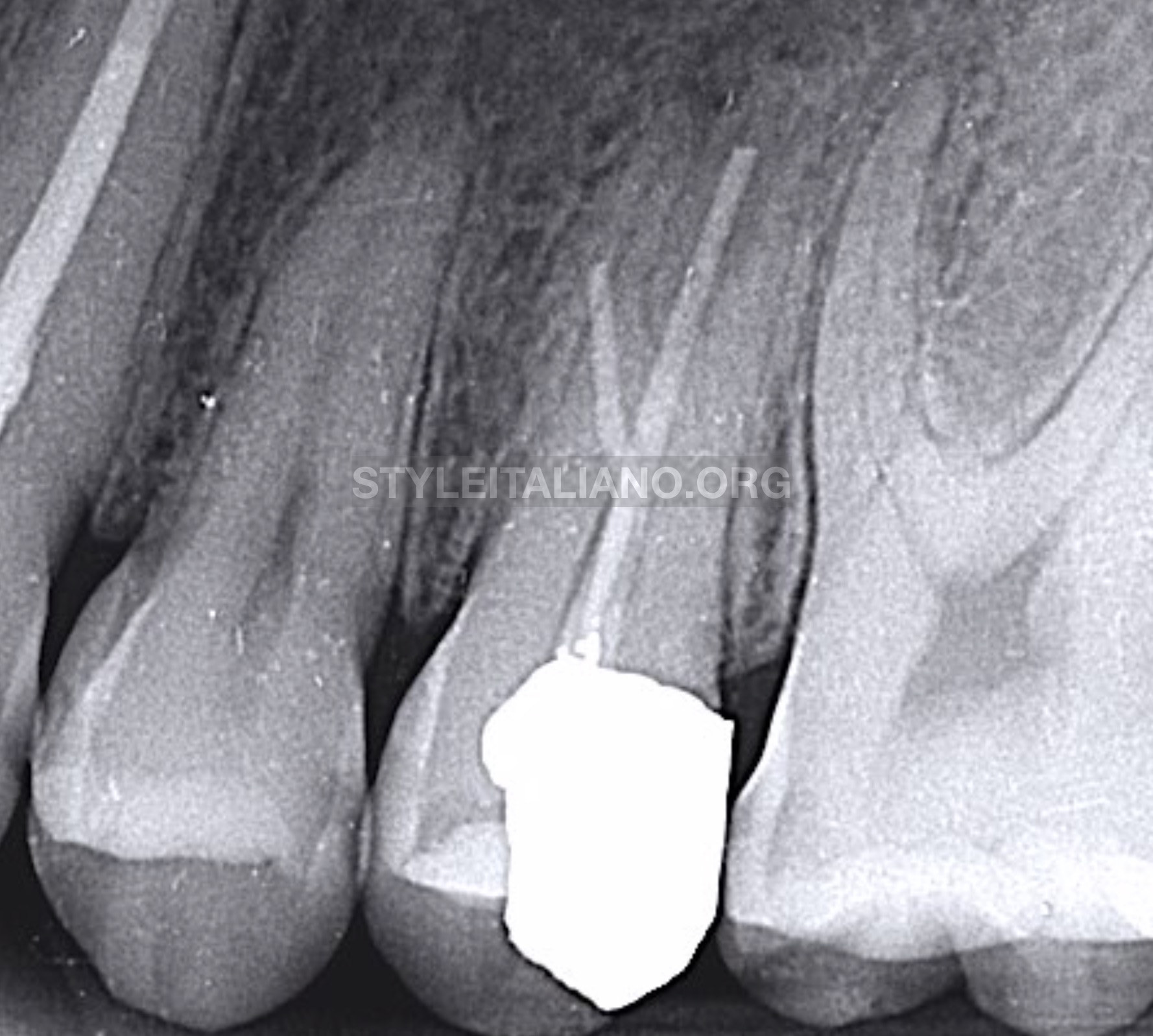
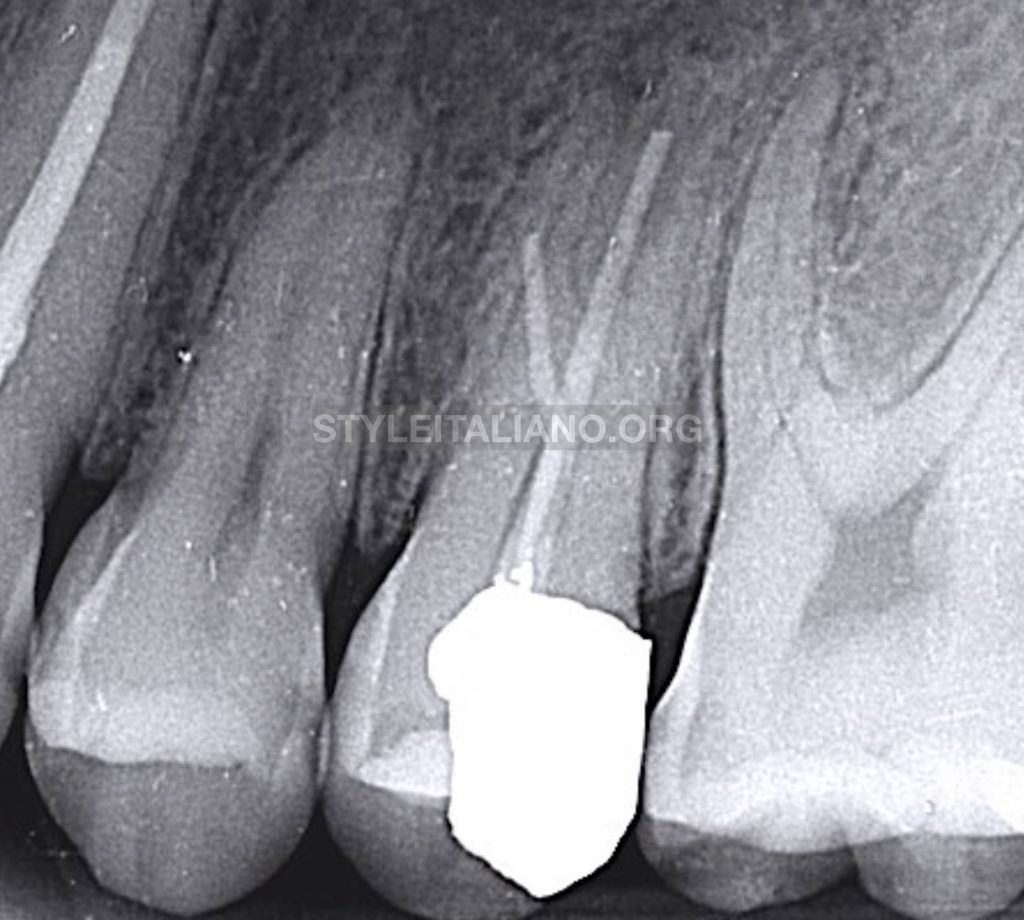
Fig. 1
Radiographical examination:
IOPA (Intra oral peri-apical) radiograph revealed that UL5 was previously treated with a failed root canal filling, It also revealed that UL5 has three roots; DB is a missed canal, P with short root canal filling, and MB is a curved root with short root filling material at the site of curvature (probably ledge or even perforation).IOPA also shows a peri-apical changes around MB and P roots. Patient clarified that he didn’t take an x-ray in the previous treatment.
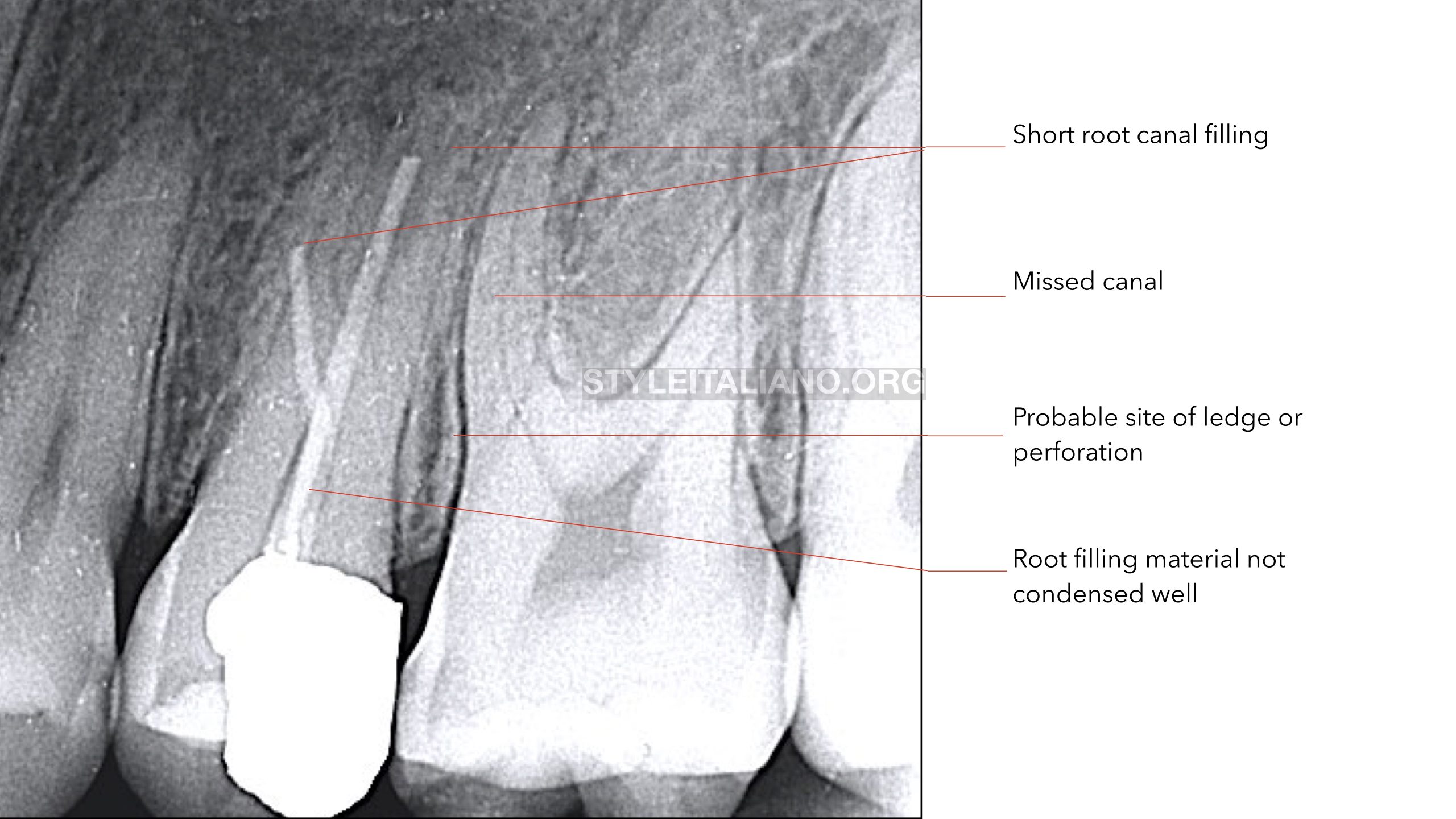
Fig. 2
Diagnosis:
Previously treated UL5, SAP (symptomatic apical periodontitis)
Treatment plan:
Re-treatment of UL5.
Objectives:
- Removing Amalgam restoration and old root filling materials.
- Getting a patent pathway though the whole working lengths of the canal.
- Chemo-mehcanical debridement of the root canal system.
- Filling the root canal system in a hermetic seal.
- Restore the tooth to function.

Fig. 3
Isolation with rubber dam.

Fig. 4
Removing old Amalgam restoration.

Fig. 5
Removing old root filling material using AF F-One #25/0.06 (Shanghai Fanta Dental Materials Co., Ltd., China).

Fig. 6
As expected, perforation in the MB root where old Gutta Percha was stopped at the curvature.
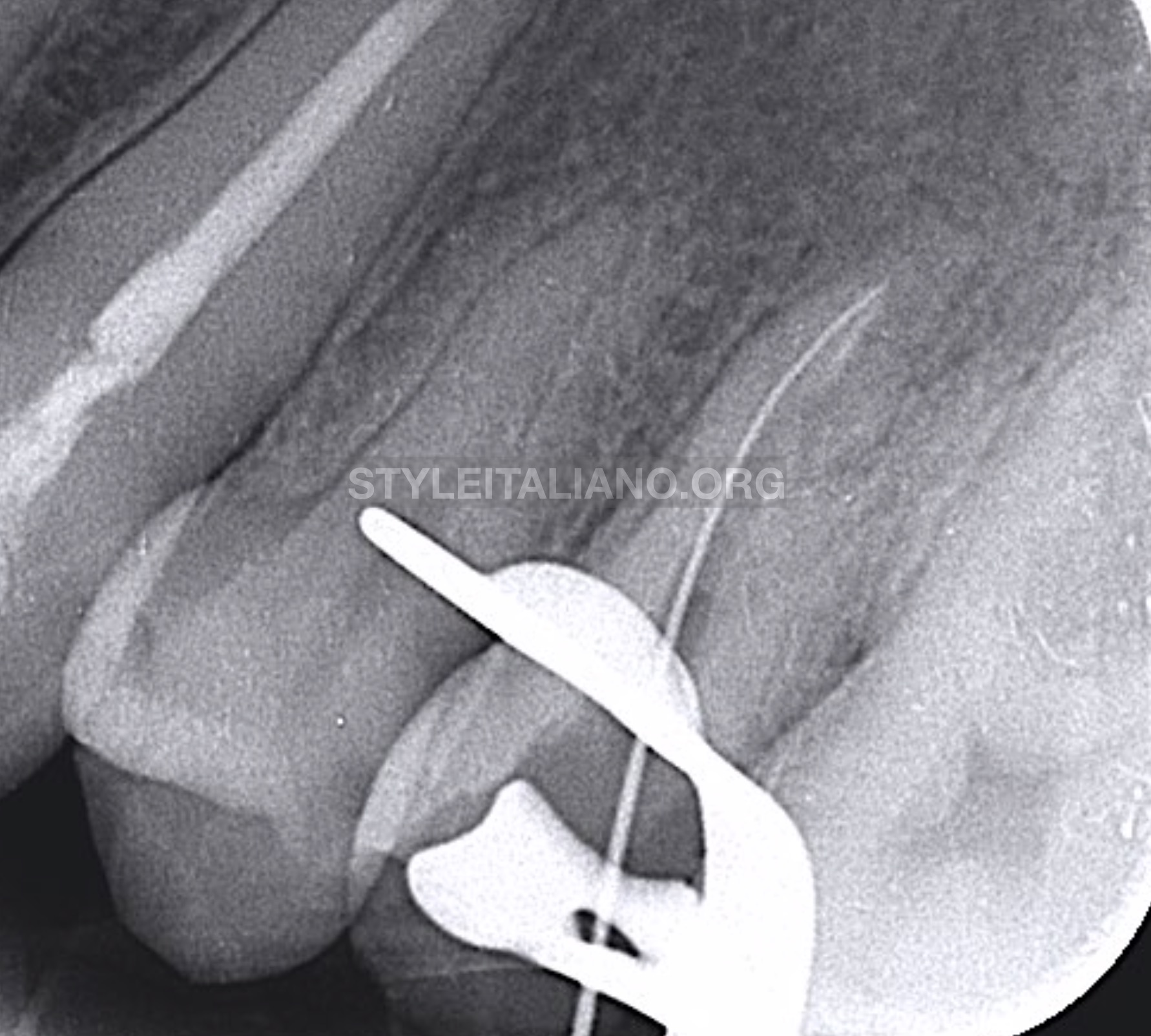
Fig. 7
Getting a patent pathway through the original MB canal using C file 10 (Shanghai Fanta Dental Materials Co., Ltd., China).
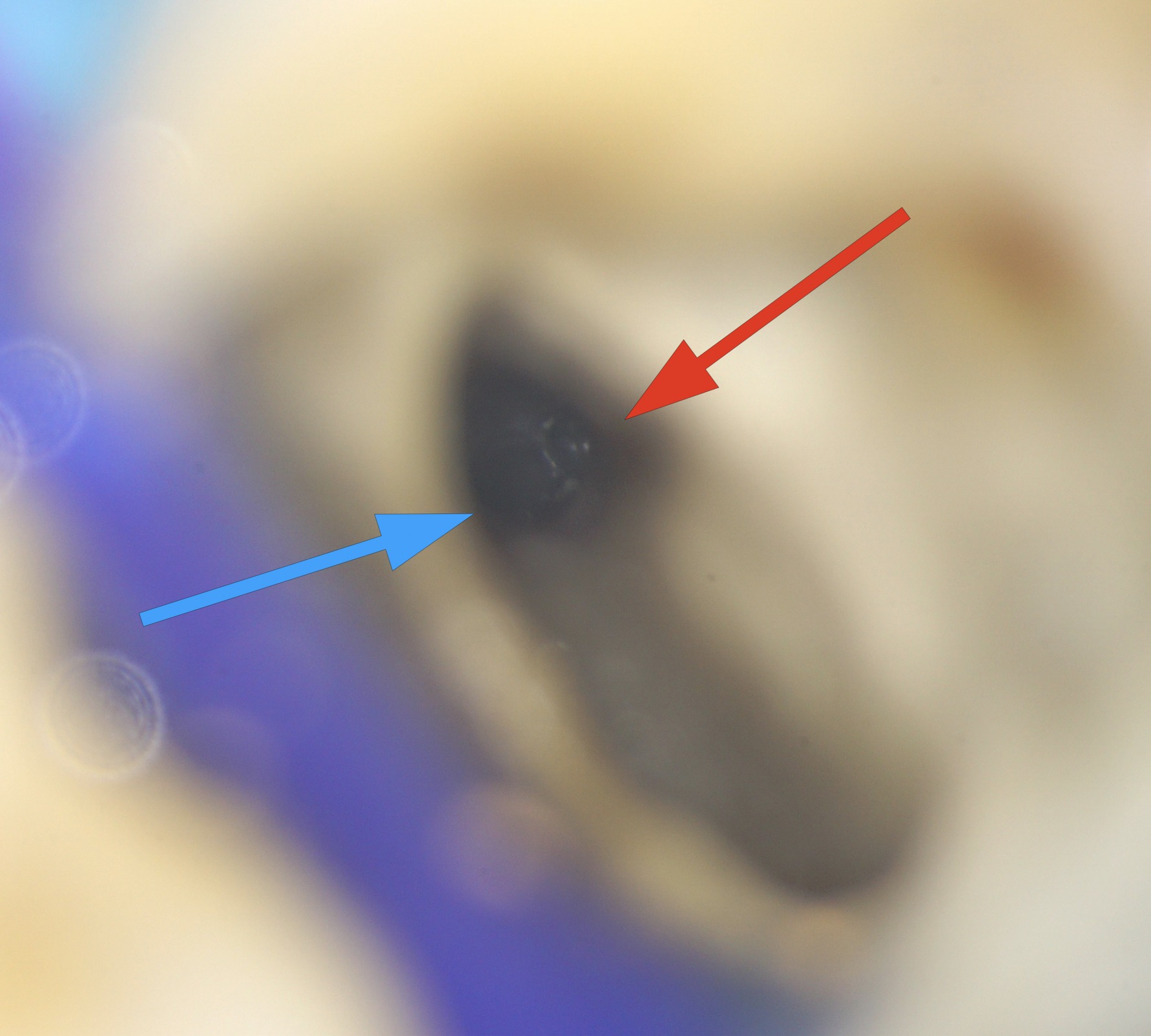
Fig. 8
MB system; Red arrow pointing to the perforation, while blue arrow pointing to the original canal.
All canals been prepared using AF F-One (MB and DB #25/0.04., P #25/0.06).
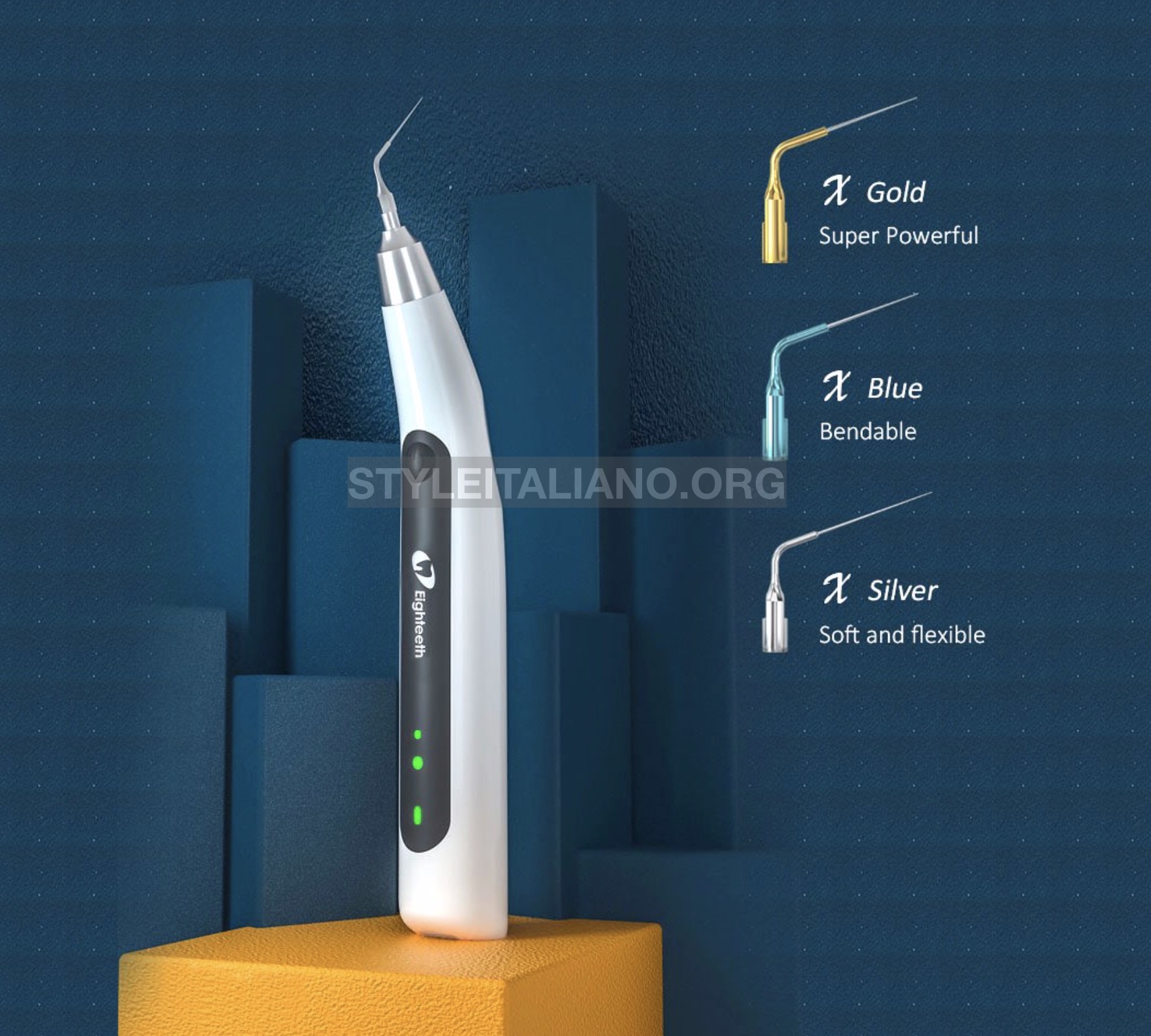
Fig. 9
Irrigation with NaOCl 5.25%, EDTA 18% solution, PUI activation (passive ultrasonic irrigation) using Eighteeth Ultra-X with the blue tip (Changzhou Sifary Medical Technology Co., Ltd., China).

Fig. 10
Obturating MB canal to the level beyond perforation site by CWC (Continuous wave compaction) of Gutta Percha, using Eighteeth Fast-Pack (Changzhou Sifary Medical Technology Co., Ltd., China).

Fig. 11
Introducing MTA to the site of perforation, by the aid of MAP System (Produits Dentaires, Switzerland). The rest of MB canal was filled with MTA.

Fig. 12
Obturation of P and DB canals Gutta Percha cones and BioCeramic Sealer using Modified Hydraulic Obturation (250 C for 2 seconds) with Fast-Pack, then Backfilling with Eighteeth Fast-Fill (Changzhou Sifary Medical Technology Co., Ltd., China).
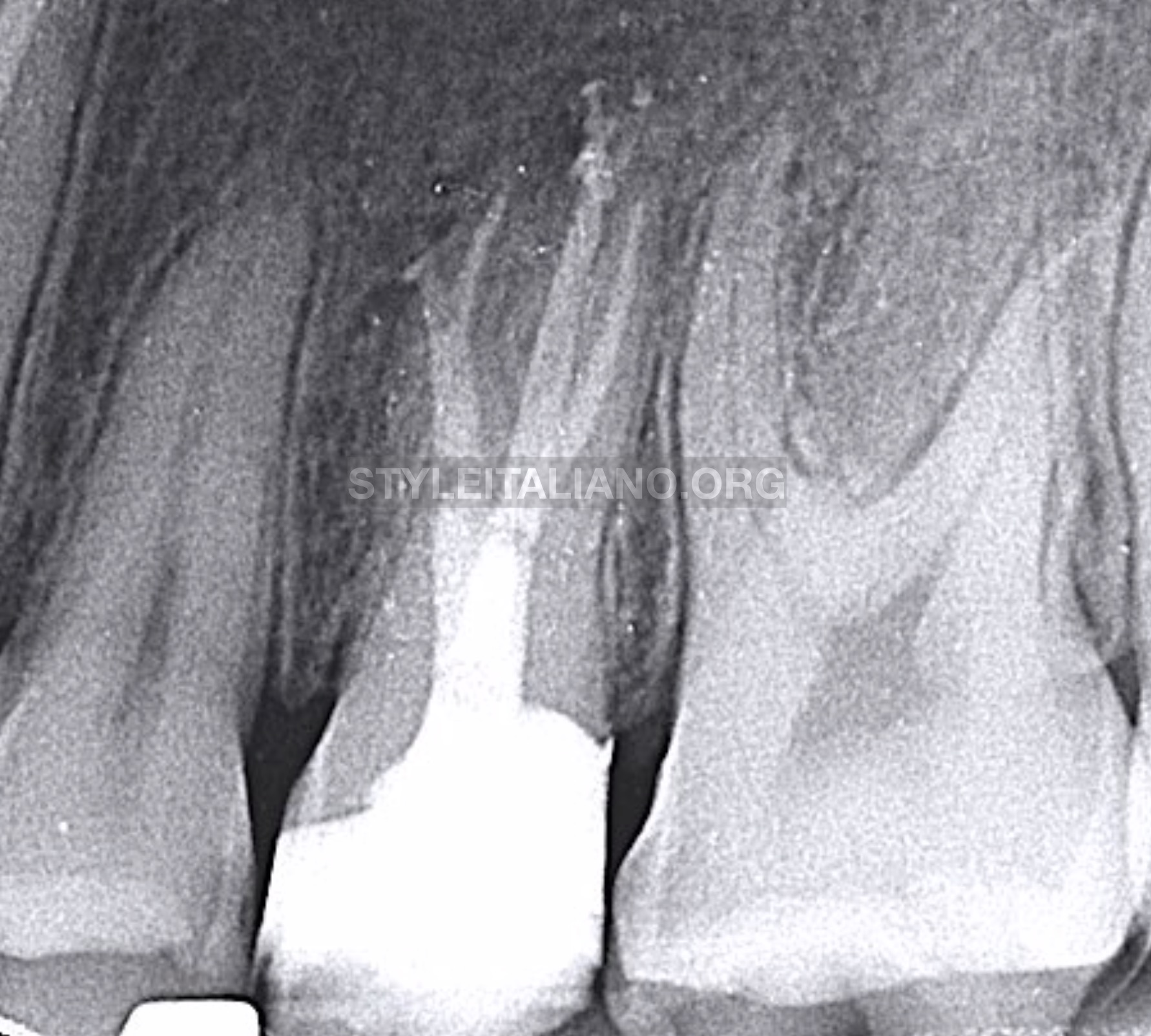
Fig. 13
Final radiograph showing obturation of the three canals, in addition to the perforation site. Core build up with composite.
The patient has been scheduled for coronal coverage.
Conclusions
It is well-known that bacteria is the primary etiological factor in the development of pulpal and peri-apical lesions (Kakehashi et al. 1965). Ørstavik and Pitt Ford (2008) described the aim of root canal treatment is “to prevent or cure apical periodontitis”. The steps of achieving this goal is by decreasing the level of bacteria (and their toxins) in the complex root canal system as low as possible through a chemo-mechanical debridement (Bystrom et al.1981, Siqueira Jr. and Rôças 2008, Wong 2004, Basmadjian‐Charles et al. 2002), and then filling the root canal system with a well adapted root canal filling capable of preventing reinfection of the root canal space and leakage of residual bacteria and bacterial products into the peri-apical tissues (Basrani and Haapasalo 2012). Preoperative radiograph plays an important role in the diagnosis and in the treatment planning (Gröndahl and Huumonen 2004). A preoperative radiograph showing full roots and at least 2-3 mm of periapical region is mandatory before prompting with the root canal treatment (ESE 2006).
In this reported case, the previous treatment was not succeeded mainly due to the inability to interpret the anatomy of the root canal system by preoperative radiograph, which led to improper execution of the treatment, inability to cure patient’s pain and comfort, more difficult re-treatment, more periapical tissue damage, more tooth structure loss in re-treatment, and more costs and chair-side time for the patient.
Pre-operative radiograph is of a great importance to confirm our primary diagnosis (collected by patient’s history and clinical examination), to make our treatment plan, and as a baseline to assess our outcomes in reviewing.
Bibliography
- Basmadjian‐Charles CL, Farge P, Bourgeois DM and Lebrun T (2002) Factors influencing the long‐term results of endodontic treatment: a review of the literature. International Dental Journal, 52(2), 81-86.
- Basrani B and Haapasalo M (2012) Update on endodontic irrigating solutions. Endodontic topics, 27(1), 74-102.
- Bystrom A and Sundqvist G (1981) Bacteriologic evaluation of the efficacy of mechanical root canal instrumentation in endodontic therapy. Scand J Dent Res, 89, 321–328.
- Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG (2007) Endodontic Applications of Cone-Beam Volumetric Tomography. Journal of Endodontics, 9, 1121-32.
- European Society of Endodontology (2006) Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. International Endodontic Journal, 39(12), 921-930.
- Forsberg J (1987a) Radiographic reproduction of endodontic ‘working length’ comparing the paralleling and the bisecting-angle techniques. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics, 64, 353-60.
- Forsberg J (1987b) A comparison of the paralleling and bisecting-angle radiographic techniques in endodontics. International Endodontic Journal, 20, 177-82.
- Gröndahl HG and Huumonen S (2004) Radiographic manifestations of periapical inflammatory lesions: how new radiological techniques may improve endodontic diagnosis and treatment planning. Endodontic topics, 8(1), 55-67.
- Kakehashi S, Stanley H, Fitzgerald R (1965) The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surg Oral Med Oral Pathol, 20, 340–349.
- Ørstavik D, Pitt Ford TR (1998) Apical Periodontitis: Microbial infection and host responses. In: Essential Endodontology: prevention and treatment of apical periodontitis. Oxford: Blackwell Science, 1-8.
- Patel S, Dawood A, Whaites E, Pitt Ford T (2009) New dimensions in endodontic imaging: Part 2. Cone beam computed tomography. International Endodontic Journal, 42, 447-62.
- Siqueira Jr. JF and Rôças IN (2008) Clinical implications and microbiology of bacterial persistence after treatment procedures. Journal of endodontics, 34(11), 1291-1301.
- Wong R (2004) Conventional endodontic failure and retreatment. Dental Clinics of North America, 48(1), 265-289.