Saving Two Mandibular Molars
03/03/2022
Ahmed Shawky
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The Primary objective of endodontic treatments is treatment and/or prevention of apical periodontitis. To achieve this goal, the endodontist must be able to process all the case givens to reach a conservative and predictable treatment.
This articles describes the decision making process in non-surgical retreatments of two mandibular molars throughout the endodontic workflow.

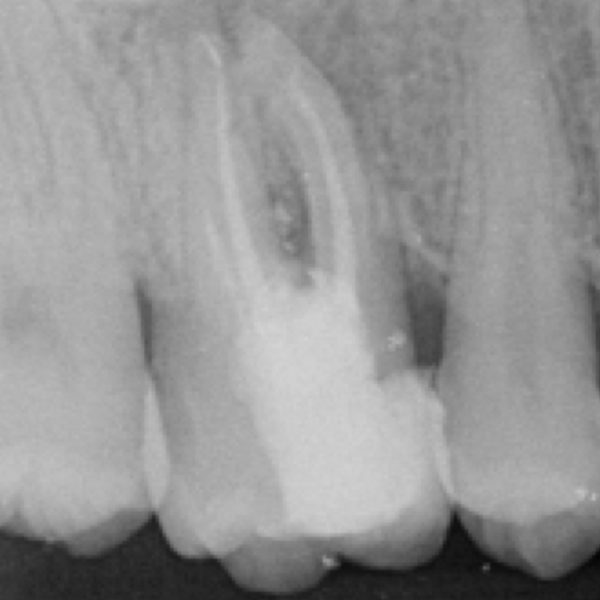
Fig. 1
A female patient came complaining of severe pain related to the mandibular left area.
Clinical and radiographic evaluation revealed the presence of symptomatic apical periodontitis related to a previously treated mandibular left second molar. The tooth was restored with a full coverage PFM restoration with a long retention element “screw post” in the distal root.
The patient was informed that the adjacent molar might be causing a potential problem due to the presence of improper treatment and the presence of over-extended long broken file in the mesial root.
The patient was consented about the proposed treatment which was “Non-surgical retreatment” of the second molar.

Fig. 2
Disassembly of the extra-coronal restoration was performed by sectioning using high speed diamond for the porcelain layer followed by a carbide trans-metal tool.

Fig. 3
The first visit involved disassembly of the long screw post using medium power ultrasonics, as well as gross removal of the gutta percha mechanically to facilitate decompression and drainage if possible.
Non-setting calcium hydroxide with iodoform was placed as a temporary dressing to promote dryness of the weeping canals, reducing symptoms and disinfection of the root canals
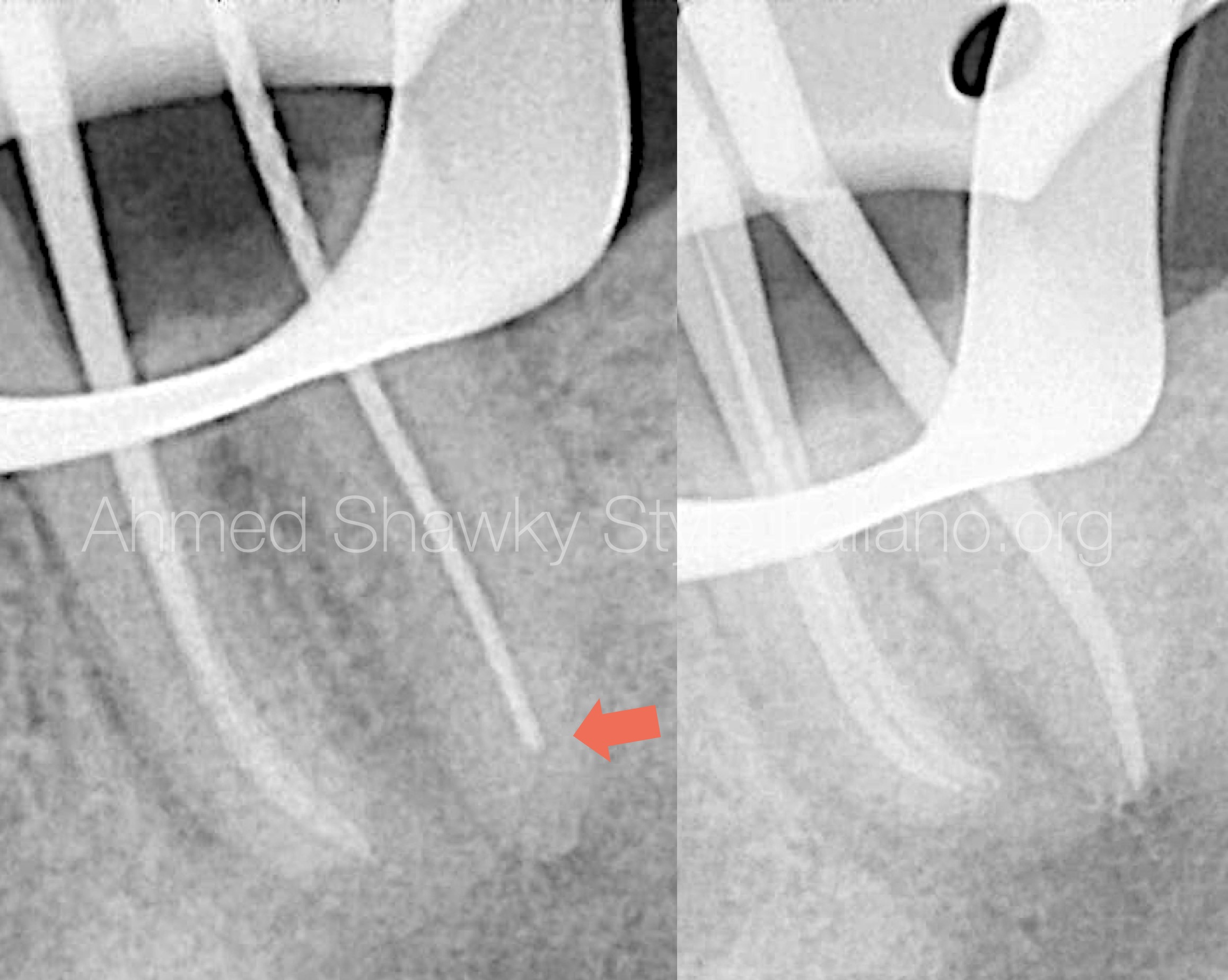
Fig. 4
After 14 days, the patient returned symptom-free.
During root canal procedures, the distal root was judged to have inflammatory resorption in the apical part. This was confirmed by using the apex locator which gave apical reading 3 mm short of the radiographic apex (Arrow). Also gauging of the distal foramen revealed a foramen size greater ISO 50
A decision was made to seal the distal root with an apical plug, while the mesial root would be sealed with warm gutta percha and heat-compatible Bioceramic sealer.

Fig. 5
Placement of 5 mm apical plug.
A resorbable collagen matrix was placed exactly at the apex (outside the root) using a pre-fitted plugger and an apex locator.
A dedicated MTA carrier was used to deliver the premixed putty Bioceramic into the distal root canal, followed by packing using gutta percha cone and the blunt end of a tapered paper point.
Radiographic confirmation revealed sharp placement of the apical plug.

Fig. 6
The patient returned after 8 months for treatment of the adjacent molar. A recall image was taken for the retreated second molar. Radiographic evaluation revealed ongoing healing of the apical lesion
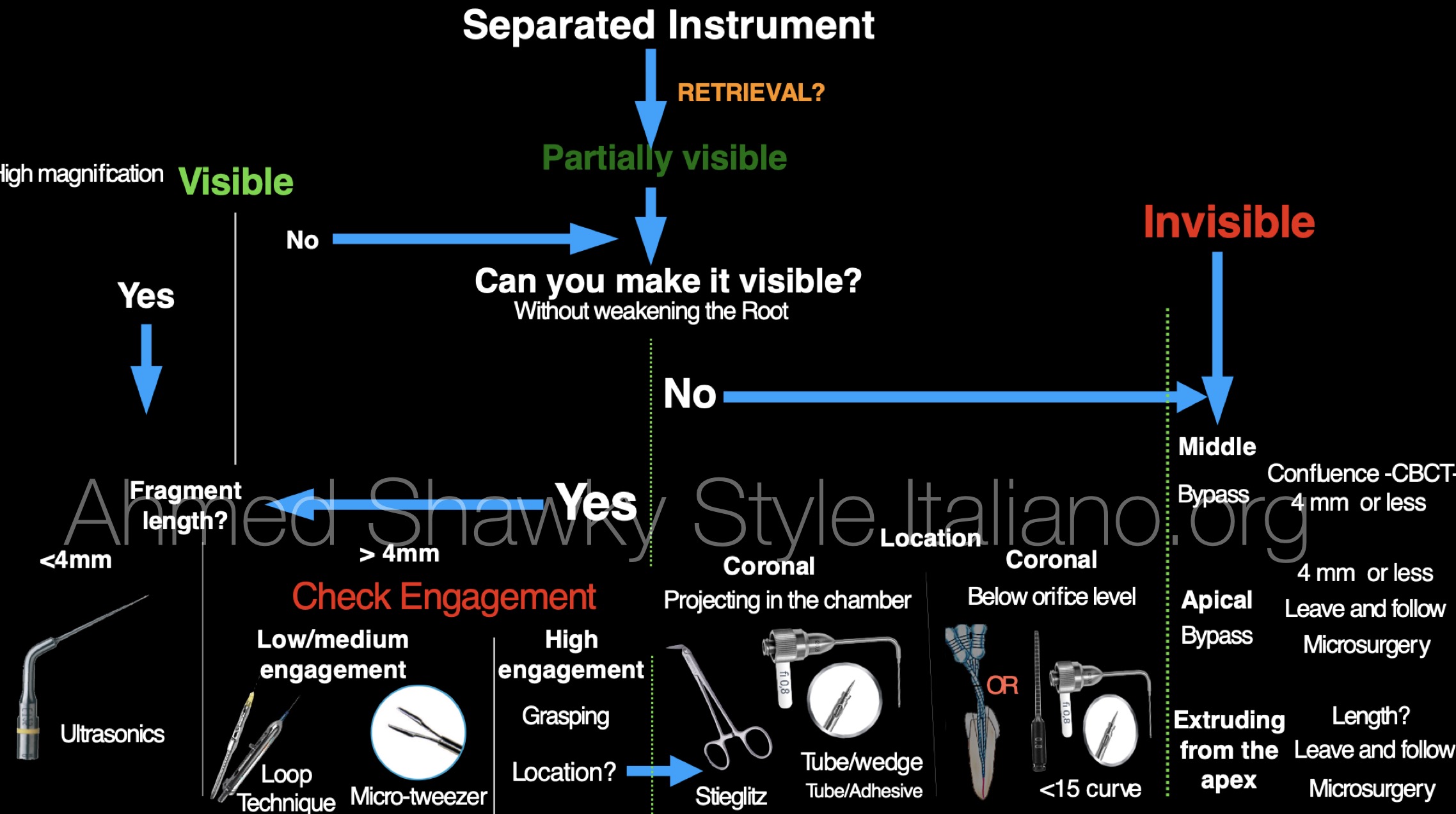
Fig. 7
Retreatment of the molar with a long broken file extruding through the apex
Disassembly of the PFM was performed similar to the second molar. The tooth was isolated and the screw post in the first molar was removed using ultrasonics. After removal of the post, the isolation was re-adjusted to start the retrieval of the extruded long fragment in the mesio-buccal root canal.
Attempts to reduce the engagement of the broken Hedstrom file was performed using low-power ultrasonics to avoid secondary fractures and/or heat generation, until the coronal part of the fragment was slightly movable. An attempt to retrieve the fragment using loop technique was performed. This attempt failed in retrieval due to strong engagement of the file
An attempt to retrieve the fragment using loop technique was performed. This attempt failed in retrieval due to strong engagement of the file
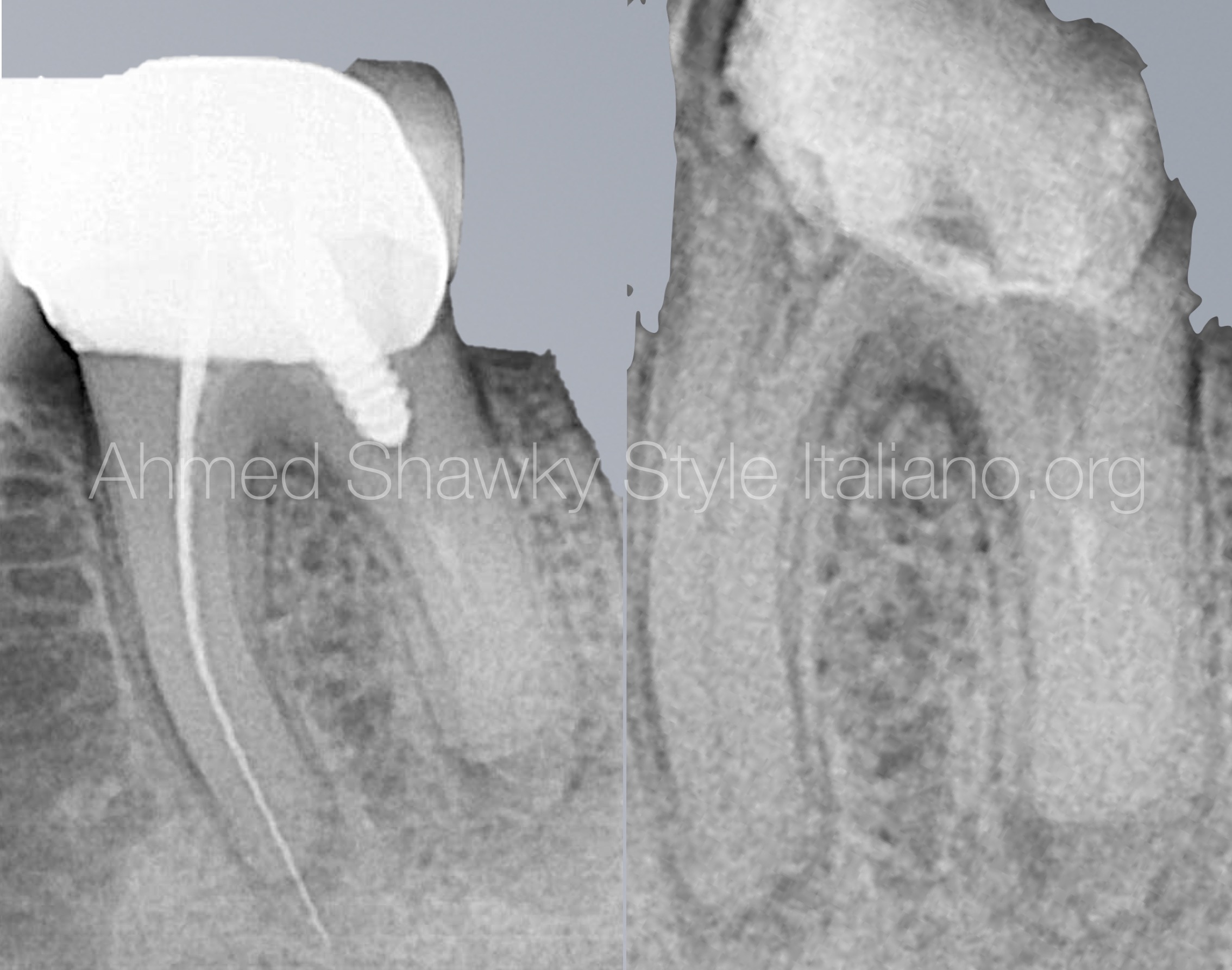
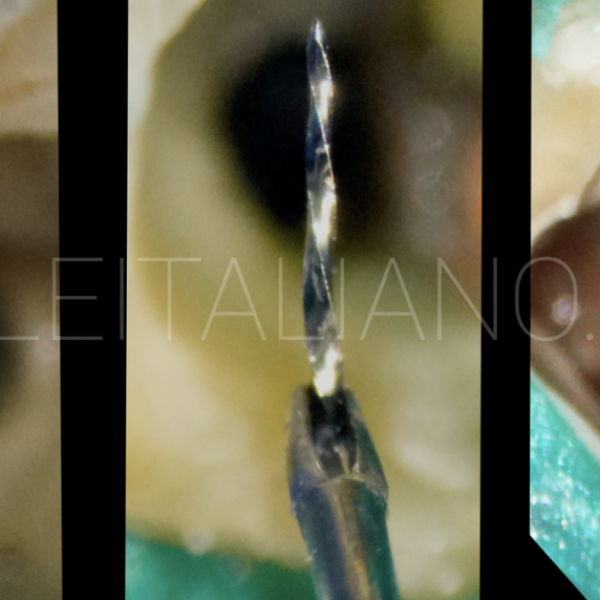
Fig. 8
Grasping the long, Highly Engaged fragment
Due to strong engagement of the broken file, further ultrasonic troughing was done followed by grasping the free head of the instrument by a Stieglitz plier using a wiggling maneuver until the long extruded fragment was successfully retrieved
Retrieval with Stieglitz plier

Fig. 9
After removal of cements and GP from the canal walls using ultrasonics, a missed ML canal was located followed by mechanical (Manual-less) shaping of the root canal system.
The tooth was obturated using warm gutta percha and heat-friendly Bioceramic sealer
The tooth was obturated using warm gutta percha and heat-friendly Bioceramic sealer
Conclusions
Conclusion:
Different treatment approaches can be selected in two adjacent teeth aiming to achieve the ultimate goal of non-surgical retreatment.
Bibliography
- Schilder H. Cleaning and shaping the root canal. Dent Clin North Am. 1974; 18: 269-296
- Schilder H. Filling root canals in three dimensions. Dent Clin North Am. 1967; : 723-744
- Reit C. Grondahl H.G. Management of periapical lesions in endodontically treated teeth: a study on clinical decision making. Swed Dent J. 1984; 8: 1-7