
Endodontic Flare-up
19/04/2017
Paolo Generali
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The occurrence of pain and/or swelling after an endodontic treatment is not uncommon in endodontic practice, and can be a frustrating event for dentists and a disappointing surprise for patients.
As stated by the American Association of Endodontics Glossary, a flare up is defined as an “acute exacerbation of asymptomatic pulp or periradicular pathosis after the initiation or continuation of root canal treatment”. This adverse event may be a result of various factors, including mechanical, chemical and bacterial irritation. As a result, patients should be warned to expect a slight amount of discomfort following endodontic therapy. Procedural errors, as overinstrumentation, inadequate debridement, or even misdiagnosis can be among the causative factors.

Fig. 1
The occurrence of pain and/or swelling after endodontic treatment is different in two circumstances: whether the pulp was vital before treatment or not. In the case of vital pulp, pain could be associated with the persistence of pulpal remnants in the root canals. This can happen as a consequence of missed canals, or of a less than optimal shaping and cleaning technique. Missed canals are often associated with a lack of accuracy in designing the access cavity. Besides the case of an erroneously short working length, the widespread use of standardised instrumentation can lead to underestimate the presence of oval shaped, or unusually wide canals. An inaccurate apical gauging and finishing of these canals can leave uncleaned canal space, and inflamed pulp remnants can cause pain.
Case 1: In this patient, persistent pain was present after endodontic treatment of a vital tooth. The periapical x-ray showed an inadequate shaping of the distal root canal, regarding both the working length and the apical taper.

Fig. 2
Retreatment of distal canal was performed using ProTaper retreatment files. Working length was assessed electronically. Canal was shaped with a Reciproc R40, thoroughly irrigated with US activation, filled with corresponding Guttafusion obturator. Pain disappeared completely some days after retreatment. In all likelihood, incomplete preparation allowed residual pulp tissue to remain in the root canal, acting as an irritant.
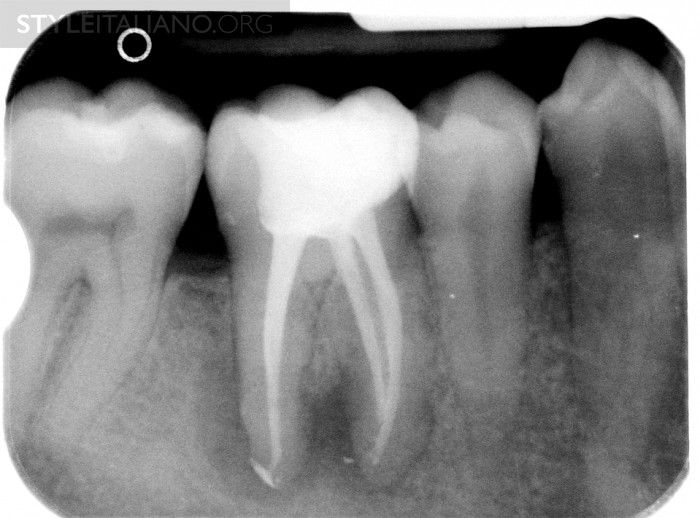
Fig. 3
The frequency of post-endodontic pain is higher in teeth with periapical or periradicular lesions. Infected debris can be forced in the periradicular tissue through a resorpted apex, thus generating acute inflammation. Creating a glide path prior to instrumentation and using a step-down technique can reduce the amount of extruded debris.
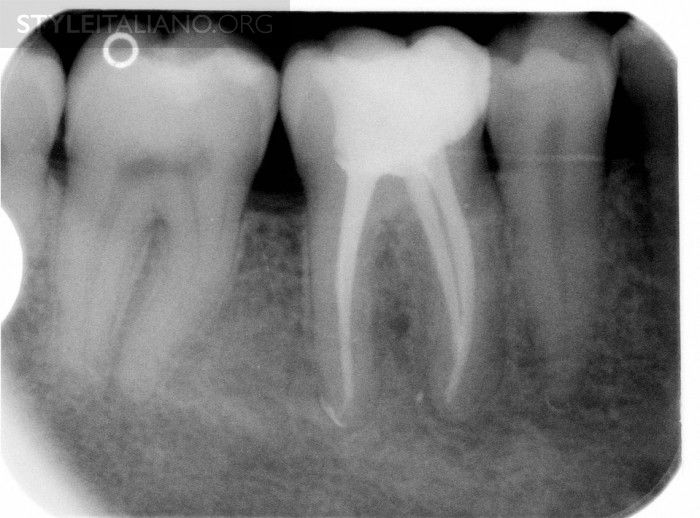
Fig. 4
Case 2: This necrotic first mandibular molar was treated in one visit, and the patient complained of post-operative pain. Analgesics and antibiotics were prescribed, and occlusion relieved. Symptoms disappeared after two days, and a radiographic follow-up after two years showed healing of the periradicular lesion.

Fig. 5
Missing canals means being unable to remove irritant or infected debris from the endodontic space, often causing persistent pain.
Case 3: This patient was referred for assessment of a first mandibular molar, after an attempted endodontic treatment. Mesio-lingual, mesio-buccal and one distal canal were scouted and filed and a calcium hydroxide temporary dressing was used before referral, but pain persisted. Eventually, most of the temporary obturation material was lost at the time of the visit.

Fig. 6
A careful examination of the pulp chamber floor showed the presence of a middle mesial canal in the mesial root

Fig. 7
And two canals in the distal root

Fig. 8
Endodontic treatment was completed and pain subsided.
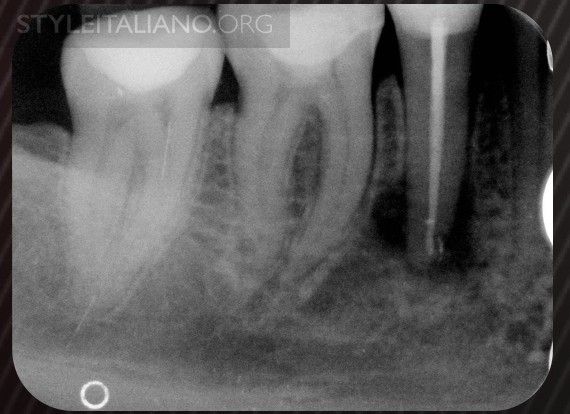
Fig. 9
Case 4: Another common cause of pain after a completed endodontic treatment is tooth fracture. This adverse event is most likely to occur if a restoration with cuspal coverage is not provided. Thereafter, waiting for the complete healing of an endodontic lesion prior to perform cusp coverage is dangerous.

Fig. 10
A crown-root fracture occurred while waiting for complete healing of periapical lesion.
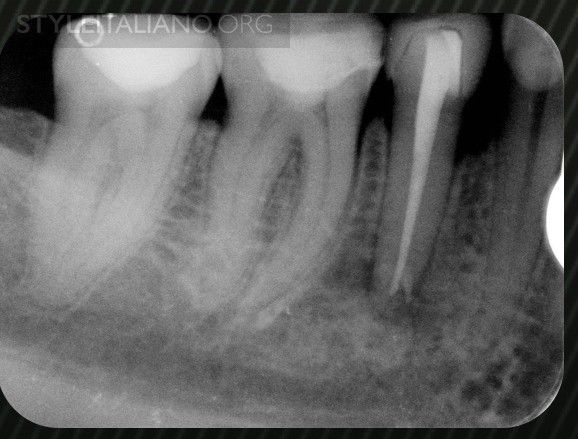
Fig. 11
Luckily, this case was still restorable, despite a minor loss of attachment.

Fig. 12
A full ceramic crown provides function, aesthetics and a ferrule effect, so it was chosen as the best option for this case.
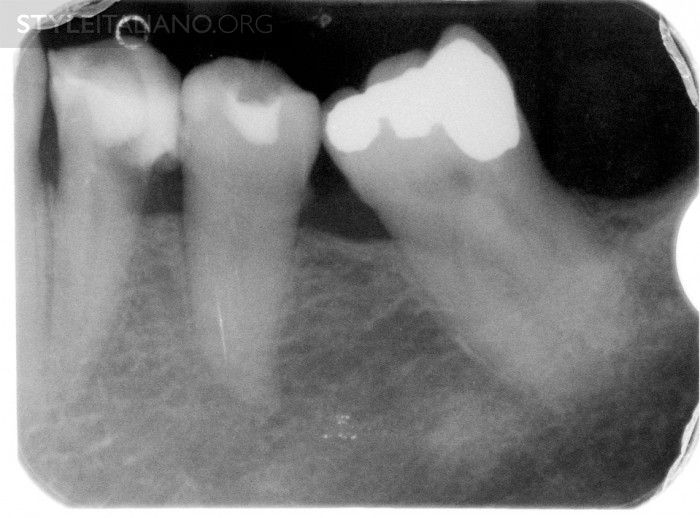
Fig. 13
In every case of post-endodontic pain, diagnosis must be assessed carefully, because sometimes pain may be coming from a nearby tooth.
Case 5: This patient came complaining of pain located in the lower left jaw; he had undergone pulpectomy of both premolars without success. In an attempt to find the root canal of the first premolar, an iatrogenic perforation occurred. The patient was referred to our practice for persistent and exacerbating pain. The patient complained pain upon chewing and percussion at premolars and molar, we could not find response to thermal and electric stimuli at premolars, while the molar hurted sharply with cold, no response to heating, pain at low voltage with electric pulp tester.

Fig. 14
The clinical picture was suggesting a misdiagnosis, and the most likely cause was a cracked tooth syndrome of the molar. The amalgam filling of the molar was removed and a crack appeared.

Fig. 15
Endodontic treatment and cuspal coverage of the molar were performed and pain subsided. Premolars were endodontically treated, also with a calcium hydroxide dressing. Perforation was filled with bioceramic. A perio-restorative procedure was proposed for a permanent restoration of perforated premolar, but patient refused.
Conclusions
Flare-up is a relatively common adverse event of endodontic treatment, and most frequently caused by infection. It causes anxiety and doubts both to the patient and to the dentist. Patients should be advised that a certain amount of pain and discomfort is possible after an endodontic treatment, and that this does not mean treatment failure. Prevention of acute exacerbation of endodontic pathology is accomplished first with a careful diagnosis. All the several conditions that can simulate odontogenic pain should be considered and excluded, and the tooth responsible of symptoms precisely identified. A complete endodontic record chart, including pulp testing results, can be helpful in treating future complications. Then, in case of infection, the administration of a short-term antibiotic prophylaxis before treatment should be considered, despite controversial literature findings. Furthermore, endodontic technique is of utmost importance: access opening, scouting for all canal accesses, irrigation, pre-flaring, glide path, step-down protocol are among the factors helpful in preventing apical extrusion of debris. Working length control, apical gauging and finishing allow the complete removal of irritants from the apical third. A safe irrigation technique, including the use of dedicated, side-vented endodontic needles, never too close to the apex, is mandatory. Irrigant activation increases the efficacy of chemical-physical debridement of inaccessible areas of the root canals, thus reducing the amount of irritants. After the completion of shaping and cleaning procedures, if the canal can be successfully dried with paper points, and apical patency is present, then the canal can be obturated, avoiding overextension. In the case of persistent exudation, obturation should be postponed. CaOH dressing can be helpful in maintaining disinfection, avoiding bacterial recontamination and proliferation. Prescription of analgesics is suggested in the case of hot tooth, and in selected patients.
If the patient needs a visit for the occurrence of pain after treatment, then diagnostic procedures should be repeated. A flare-up may be caused by several factors, the most frequent being infection. Occlusion should be checked and relieved. If the previous endodontic procedure has been completed, the written records and x-rays should be revised critically. If in doubt, retreatment should be performed; if all the procedures have been accomplished at their best, then the patient should be reassured, explaining in plain language that there is nothing dangerous and that a rapid recovery can be expected. Antibiotics and analgesics should be prescribed, and another visit scheduled after a few days for re-evaluation. Corticosteroid administration, via intraoral injection, is a safe and effective procedure. Endodontic surgery can be an option. Despite literature data, an extreme method for the treatment of an acute exacerbation of periapical pain is trephination: under anaesthesia, the cortical bone adjacent to the apex of the affected tooth is perforated with a sterile bur, and the periapical exudate is released. Leaving access cavity open for drainage should be considered as the most direct way towards additional contamination and, eventually, tooth extraction.
Bibliography
American Association of Endodontists. Glossary of endodontic terms, 9th ed. Chicago: American Association of Endodontists; 2016.
Torabinejad M, Kettering JD, McGraw JC, Cummings RR, Dwyer TG, Tobias TS. Factors associated with endodontic interappointment emergencies of teeth with necrotic pulp. J Endod. 1988;14:2616
Siqueira JF, Barnett F. Interappointment pain: mechanisms, diagnosis, and treatment. Endodontic Topics 2004, 7, 93109
Tsesis I, Faivishevsky V, Fuss Z, Zukerman O.Flare-ups after endodontic treatment: a meta-analysis of literature. J Endod. 2008 Oct;34(10):1177-81






