Treatment of an invasive external resorption
18/01/2024
Federico Ceroni
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
External resorptions are degenerative processes of the dental tissue which, if not intercepted in time, can lead to the loss of the dental element.
The diagnosis can be complicated and are sometimes confused with dental cavities.
To treat this type of problem, it is essential to know how to correctly diagnose it and treat it following a precise protocol.the difference that can be perceived between dental caries and resorption is that in the first case the lesion has more defined margins compared to resorption if we are analyzing an intraoral x-ray. We will then have the confirm of the diagnosis by carrying out a cone beam CT scan. to perform a correct treatment plan we will have to evaluate the periodontal, endodontic and residual tooth substance situation. the treatment plan will therefore be multidisciplinary.

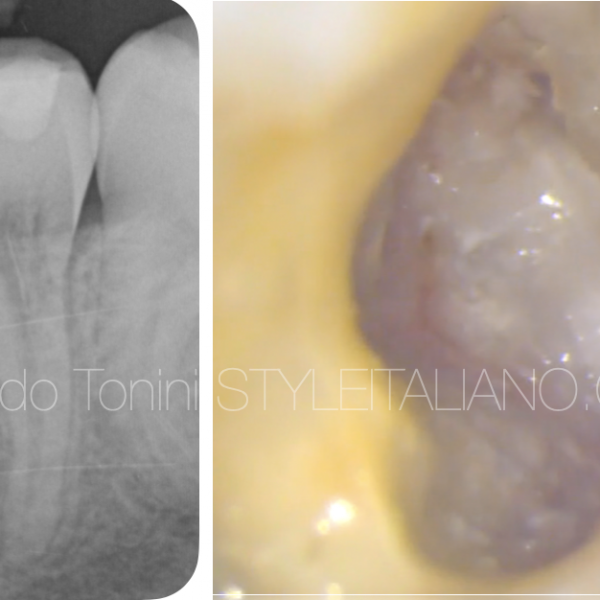
Fig. 1
A 27 yrs old woman came to our office complaining discomfort related to the first upper left premolar.
The bitewing X-ray shows a degenerative process eroding the dental tissue in the disto-cervical portion of tooth 26.
At this moment we are not able to understand whether the problem is a carious process or a resorption for this reason we decide to perform a CBCT.

Fig. 2
Once the CBCT is performed, the presence of invasive external resorption in the distal-cervical portion of the tooth is clear.
The lesion is also positioned at bone level, the portion of healthy tissue once the cavity has been cleaned will therefore be very deep.
Biologically, a distance of 3 mm is recommended between the restorative margins and the alveolar crest in order to avoid detrimental effects on neighboring soft and hard periodontal tissue: unfortunately in this case the distance was not respected, so a crown lengthening was chosen to restore the tooth.
The treatment of this tooth will consist of performing a clinical crown lengthening and a pre-endo build up, followed by root canal treatment, composite restoration.

Fig. 3
Crown lengthening and pre end build up. After opening a flap and repositioning the bone level, the tooth was isolated with open flaps and the distal wall was reconstructed with composite.

Fig. 4
In a second appointment, after the rubber dam placement, the endodontic treatment was performed.
The working length was checked radiographically and the subsequent irrigation protocol consisted in 5,25% NaOCL and 17% EDTA. The canal was dried and the filling was performed with warm vertical condensation.

Fig. 5
Then a composite restoration was performed
A total etch adhesive procedures was done, etching for 30 sec the enamel and 15 sec the dentin, then a three step etch and rinse adhesive system was placed and lightcuring for at least 30 sec.
Then the composite restoration with a nano hybrid composite was layered.

Fig. 6
This is the result 1 month later. As you can see, the periodontal tissue its healthy and the coronal part of the papilla regrew, meaning that the treatment was performed correctly.

Fig. 7
After the six-months follow up the case will be finalized with an indirect adhesive restoration.
Conclusions
Tooth resorption is a pathological phenomenon that can linger unnoticed for several years and we still know little about it.
Most of tooth resorption cases exhibit no symptoms. Timely identification of resorption is crucial for effective treatment.
A well-thought-out strategy prior to intervention holds significant value, and a multi-disciplinary approach is almost always required in all cases.
Bibliography
Patel S, Mavridou AM, Lambrechts P, Saberi N. “External cervical resorption: part 1 - histopathology, distribution and presentation”. Int Endod J 2018 Nov 51(11):1205-1223
Patel S, Foschi F, Condon R, Pimentel T, Bhuva B. “External cervical resorption: part 2 - management: External Cervical Resorption”. Int Endod J 2018 Dec(12):1224-1238Patel S,
Foschi F, Mannocci M, Patel K. “External Cervical Resorption: a three dimensional classification”. Int Endod J 2018 Feb:51(2):206-214
Gold SI, Hasselgren G. Peripheral inflammatory root resorption: a review of the literature with case reports. J Clin Periodontol 1992;19:523–34.
Mavridou AM, Hauben E, Wevers M, et al. Understanding external cervical resorption in vital teeth. J Endod 2016;42:1737–51.