Treatment of an external inflammatory root resorption
26/06/2025
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
External inflammatory resorption (EIR) is present on the external surface of the root of majority of the teeth diagnosed with chronic apical periodontitis. EIR also affects teeth that suffer severe dental traumatic injury (for example, avulsion and luxation). In dental trauma injury cases, EIR occurs as a result of injury to the root surface and adjacent periodontium. It is initially self‐limiting and only focussed on the damaged root surface. Consequently, the loss of pulp vitality and infection of the necrotic pulp can result in the progression of EIR.
The clinical features of EIR are irreversible pulpitis and/or apical periodontitis such as pain, swelling, tenderness to percussion or palpation, sinus tract and discolouration. The affected tooth usually has a negative response to pulp sensitivity test
The diagnosis of EIR is confirmed on radiographic findings. EIR due to solely infected necrotic pulp contents may appear to be shorter or stunted in appearance than normally expected and sometimes have a ragged margin at the root end and associated with periapical radiolucency adjacent to the affected root . The root end may also have a ragged appearance.
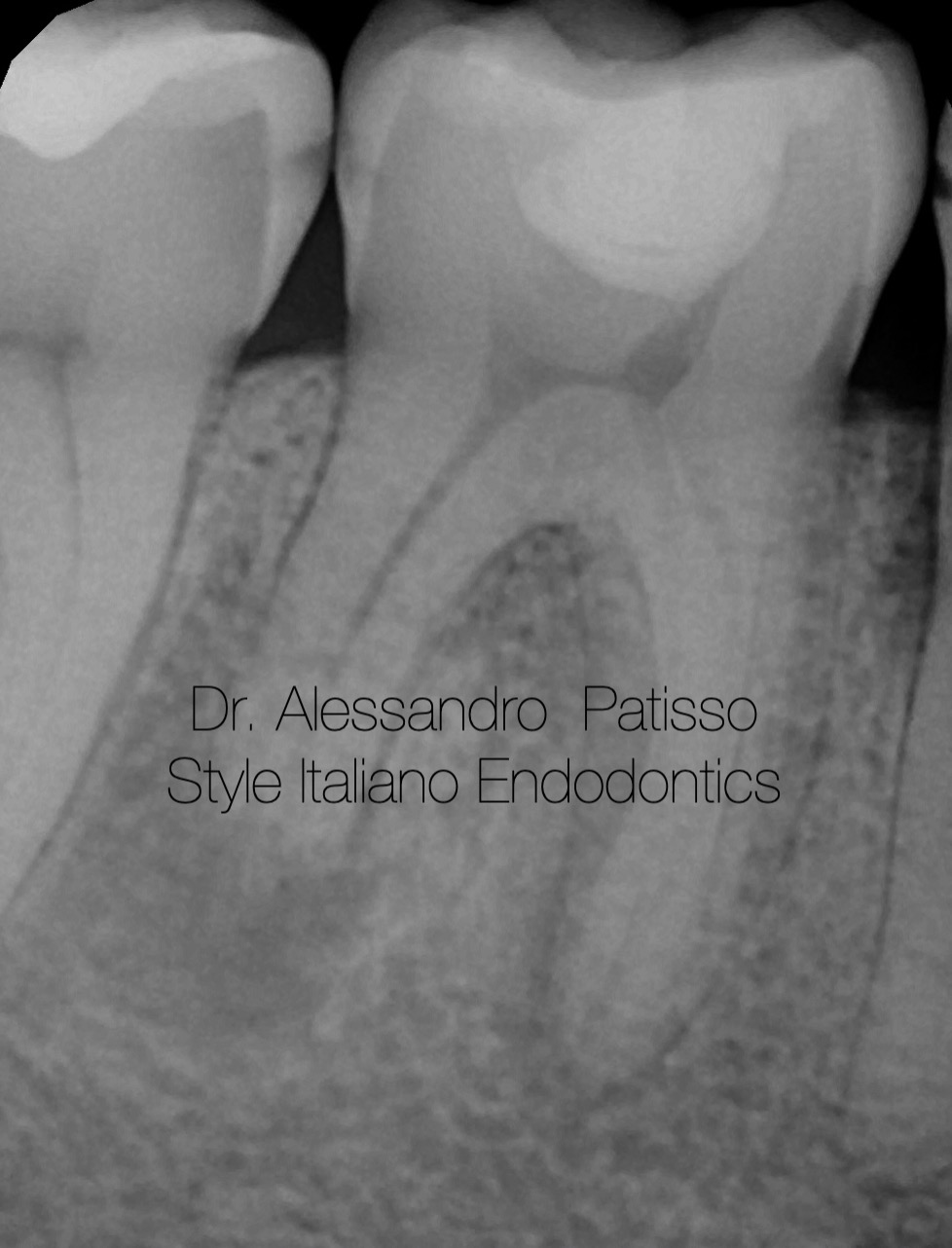
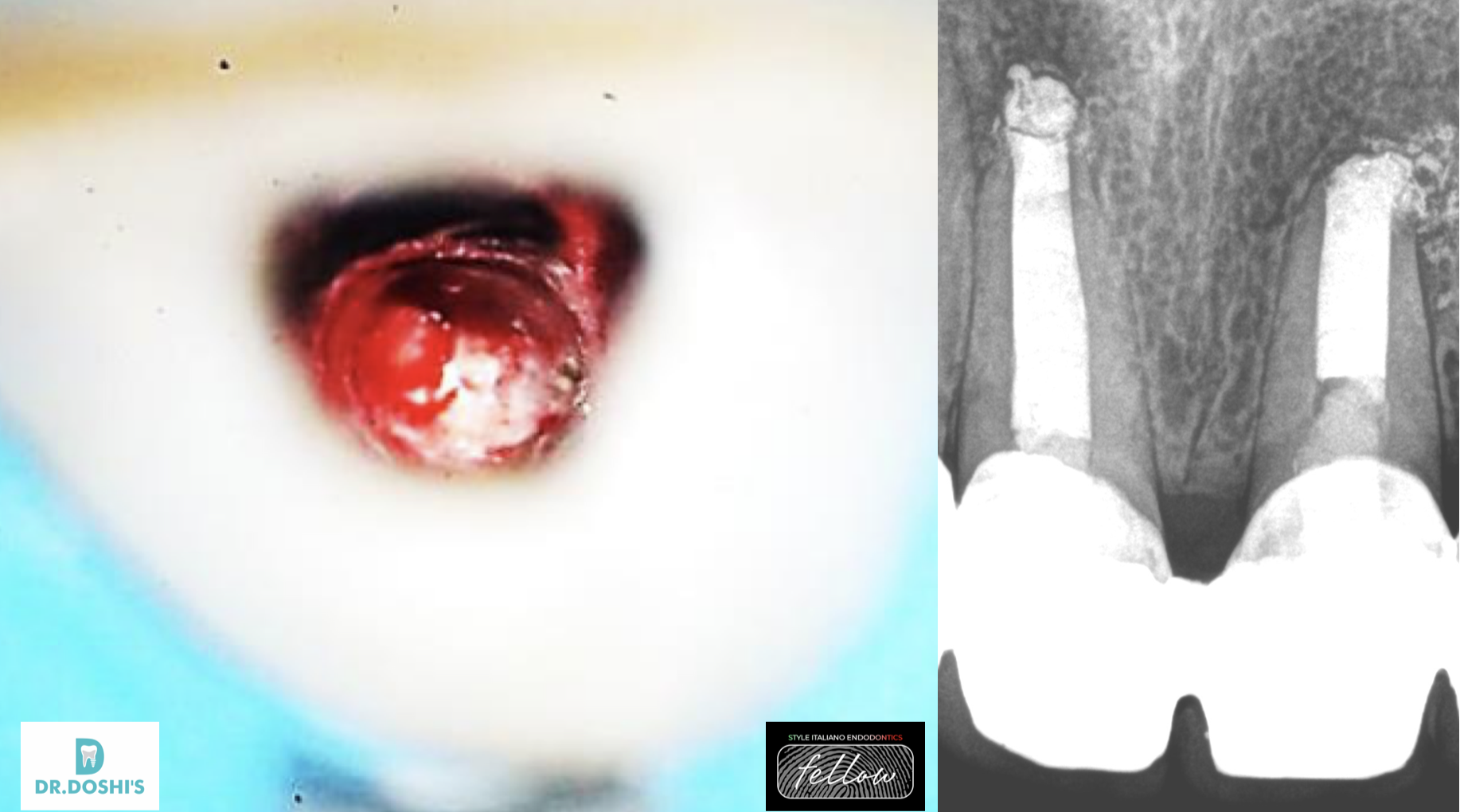
Fig. 1
Fig. 1
Case of tooth 46, male, 35 years old, referred to our clinic due to a case of external root resorption with periapical lesion.
A periapical radiograph, revealing periradicular bone loss and periapical radiolucency associated with external
inflammatory resorption on the apical‐third of tooth 46
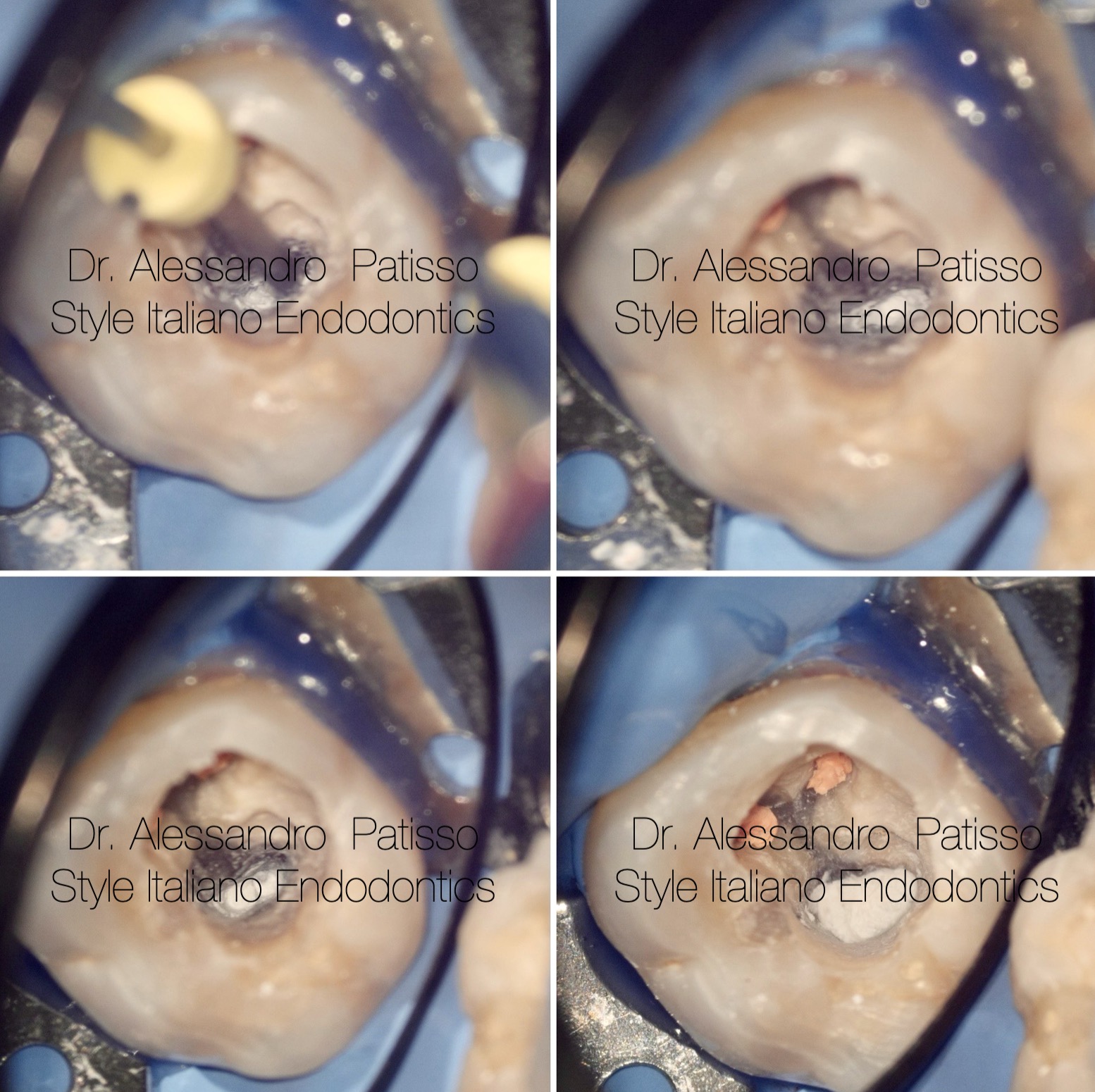
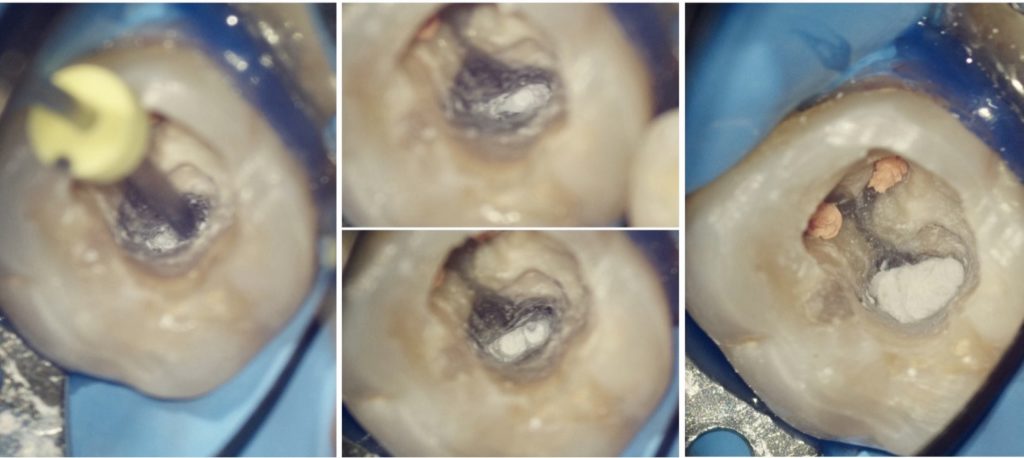
Fig. 2
MAP system was used to put Bioceramic PUTTY material for obturation IN THE DISTAL CANAL
FOR THE MESIAL I USED A three-dimensional hot obturation system allowed me to seal the entire root canal with the gutta percha.(BIOCONELESS)

Fig. 3
POST OP XRAY
Root canal treatment will eliminate the stimulating factors (microbes and their toxins) and arrest the resorptive process, thus preventing further damage on the root, at the same time allowing hard tissue repair of the damaged root surface.

Fig. 4
Follow up at 2 years, bone healing was evident, tooth was asymptomatic.

Fig. 5
Graduated in Dental Hygiene at the University of Bari in 2009 and Dentistry and Dental Prosthetics at the Universidad Europea de Madrid in 2015.
From the beginning he has practiced exclusively Clinical Edodontics, perfecting himself through numerous courses around Italy. Among the most recent he attended the courses of Dr Giuseppe Carrieri, finishing first in the course.
Today he works as a freelancer using only the microscope. Tutor in the courses of Dr Giuseppe Carrieri Fellows member Styleitaliano Endodontics.
Conclusions
Robust clinical research is required to gain a deeper knowledge of the aetiology and pathogenesis of the various types of root resorption.
The importance of a thorough and systematic clinical and radiographic examination is paramount to ensure appropriate management. The prognosis of root resorption is dependent on an accurate and early diagnosis. Increasingly, CBCT is being used to confirm the diagnosis and/or aid management.
Bibliography
- Abella, F. , Ribas, F. , Roig, M. , González Sánchez, J.A. & Durán‐Sindreu, F. (2018) Outcome of autotransplantation of mature third molars using 3‐dimensional‐printed guiding templates and donor tooth replicas. Journal of Endodontics, 44, 1567–1574.
- Acar, A. , Canyürek, U. , Kocaaga, M. & Erverdi, N. (1999) Continuous vs. discontinuous force application and root resorption. The Angle Orthodontist, 69, 159–163, discussion 163–154. Ahlberg, K. , Bystedt, H. , Eliasson, S. & Odenrick, L. (1983)
- Long‐term evaluation of autotransplanted maxillary canines with completed root formation. Acta Odontologica Scandinavica, 41, 23–31.
- Gold SI, Hasselgren G. Peripheral inflammatory root resorption: a review of the literature with case reports. J Clin Periodontol 1992;19:523
- Mavridou AM, Hauben E, Wevers M, et al. Understanding external cervical resorption in vital teeth. J Endod 2016;42:1737–51.
- Fuss, Z., Tsesis, I., & Lin, S. (2003). Root resorption - diagnosis, classification and treatment choices based on stimulation factors. Dental Traumatology, 19(4), 175–182.
- Haapasalo, M., & Endal, U. (2006). Internal inflammatory root resorption: the unknown resorption of the tooth. Endodontic Topics, 14(1), 60–79.
- Heithersay GS. Management of tooth resorption. Australian Dental Journal. 2007 Mar 1;52(s1).
- Patel, S., Ricucci, D., Durak, C., & Tay, F. (2010). Internal Root Resorption: A Review. Journal of Endodontics, 36(7), 1107–1121.
- Gabor, C., Tam, E., Shen, Y., & Haapasalo, M. (2012). Prevalence of Internal Inflammatory Root Resorption. Journal of Endodontics, 38(1), 24–27.