The management of two mandibular molars with apical inflammatory root resorption
03/06/2021
Alexandru Gliga
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Apical pathology can appear as a straightforward diagnosis, however the tools available for assessment come across different limitations. Histology has highlighted various aspects that can not be yet coherently linked to a clinical situation using imaging investigations (Ricucci, Mannocci & Pitt Ford, 2006).
Inflammatory root resorption makes no exception and reveals itself on periapical x-ray investigations in less than 20% of cases however the histology analysis confirms that resorptive defects are present in more than 80% of the cases (Laux et al., 2000). Hence there is a considerable chance for many clinicians to have been treating apical root resorption without being aware of it.
Severe apical root resorption is more likely to be noticed even with panoramic x-ray since the osteoclasts have removed enough cementum and dentine and the root morphology has dramatically changed. Although in these cases there is a possibility to proceed with the root canal therapy examining periapical X-ray only (as it will be presented for the first case of this article) there are many advantages in the assessment, treatment planning and performance if a pre-operative CBCT is available (second case).

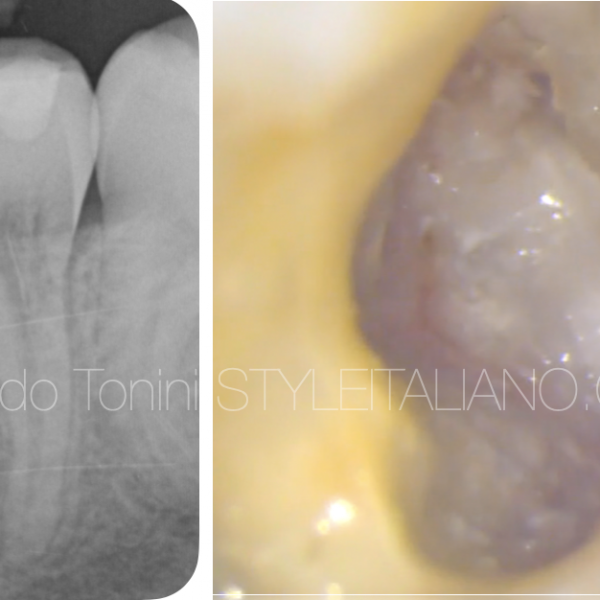
Fig. 1
The 30 years old patient was referred to our office by his wife, who attended regularly our dental practice. He complained about acute suffering pain and swelling with great sensitivity on biting associated with tooth 36 for the last 2 weeks.
When presented to his first visit, the patient had already begun an antibiotic treatment. Although the medication had managed the acute symptoms the patient was not very confident in keeping the tooth.
It is not easy to talk about prognosis considering the related pathology, however the final decision was to perform the endodontic treatment and aim to retain the patient’s lower left first molar.
The treatment was done in 3 visits, 60 - 90 minutes each. The first appointment was for instrumentation, irrigation and medication (Ca(OH)₂ was placed in the canals between visits). The endodontic treatment was completed during the second visit and the last appointment was dedicated to the coronal restoration.

Fig. 2
Rubber dam was secured over tooth 36 with a #7 rubber dam clamp (Hygenic Fiesta) and liquid rubber dam was used to ensure the isolation.
The access cavity was drilled using a round carbide bur through the composite core. The pulp chamber was fully accessed and refined using a stainless steel diamond coated ultrasonic tip with and without water spray.
The MB canal was negotiated and then instrumented with R25 (VDW). The working lengths of the canals were determined using an apex locator (VDW Gold). The ML canal had an open apex, could not determine the MAF, even with the second series files. For the distal canal GG nr. 3 and 4 and a stainless steel diamond coated ultrasonic tip were use for mechanical instrumentation.

Fig. 3
The following step was removing the granulation tissue found in the distal canal and manage the bleeding.
The mesial canals were prepared with reciproc technic at the full working length, with R25 files (VDW), following the previous obdurate path.
Irrigation was performed with 5.25% sodium hypochlorite (Cerkamed) and EDTA 17% (Endo-solution Cerkamed) during the preparation of the root canals. Activation of the sodium hypochlorite was carried out using ultrasonic tips U-files (Mani), and EDTA cream with Urea Peroxide.

Fig. 4
Apical gauging was verified with K-Files. MB canal was gauged to ISO size 25. Customised R25 gutta percha point was checked for their apical size and afterwords tried in the canal. Distal and ML canals could not be gauged.
During the second appointment the ML canal was apically plugged with MTA and back-filled with fluid gutta percha. On the distal canal a bleeding sponge was initially placed to create an apical barrier and perform the MTA plugging.

Fig. 5
Photo documentation on the direct composite restoration

Fig. 6
11-month recall shows notable healing process
and good coronal sealing

Fig. 7
36-month recall showing complete healing
The reason behind the direct restoration was the limited conviction for the outcome of the treatment. The restoration was placed free of charge asking the patient for follow-up in exchange. After the first year follow-up the patient was referred for a crown placement but he refused to change the restorative treatment.
The patient has been informed of the fracture risk but he decided, for the moment, to keep the composite restoration and continue attending the annual recall.
Although a success, altered root canal morphology in these cases requires a detailed assessment that can easily be obtained through CBCT investigation.

Fig. 8
Different views.
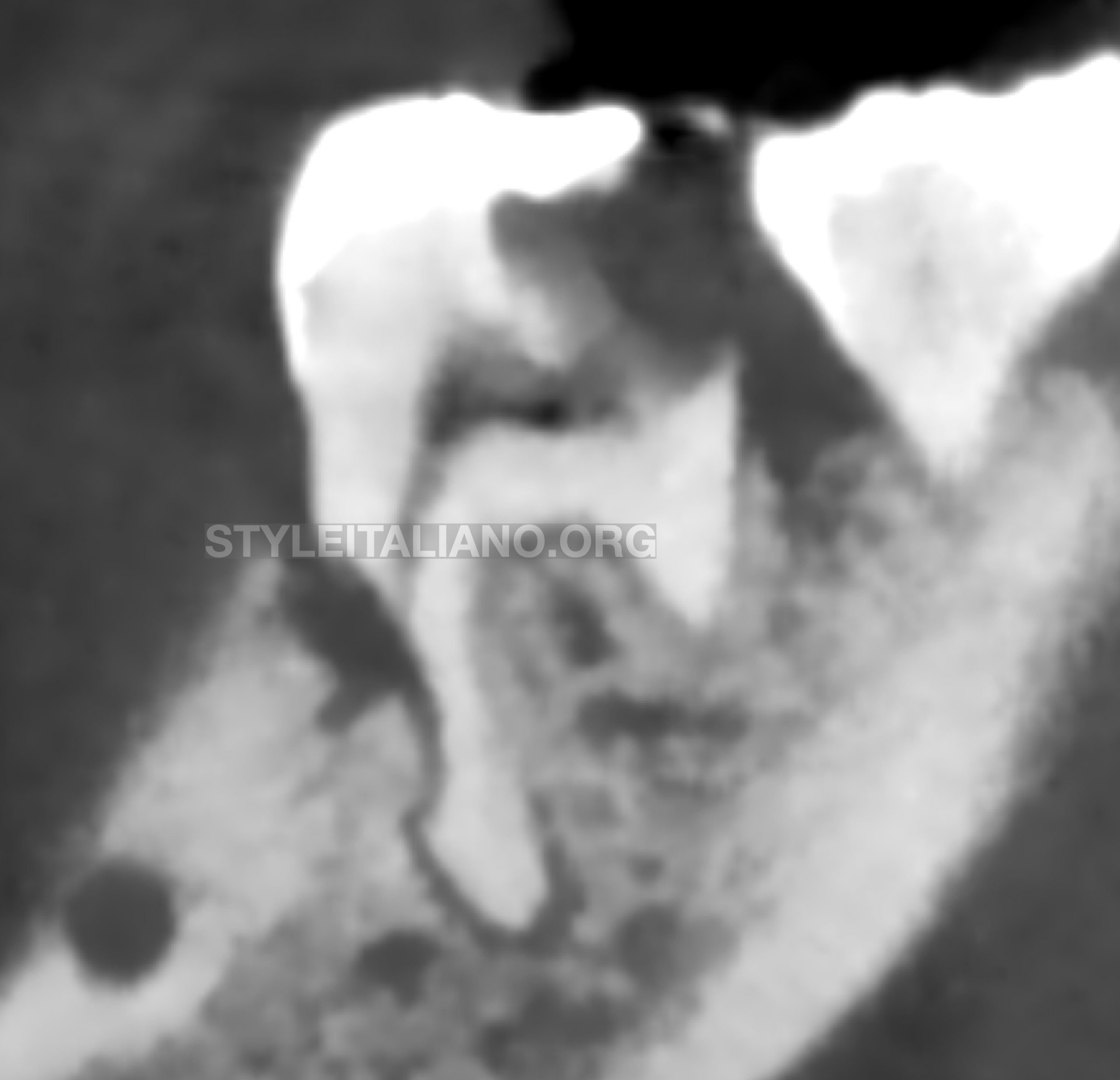
Fig. 9
The 24 years old patient was referred for endodontic treatment by his GDP. The patient accused acute suffering pain with great sensitivity on biting associated with tooth 36 and he also noticed the presence of a fistula.
A CBCT of the lower left first mandibular molar region revealed a root resorption and an apical pathology on both 36 and 35 teeth (Figure 16).
The treatment was performed during 3 visits. The first appointment was for instrumentation, irrigation and medication (Ca(OH)₂ was placed in the canals between visits). The second one for finishing the endodontic treatment and the last one for a surgical approach of the mesial periodontal pocket.
Pre-op CBCT - sagittal view
Pre-op CBCT - sagittal view

Fig. 10
Rubber dam was secured over tooth 36 with a #7 rubber dam clamp (Hygenic Fiesta) and liquid rubber dam was used to ensure the isolation. (Figure 17)
The access cavity was drilled using a round carbide bur through the composite restoration and by removing the infected dentine. The pulp chamber was fully accessed and refined using a stainless steel diamond coated ultrasonic tip (SB1 tip; Woodpecker) with and without water spray. (Figure 18)
The ML canal was negotiated and then instrumented with R25 (VDW). The working lengths of the canals were determined using an apex locator (VDW Gold).
The MB canal had an open apex, the MAF was determined with the second series files.
The distal canal was very wide so no files could achieve a good instrumentation. The canal walls were mechanically prepared with a GG nr. 2 and 3 and a stainless steel diamond coated ultrasonic tip E5D
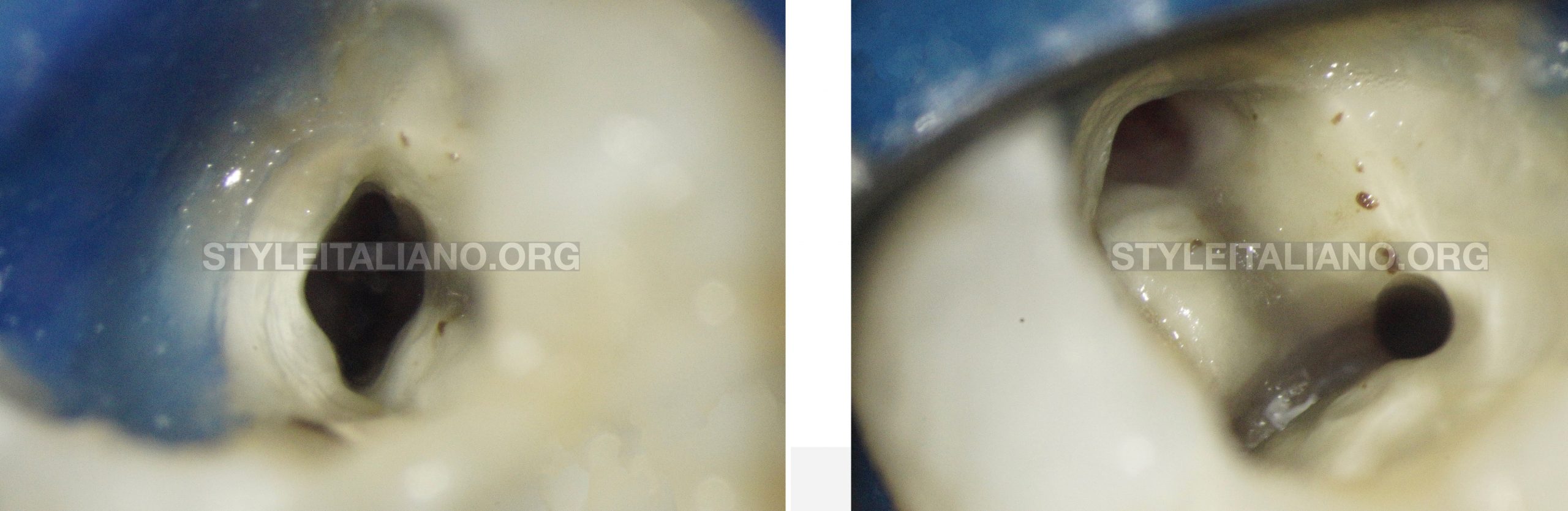
Fig. 11
The mesial canals were prepared with reciproc technic at the full working length, with classic R25 files (VDW).
Irrigation was performed with 5.25% sodium hypochlorite (Cerkamed) and EDTA 17% (Endo-solution Cerkamed) during the preparation of the root canals.
Activation of the sodium hypochlorite was carried out using ultrasonic tips U-files (Mani) and EDTA cream with Urea Peroxide.
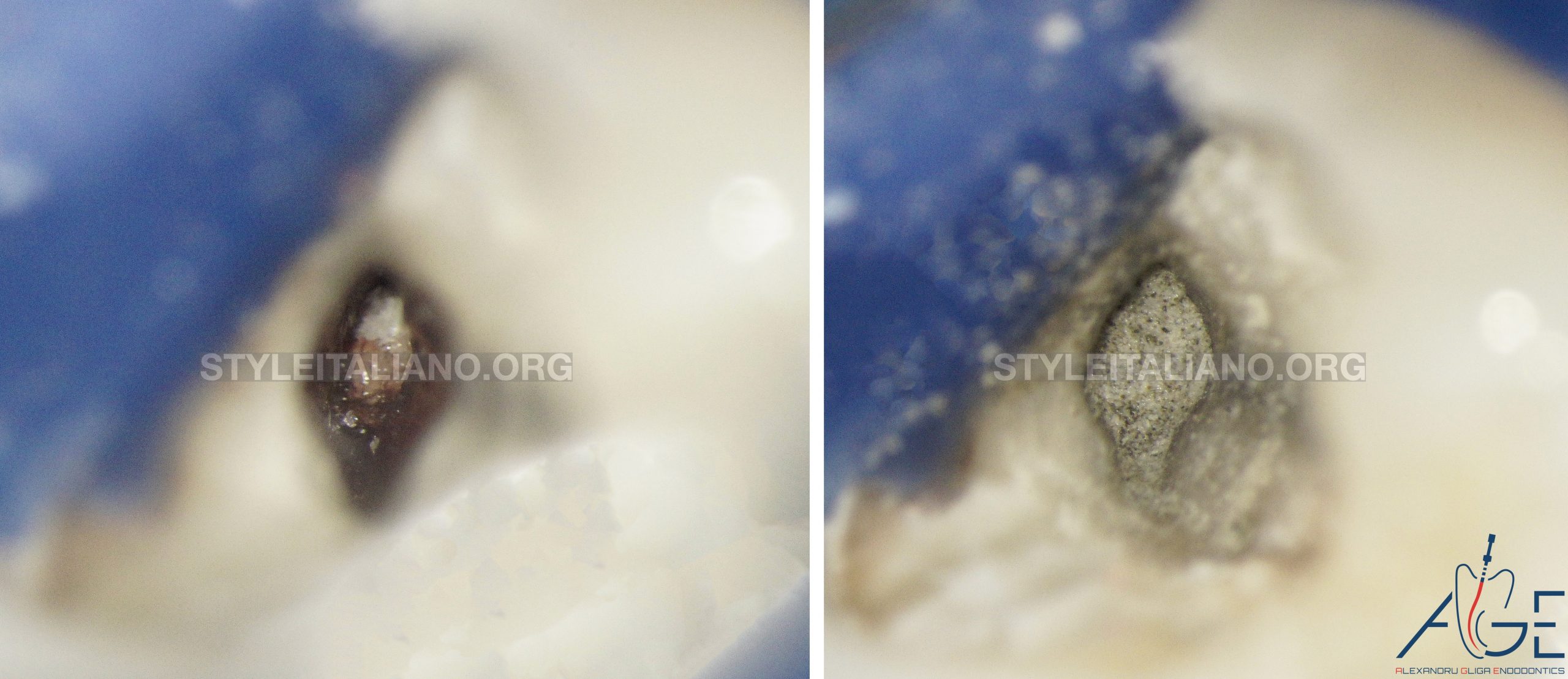
Fig. 12
On the distal and mesiobuccal canal a bleeding sponge was initially placed to create an apical barrier and safety perform the MTA plugging.
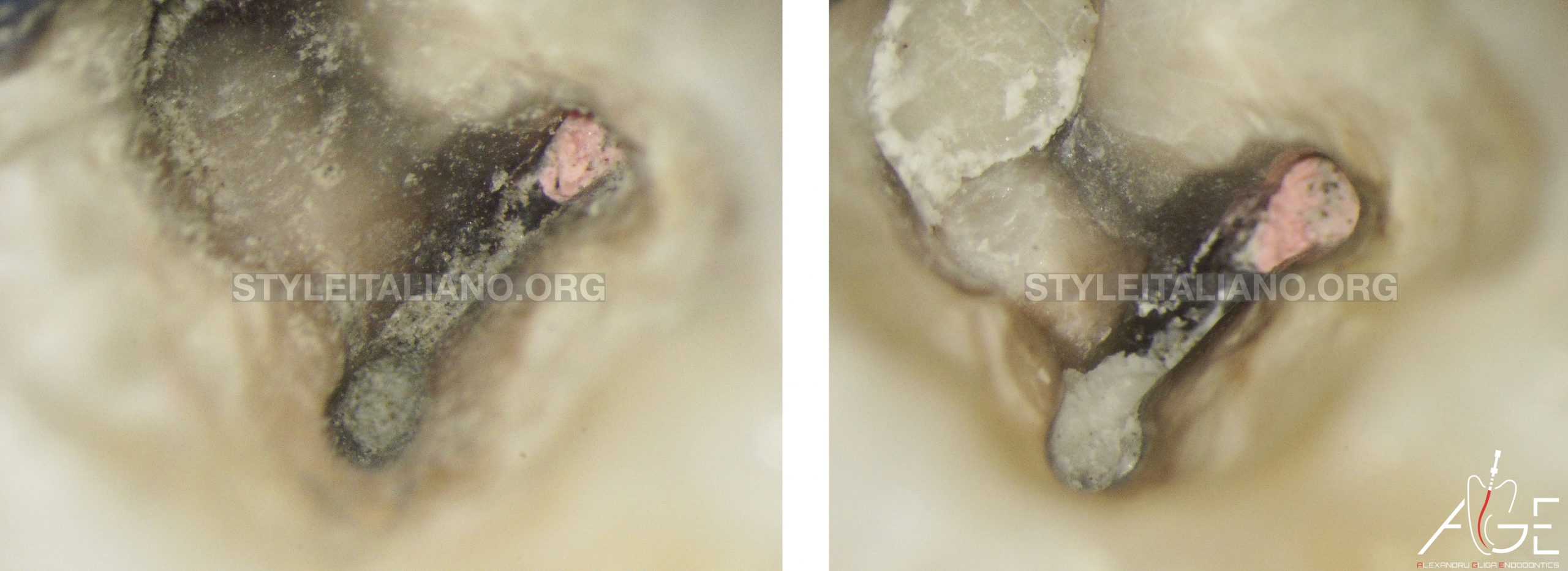
Fig. 13
GIC was placed on top of the MTA.
Periodontal surgery was performed between 36 and 35 endodontic treatments.

Fig. 14
Post-op X-ray tooth 36
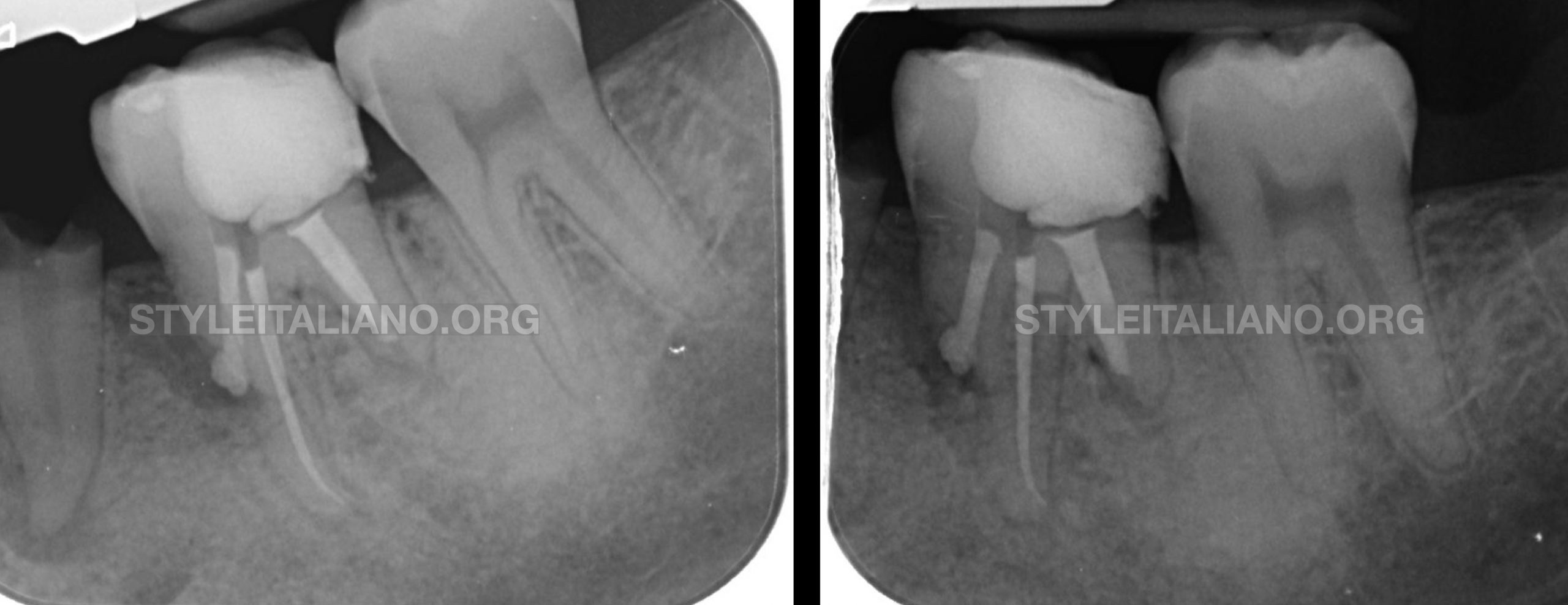
Fig. 15
final xray different projection
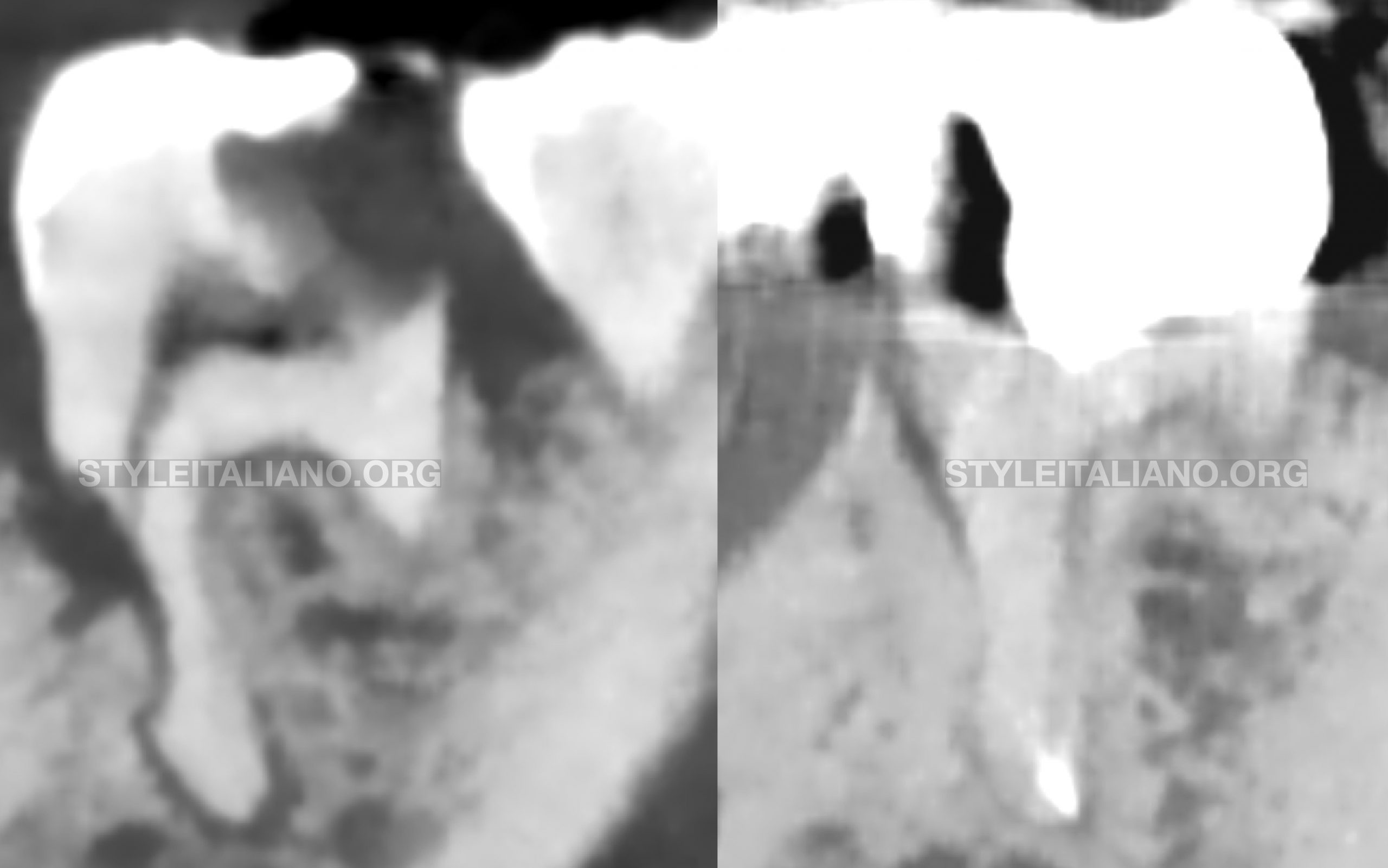
Fig. 16
Pre-op CBCT and
6 months follow-up
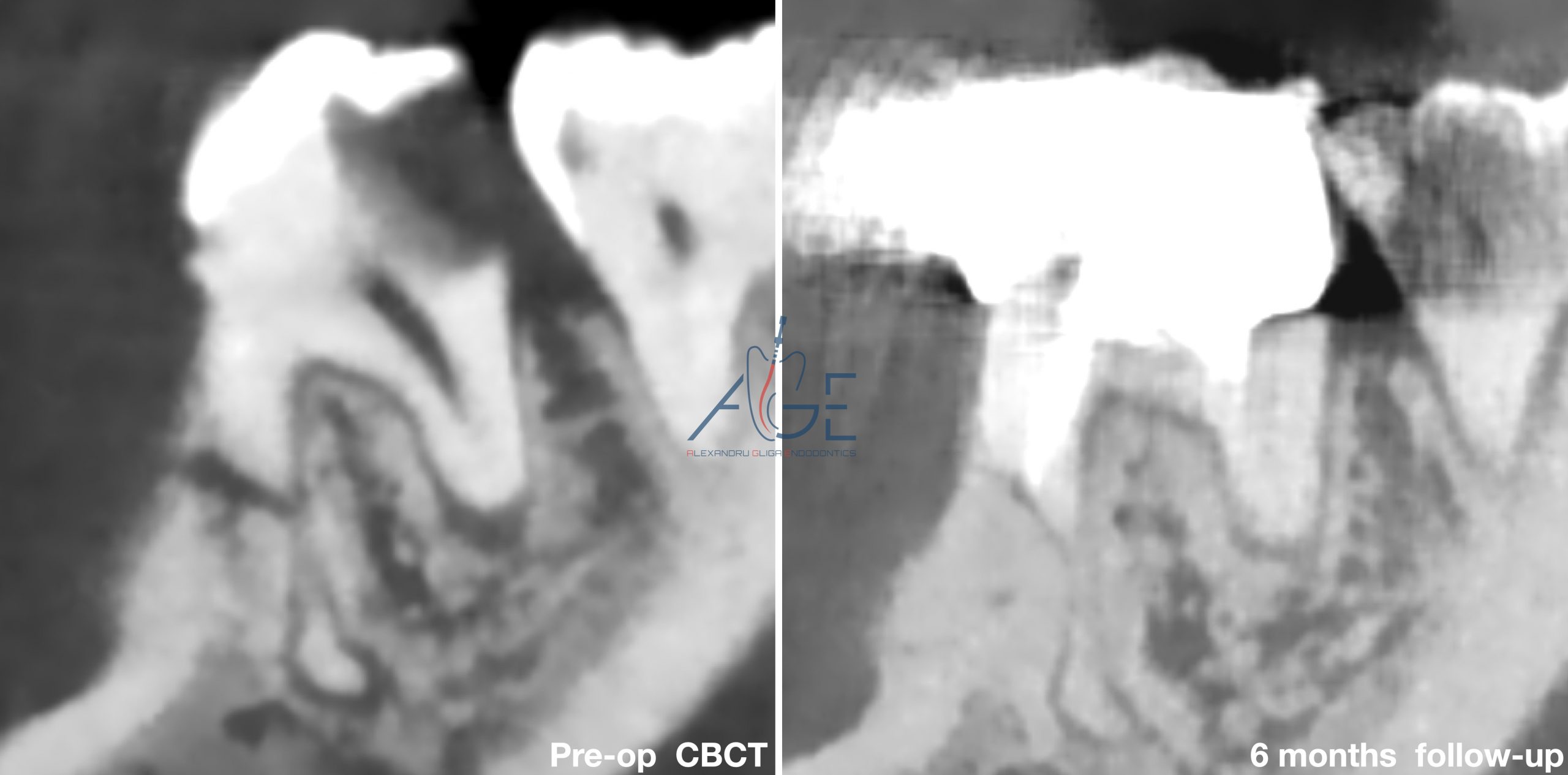
Fig. 17
Pre-op CBCT
6 months follow-up

Fig. 18
Pre-op CBCT and
6 months follow-up
Recall CBCT - sagittal view
Recall CBCT - axial view
Conclusions
Altogether, it might look like two straight forward re/treatments, but there is no clear protocol nor any specific technique published on the approach of cases with external root resorption for ensuring a defined predictable outcome (Ahangari et al., 2015). Cases like the ones presented request same attention as any apical pathology case does. Clinicians should mechanically and chemically clean the endodontic space as efficient as possible, intermediate medication is advertised and the sealing of resorbed canals should be carried out with bio-compatible materials.
In difficult cases like teeth with root resorption, CBCT examination is crucial for assessment, treatment planning and engagement. Navigating through a three-dimensional imaging allows the clinician not only to predict, but also to develop the future management and procedures.
Even though extraction or retrograde endodontic treatment is common in situations like the ones described, the outcome of orthograde endodontic therapy represents a major factor all clinicians should first consider.
Bibliography
Ahangari, Z., Nasser, M., Mahdian, M., Fedorowicz, Z. & Marchesan, M.A. 2015, "Interventions for the management of external root resorption", Cochrane Database of Systematic Reviews, , no. 11.
Cotti, Lusso & Dettori 1998, "Management of apical inflammatory root resorption: report of a case", International endodontic journal, vol. 31, no. 4, pp. 301-304.
Laux, M., Abbott, P.V., Pajarola, G. & Nair, P.N.R. 2000, "Apical inflammatory root resorption: a correlative radiographic and histological assessment", International endodontic journal, vol. 33, no. 6, pp. 483-493.
Ricucci, D., Mannocci, F. & Pitt Ford, T.R. 2006, "A study of periapical lesions correlating the presence of a radiopaque lamina with histological findings", Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, vol. 101, no. 3, pp. 389-394.