Surgical Flap in Endo Surgery - Part 1
06/05/2016
Fabio Gorni
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The selection of an appropriate flap design could determine the success of an endodontic surgery; therefore it's not possible to use a single flap design for different clinical situations and every flap has advantages and disadvantages: for this reason the pre-surgical planning is one of the most important phase of the treatment. The design of the flap will be conditioned by
1) Number of teeth involved
2) Position of the tooth
3) Shape, length and curvatures of the roots
4) Depth of vestibule
5) Muscle insertions and presence of the frenula
6) Presence and amount of attached gum
7) Periodontal biotype
8) Presence and depth of periodontal pockets
9) Dimension of the lesion
10) Anatomy structures nearby
11) Amount of bone covering the surgical target
12) Presence of crowns on the involved teeth
13) Aesthetic value of the areas
FLAP CLASSIFICATION
Sulcular flap
Semilunar flap
Triangular flap
Rectangular flap or trapezoidal flap
Submarginal scalloped flap
Submarginal straight flap
Papilla base flap
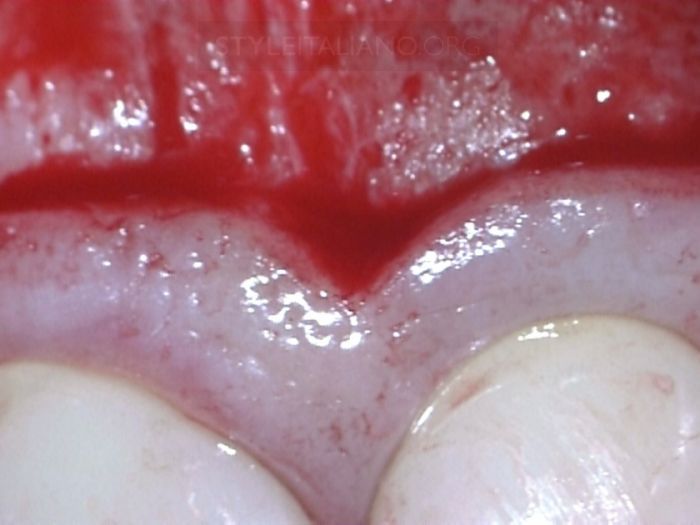
SUBMARGINAL SCALLOPED FLAP (Oshenbein-Leubke) The submarginal scalloped flap is a variant of the rectangular flap, the horizontal incision runs along the attached gingiva following the gingival scallops. The incision must not involve the gingival sulcus or periodontal pocket in order to avoid dehiscence and gum recessions.
Advantages: Simple to perform, simple to suture and allows an exact repositioning of the flap, avoid gum recession especially in aesthetic area and is the perfect in the presence of crowns. This flap guarantees a good access, also in case of long roots.
Disadvantages: this flap requires a good amount of attached gum and requires of careful periodontal evaluations to be performed correctly. The suture needs time and accuracy and a bad suturing can result in visible scars.
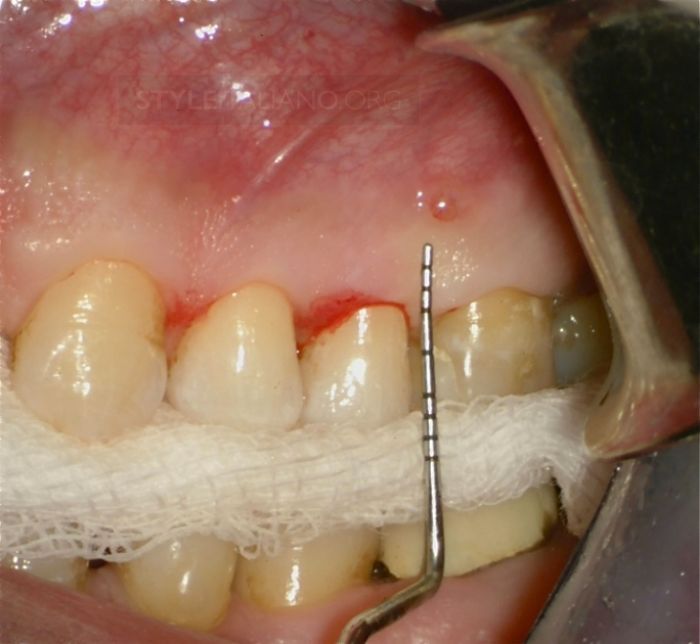
Fig. 1
PROBING AND FLAP DESIGN
At this stage a precise probing is very important in order to prevent the incision from involving the sulcus or periodontal pockets. The flap design must be trapezoidal and the base has to be larger than the horizontal incision. The flap does not involve frenulum or sinus tract.

Fig. 2

Fig. 3
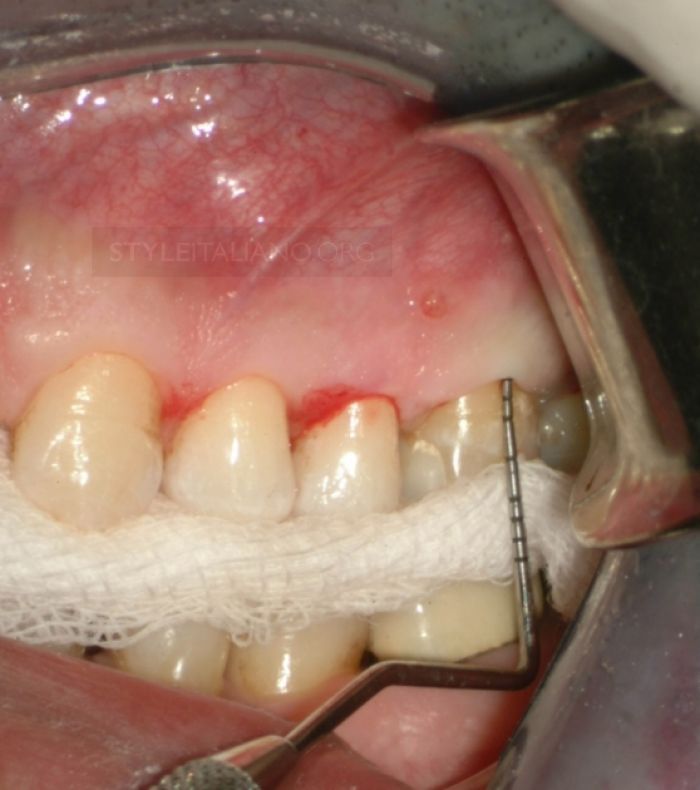
Fig. 4
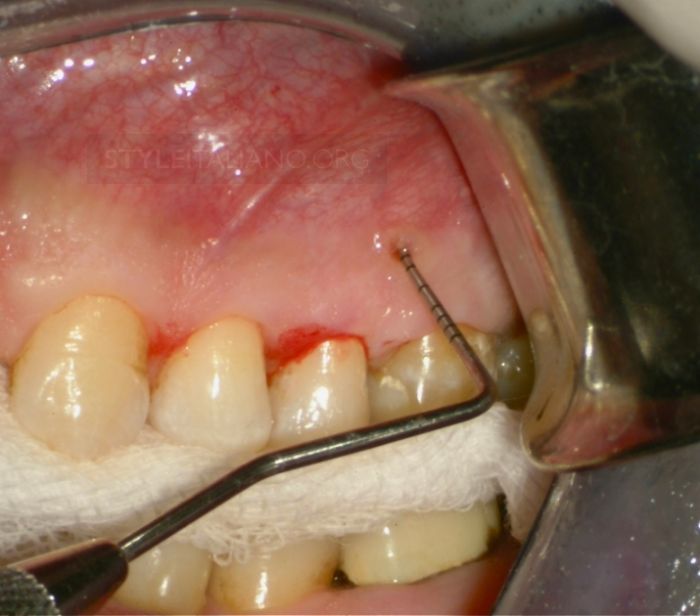
Fig. 5

Fig. 6
Img. 6 - INCISION AND FLAP ELEVATION
The incision must be performed in a continuous motion and full thickness. The horizontal incision follows the scalloped gengiva and connects the two vertical incisions. For this kind of surgery it is normal to use mini- or micro-blades. In this specific case we used a mini-blade, 6400 round tip (Surgistar, CA, USA). The round sharp tip is also useful during the phases of the flap elevation because it allows detachment of the flap from the periosteum in case of incomplete incision.

Fig. 7

Fig. 8

Fig. 9

Fig. 10
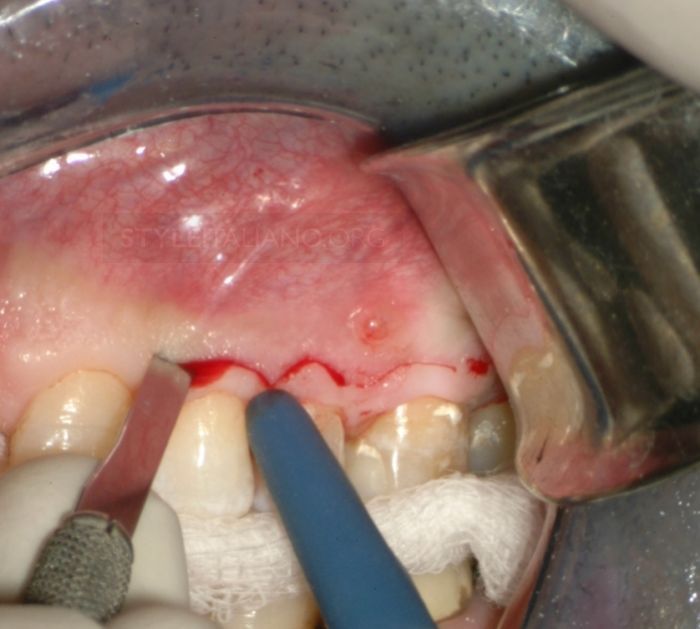
Fig. 11

Fig. 12

Fig. 13

Fig. 14

Fig. 15
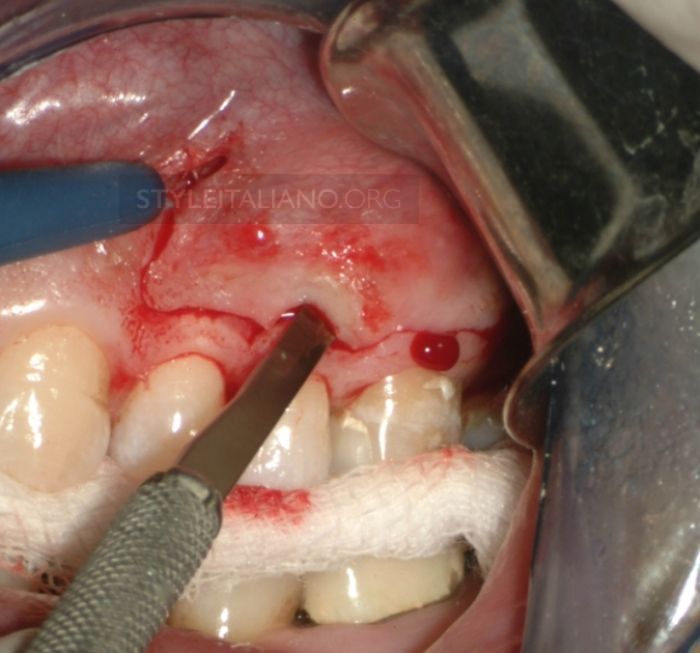
Fig. 16
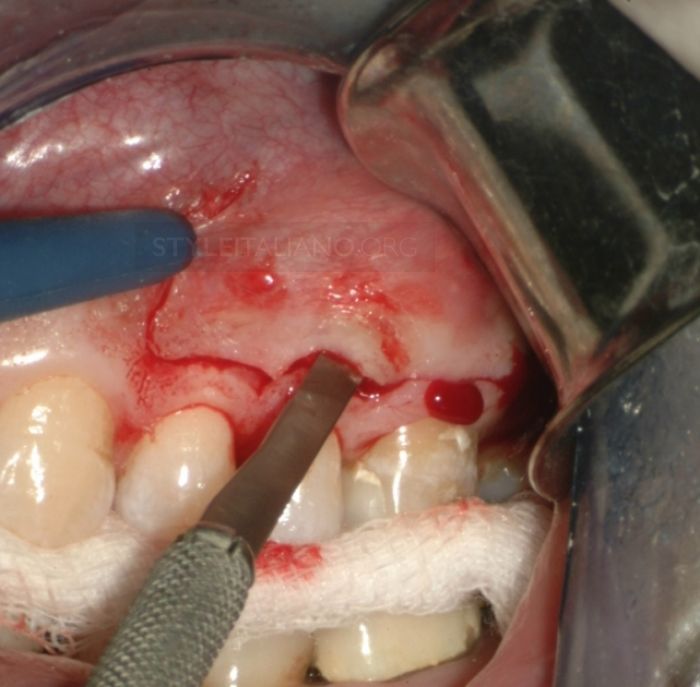
Fig. 17
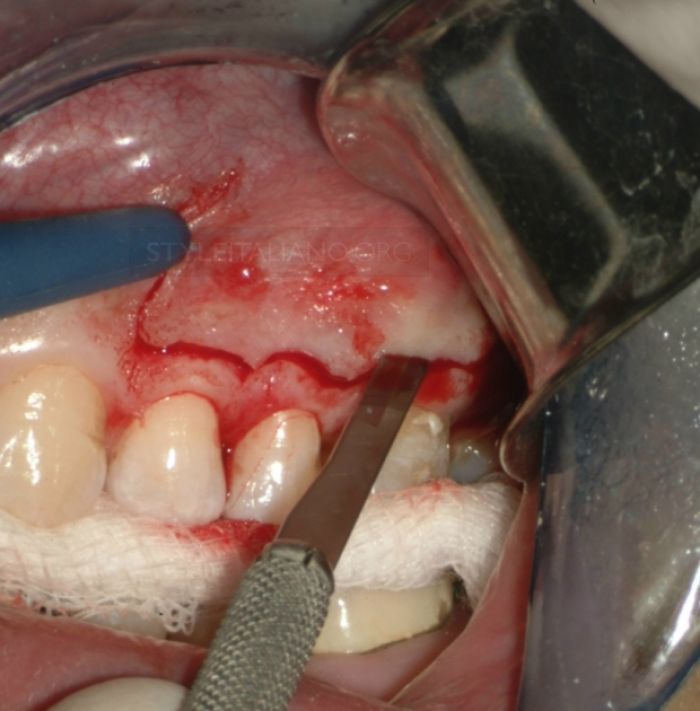
Fig. 18

Fig. 19
Flap elevation is completed with scalpels, in this case, the curettes designed by Clifford Ruddle are being used: these are available on the market in three different shapes (left, right and straight) and with two different head shapes (square or round).

Fig. 20
OSTEOTOMY AND APICAL RESECTION
This part of the treatment is the heart of the endo surgery and we will discuss the technique in further articles. In these pictures we can briefly see all the phases of the treatment. The osteotomy and the apical resection is completed in the same action, with a straight handpiece, after the resection the cavity is performed with ultrasonic tips that allow us to shape the canal along the root axis.

Fig. 21

Fig. 22
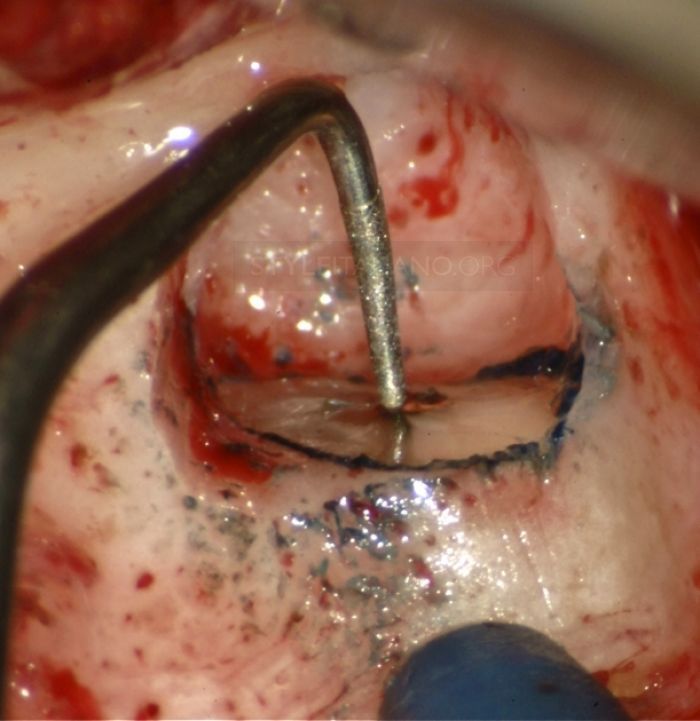
Fig. 23
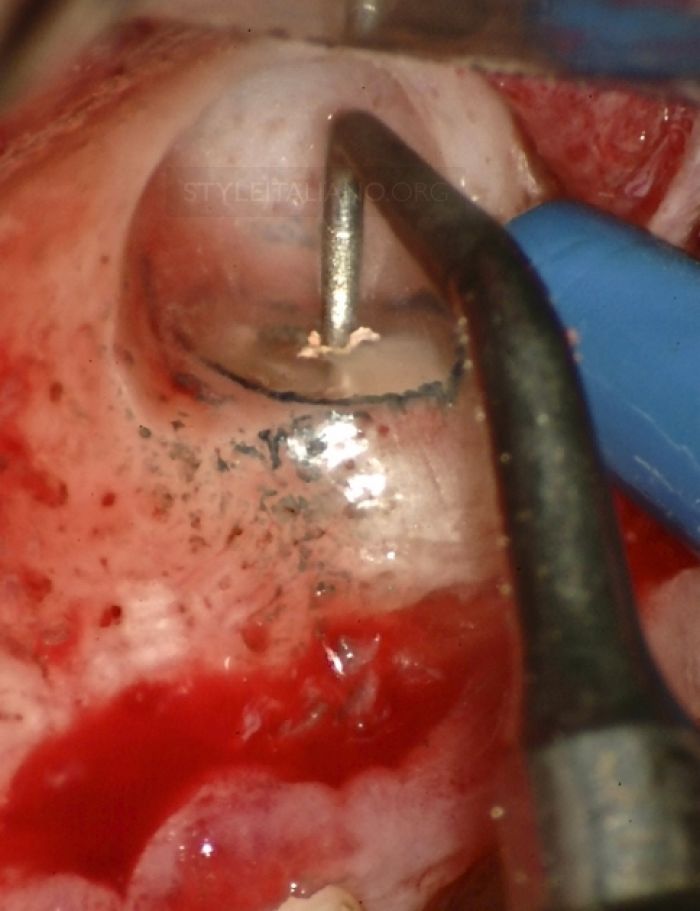
Fig. 24
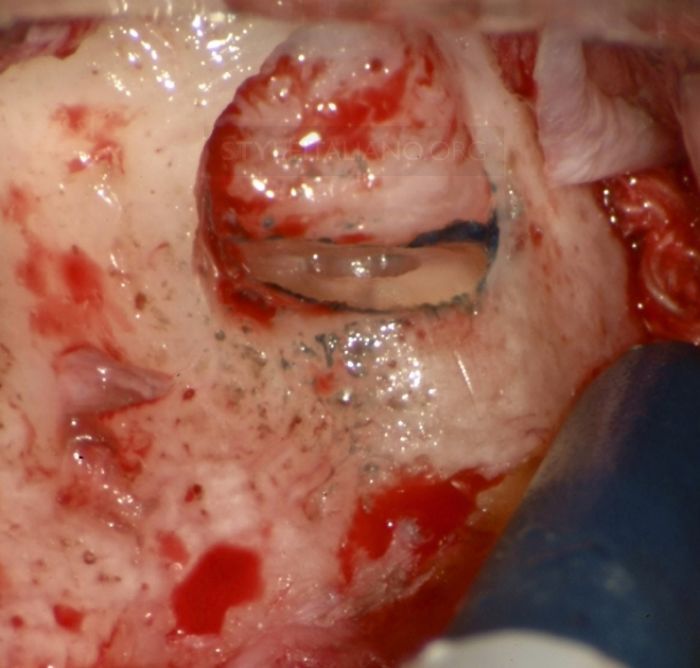
Fig. 25
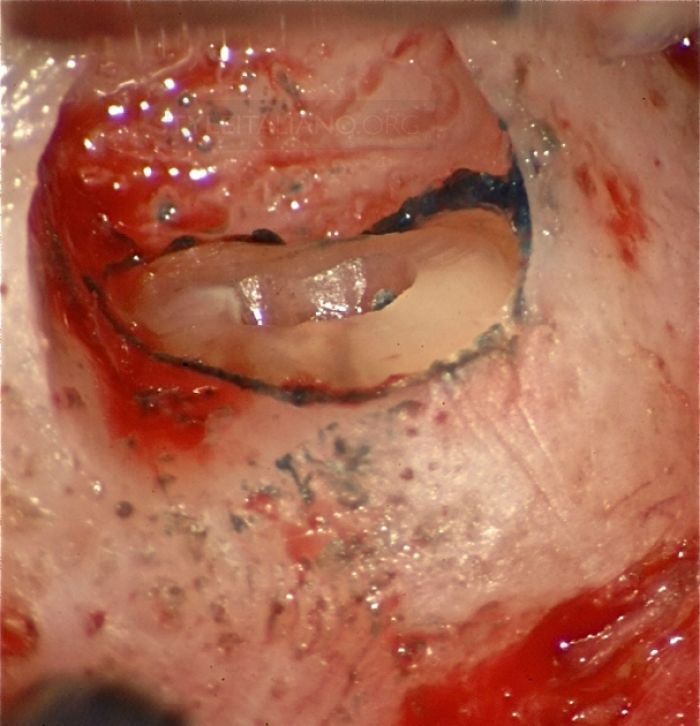
Fig. 26
The final cavity is correctly shaped with smooth walls, it is perfectly clean and ready to receive the root end filling.
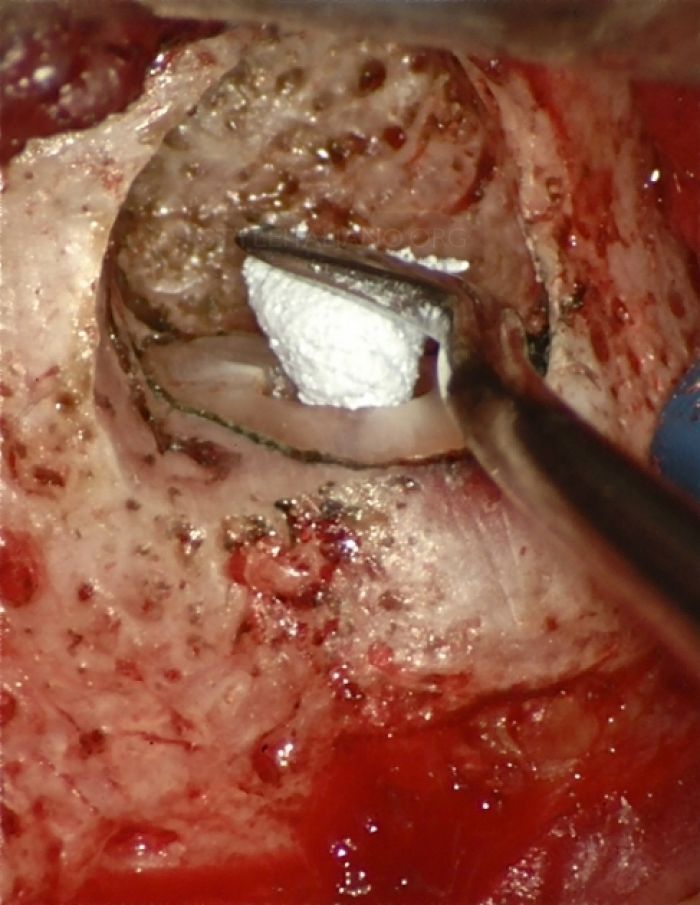
Fig. 27
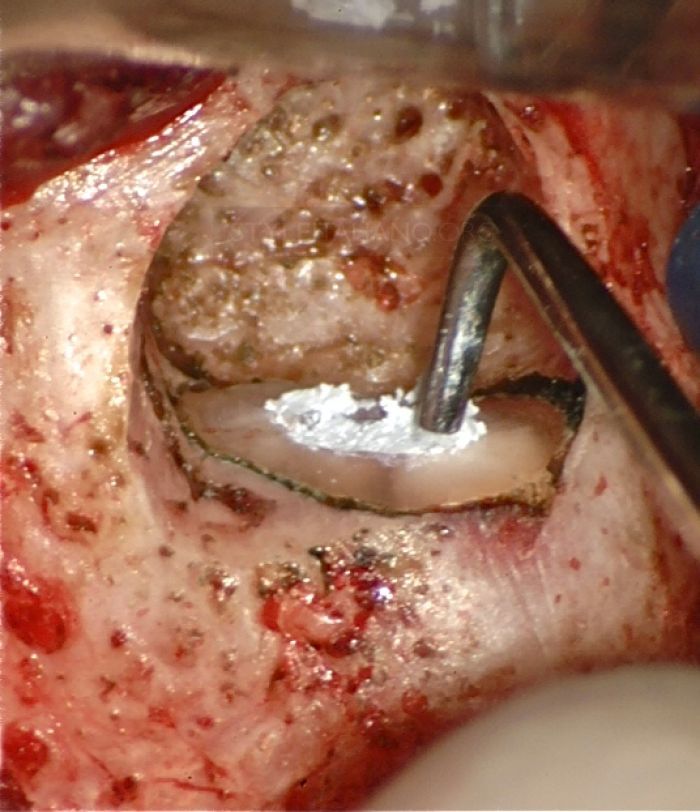
Fig. 28
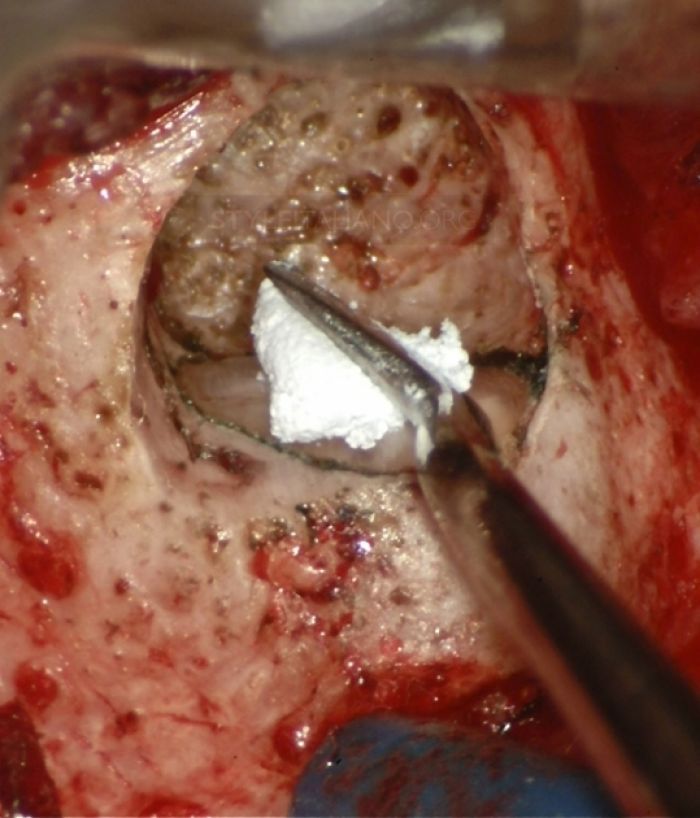
Fig. 29
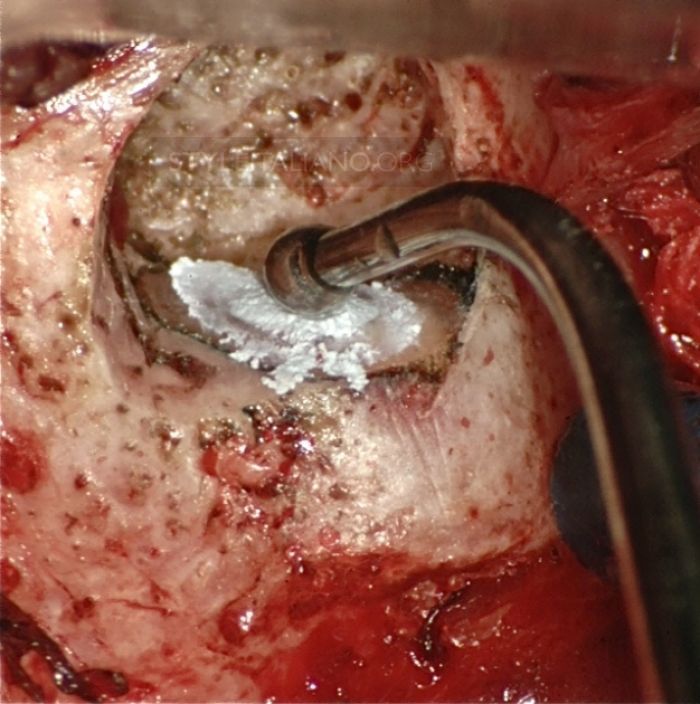
Fig. 30
Conclusions
This flap design provides good access, does not involve marginal gingiva and is indicated in presence of prosthetic crowns, being therefore indicated both for good surgical and endodontic workflow and biological preservation.
Bibliography
- Fermin A. Carranza, Michael G. Newman (1996) Clinical Periodontology, 8 thedn. W.B. Saunders: 592.
- Gutmann JL, Harrison JW (1999) Surgical Endodontics, 1st ed. Ishiyaku EuroAmerica, Inc. St.Louis. Tokyo, All India Publishers, 17, 7, 162-167.
- Donald E Arens, Practical lessons in Endodontic Surgery, 1st edn: Quintessence Publishing Co, Inc, 5156.
- Franklin S. Weine (1998) Textbook of endodontology, 5th edn: Mosby 553.
- Guerini V (1909) A history of dentistry, Philadelphia: Lea and Febiger, 117.
- David M. Nosonowitz, Pleasant valley, N.Y.(1983) Flap designs for gaining access to periapical lesions. Oral surgery November, 537541.
- Buckley JP (1914) Root amputation. Dent Summary 34 , 964965.
- Hofer O. (1935) Wurzelspitzenresektion und Zystenoperationen. Z. Stomatol 32, 513533.
- Gutmann J, Harrison J(1985) Posterior Endodontic Surgery: Anatomical consideration and clinical techniques. International Endodontic Journal 18, 8 34.
- Neumann R(1926) Atlas Der radikal chirurgischen Behandlung der Paradentosen. Berlin. Hermann Meusser, 14.
- P. Velvart (2002) Papilla base incision: a new approach to recession free healing of the interdental papilla after Endodontic surgery. International Endododntic Journal 35, 453460


