Single, rare and fabulous
06/12/2024
Andreas Louloudiadis
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
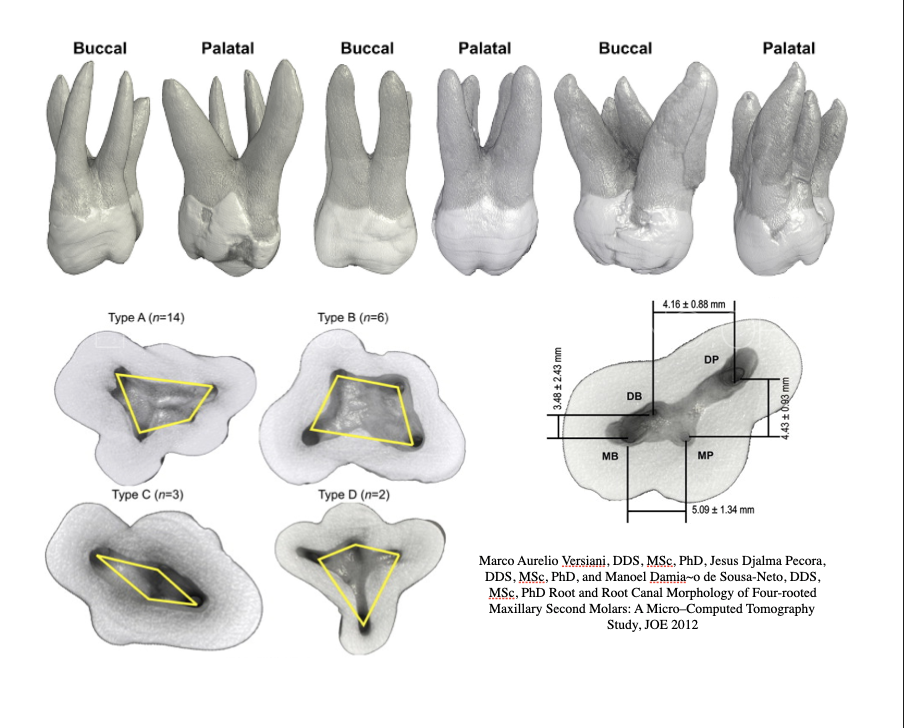
A thorough and detailed knowledge of root canal anatomy is a crucial requirement for a successful endodontic treatment outcome. Due to each tooth singularity a vast number of morphological variations is possible. Such variations increase the difficulty in shaping, cleaning and filling the three dimensional root canal system.( Vertucci et al 2009).The anatomical characteristics of permanent maxillary molars are complex and are generally described as teeth with three roots: Two buccal canals and one palatal (Bornstein et al). Probably, the tooth with the widest range of anatomical differences is the maxillary first molar ( Vertucci 1984, Cantatore et al 2006). A number of studies have been published on the anatomy and morphology of the maxillary first molar, depicting a great variety of anatomical configurations on this tooth. The majority of papers concern themselves mainly with the anatomy of the mesiobuccal root of maxillary first molar, and the incidence of the second mesiobuccal canal. Case reports of maxillary first molar with four and five roots (Fahid & Taintor, 1998) and four to six root canals (Maggiore et al 2000) or even seven separate root canals( Kottoor et al 2010) have been reported. Existence of C-shaped canals have been also reported (Khafrouf et al 2019). However, the configuration of one canal in one rooted maxillary first molar has rarely been described in studies either in-vitro or in-vivo (Gopikrishna et al, 2008). The prevalence of single canal in the maxilary first molar was reported to be 0,5%-0.6% ( Libfield Rotstein1989). The recently developed limited cone beam computed tomography designed for for dental use has a lower radiation dose and higher resolution than traditional computed tomography scans ( Patel 2009). It has proved useful in detecting periapical lesions ( Low at al 2008) and root canal morphology in maxillary region ( Tsiklakis et al 2005, Patel and Horner et al 2009). CBCT as a non invasive tool can provide three dimensional images of dentoalvelor regions for disease diagnosis and morphological evaluation in endodontics (Matherne et al 2008). Kim et al in their study using CBCT found the incidence of a single -rooted maxillary second molar to be 10,7% in the Korean population and Zhang et al found the incidence to be 10% in the Chinese population. Martins et al 2024 in multi-center cross-sectional study where researchers from 44 nations examined 26400 maxillary molars fusing cbct scans found that the prevalence of single-rooted with a single canal and four-rooted configurations in the maxillary first molar was 0.16% and 0.28%, respectively, while in the maxillary second molar, it was 2.56% and 0.83%. Despite CBCT imaging as analytical tool, the literature reports on the prevalence of single rooted maxillary molars still remains scarce. The present case report describes the endodontic treatment of a maxillary first molar having one such rarest variation that was diagnosed with the aid of Cone Beam Computed Tomography.
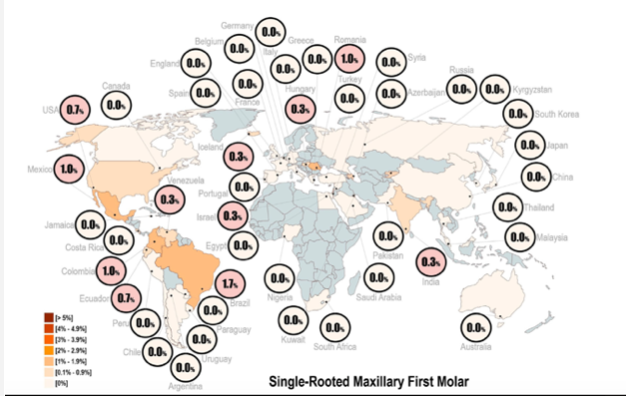
Fig. 1
Martins NR et al. Worldwide prevalence of single root canal and four-rooted configurations in Maxillary Molars:A Multi-center Cross-sectional Study with Meta-analysis. J Endod 2024 Sep;50(9):1254-72
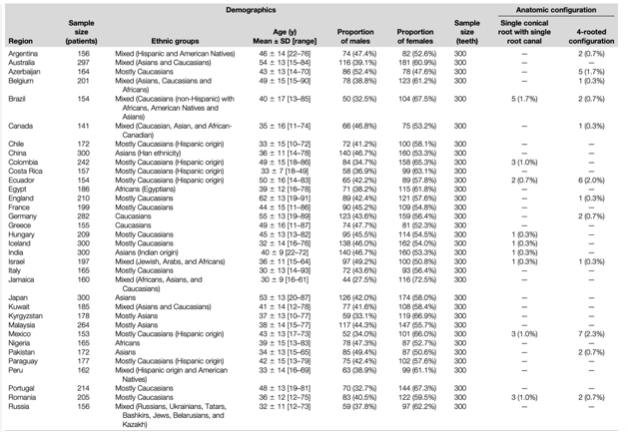
Fig. 2
Martins NR et al. Worldwide prevalence of single root canal and four-rooted configurations in Maxillary Molars:A Multi-center Cross-sectional Study with Meta-analysis. J Endod 2024 Sep;50(9):1254-72

Fig. 3
A 43 year old woman was referred for assessment and treatment of tooth 26. The patient reported an intermittent pain when biting on the tooth, and she did not give any history of spontaneous or nocturnal pain and there was no history of any swelling associated with the pain. Her medical history was non-contributory. A thorough dental history indicated that tooth 26 has had a deep occlusal-palatal composite filling. Clinical examination revealed moderate percussion pain on the left maxillary molar, and slight sensitivity to palpation. Periodontal examination was within normal limits and no mobility was noted. Radiographic examination revealed a deep composite restoration within close proximity to the pulp and a periapical pathology was present. The radiographic examination also revealed some variation in root canal anatomy of tooth 26 and tooth 27 having a single root and a single canal, and e decision for a cbct was made.
Based on clinical and radiographic findings a diagnosis of Pulp necrosis and Symptomatic Apical Periodontitis was formulated.

Fig. 4
Sagittal, cross-sectional and axial CBCT images of tooth #26
The results of the CBCT showed the presence of a single root with Vertucci’s Type I canal configuration and the same was observed for tooth 27.
Axial CBCT view of UL7
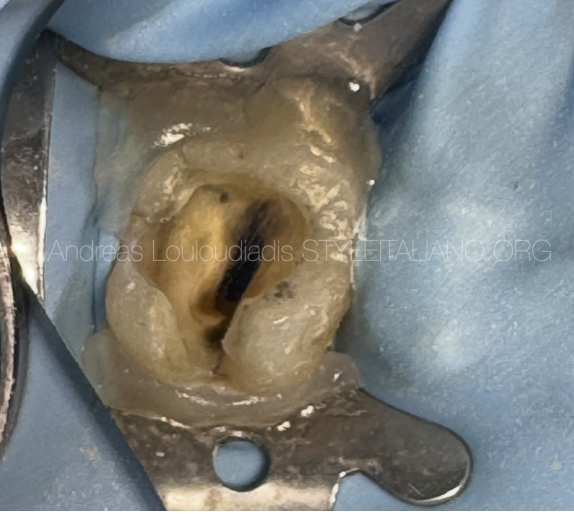
Fig. 5
Local infiltration anesthesia and single tooth rubber dam isolation using rubber dam seal (OpalDam Ultradent).
Removal of the defective existing composite restoration and identification of the pulp chamber showing only a single canal orifice was made.

Fig. 6
Access was made and identification of one large canal and preparation of the canal was achieved.
Working length was calculated using an electronic apex locator
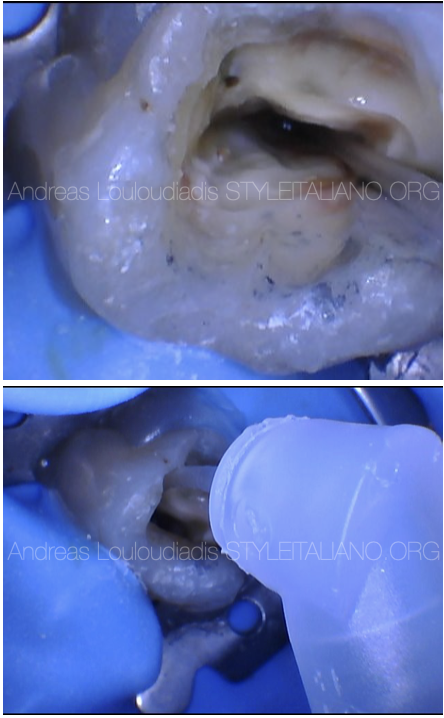
Fig. 7
Irrigation protocol included 5.25% NaOCl and 17% EDTA using Irriflex tip.
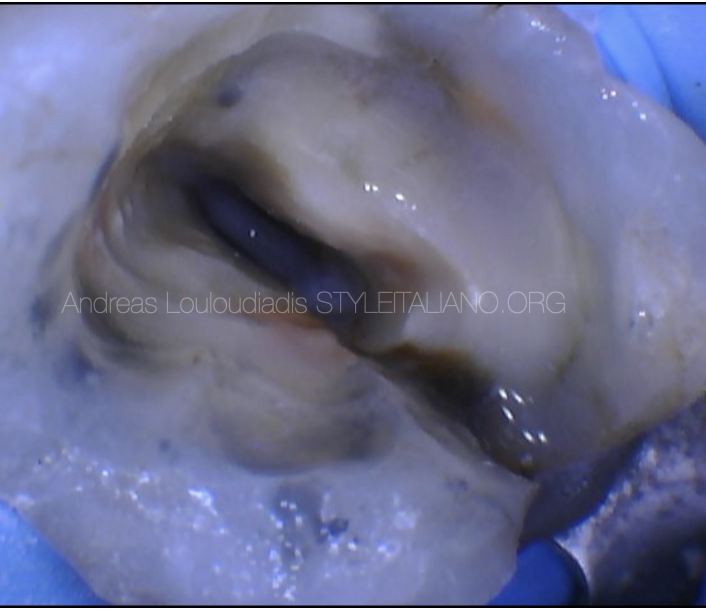
Fig. 8
Activation of the irrigant
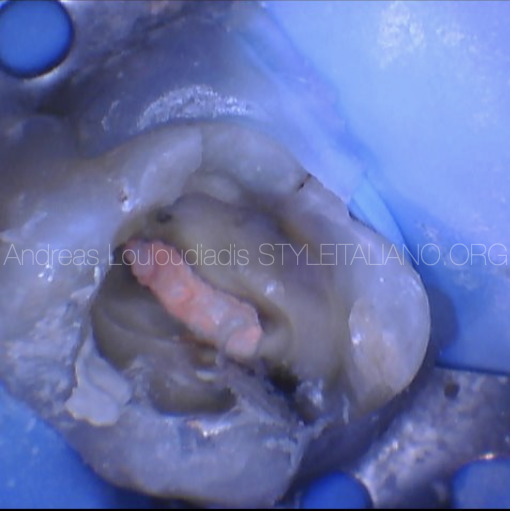
Fig. 9
Obturation was performed with WVC.
A composite resin restoration was placed and patient referred back for fabrication of an indirect restoration

Fig. 10
Final post operative xray showing one single canal with an apical delta anatomy and sealer puff.
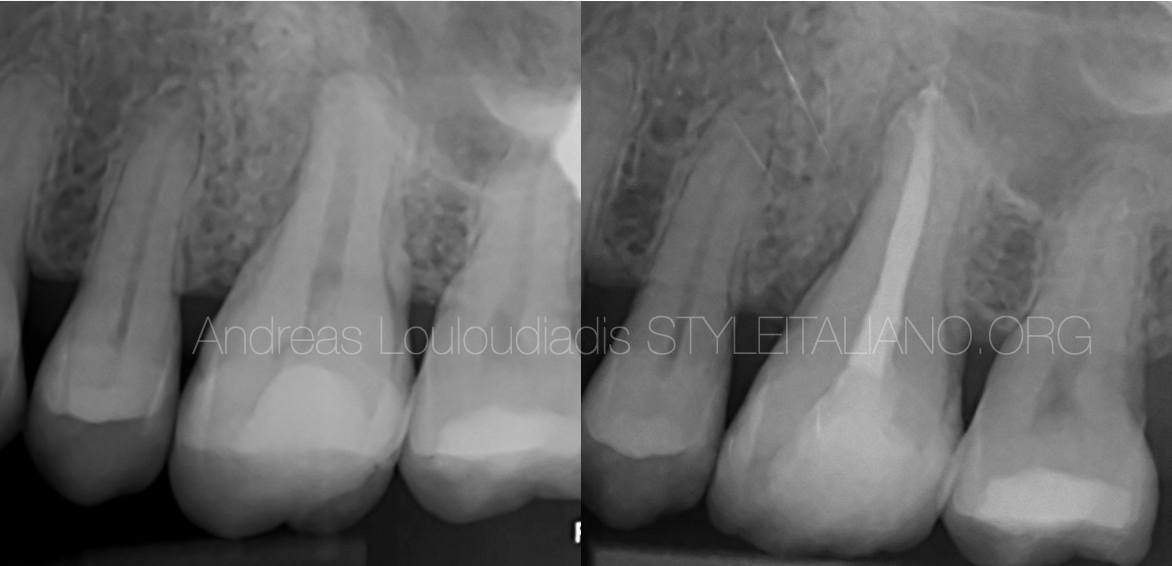
Fig. 11
Pre-op and Post-op radiograph of tooth #26
Conclusions
The present case report discusses the endodontic management of maxillary first molar with single root and single canal and also highlights the role of CBCT as an objective analytic tool to ascertain root canal morphology.
The AAE and ESE Position statement recommend intraoral radiograph as the imaging modality of choice. Furthermore they stated that CBCT should be considered as an adjunct in certain situations such as investigation of teeth with complex anatomy or inconclusive interpretation of two dimensional radiographs.
To achieve satisfactory root canal therapy, a proper and in-depth knowledge of complex and abnormal root canal morphology is more than essential. Although the incidence of single canal is not high, it is important to take these variations into consideration during root canal treatment of maxillary molar in order to ensure success.
A recent multi-centered cross-sectional Meta-analysis study concluded that the prevalence of single roots with a single root canal in maxillary molars was found to be low, with rates of 0.16% for the first molar, and 2.56% for the second molar, respectively.
Cone-beam computed tomography (CBCT) can be an effective tool for diagnosis and treating a single-rooted maxillary first molar with complex root canal configuration due to its accuracy, reliability and three dimensional imaging capabilities and guides and helps the clinician to achieve an efficient outcome.
Bibliography
1.Low K, Dula K,Burgin W, Thomas VA. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred or apical surgery. J Endod 2008 May;34(5): 557-62
2.Gopikrishna et al. Endodontic management of a maxillary first molar with single canal diagnosed with the aid of Spiral CT: A case report. J Endod 2006 Jul ;32 (7): 687-691
3.Patel S, Durrack C, Abella F, Brown J, Pimentel T, Kelly RD. Cone beam computed tomography in Endodontics- a review of literature. Int End J 2019 Aug;52(8):1138-1152
4.Martins NR et al. Worldwide prevalence of single root canal and four-rooted configurations in Maxillary Molars:A Multi-center Cross-sectional Study with Meta-analysis. J Endod 2024 Sep;50(9):1254-72
5.Zhang Q, Chen H, Fan B et al. Root and root canal morphology in maxillary second molar with fused root from native Chinese population. J Endod 2014;40:871-5
6.KottoorJ, Velmurugan N,Sudha R Hemmalathi S. Maxillary first molar with seven root canals diagnosed with cone-beam tomography scanning: a case report. J Endod 2010; 36:915-921
7.Tsiklakis K et al. Dose reduction in maxilofacial imaging using low dose Cone Beam CT. Our J Radiol 2005;56(3):413-417
8.AAE and AAOR joint position statement: use of cone-beam computed tomography in endodontics 2015 update. Oral Surgeon Oral Med Oral Pathol Oral Radiology 2015;120:508-12
9.Bornstein MM, Wasmer J, Sendi P, Janner SF, Buser D. Characteristics and dimensions of the Schneiderian membrane and apical bone in maxillary molars referred for apical surgery: a comparative radiographic analysis using limited cone beam computed tomography. J Ended 2012; 38:51-57
10.Kharouf N, Haikel Y, Mancino D.Unsual Maxillary first molars with C-shape Morphology on the same patient: Variation in root canal anatomy.Case Reports in Dentistry Oct 2019 (19)
11.Matherne R, Angelopoulos C, Kullid J, Tira D. Use of cone- beam computed tomography to identify root canal systems in vitro. J Endod 2008 jan;34(1) :87-9
12.Peikoff MD, Christie WH, Fogel HM. The maxillary second molar: variations in the number of roots and canals. Int Ended J 1996;29(6) :365-9
13.Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surgeon Oral Med Oral radiology Oral Pathology. 1984;58:589-599
14.Fahid A, Taintor JF. Maxilalry second molar with 3 buccal roots. J Endod 1998 ;14:181-183
15.Libfield H, Rotstein I. Incidence of Four-Rooted Maxillary Second Molars: Literature review and radiographic survey of 1200 teeth. J Endod 1989;15(3): 129-131
16. Kim et al. Morphology of Maxillary first and second molars analyzed by cone- beam computed tomography in Korean population. J Endod 2012;38:1063-8