Regenerative endodontics: A Reliable Option
08/07/2021
Ahmed Shawky
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Various regenerative endodontic treatment (RET) protocols have been suggested with differences mainly in the disinfection technique used, intracanal medicaments, scaffold systems, and coronal filling materials. In order to reduce such variability, the American Association of Endodontists (2013) and European Society of Endodontology (2016) developed evidence based recommended protocols. These guidelines helped reduce some of the differences in the RET steps such as EDTA and sodium hypochlorite use, however, variations in terms of intracanal medicament, sealing material and assessment tools still exist due to the lack of high-quality evidence.
Our objectives in such treatments are primarily resolution of apical periodontitis and reconstitution of the lost structures, and secondarily will be continuation of root development (in terms of apical closure, root lengthening and dentin thickening)
The aim of this case report is to demonstrate successful regenerative therapy monitored for 42 months.
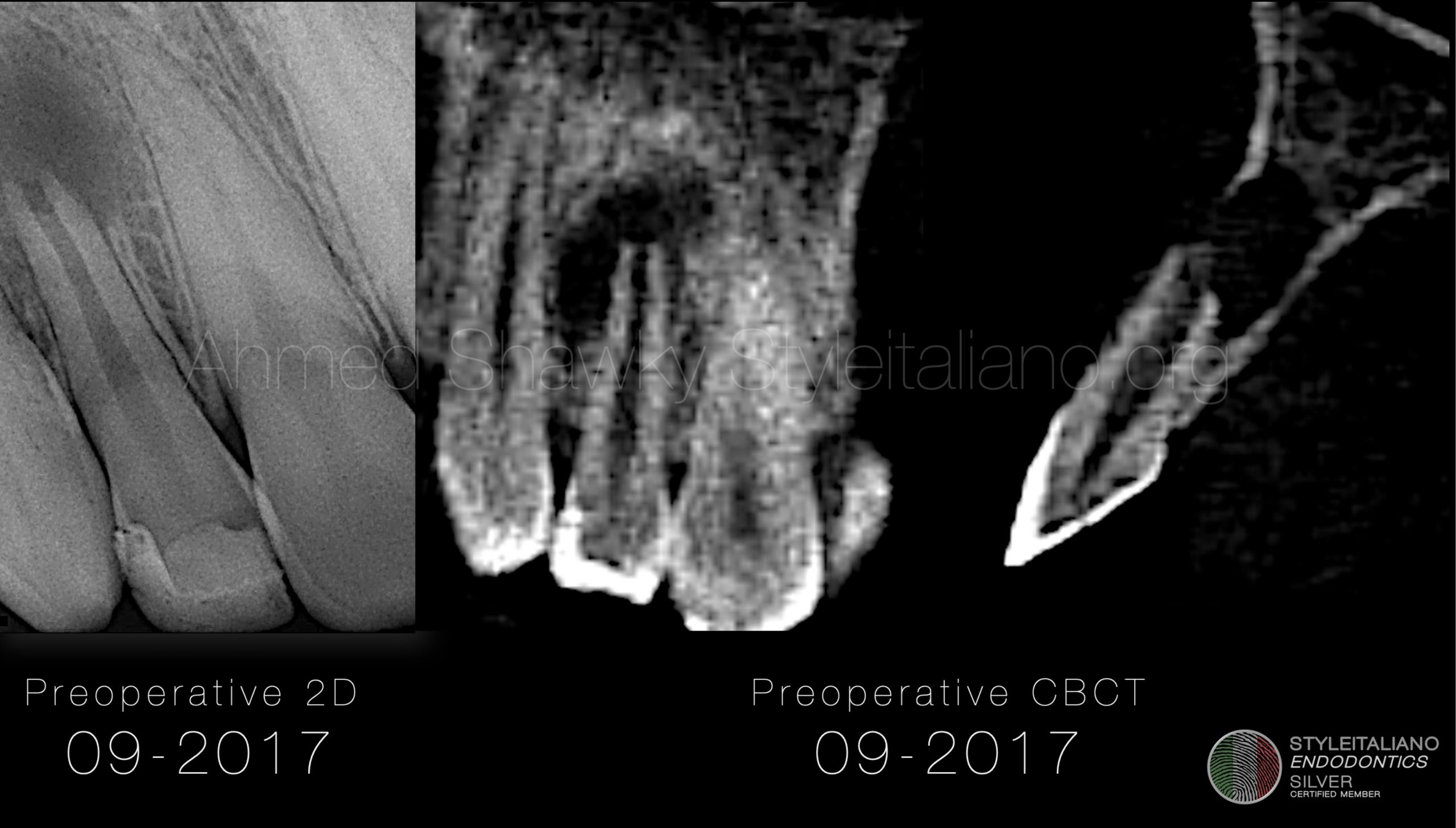
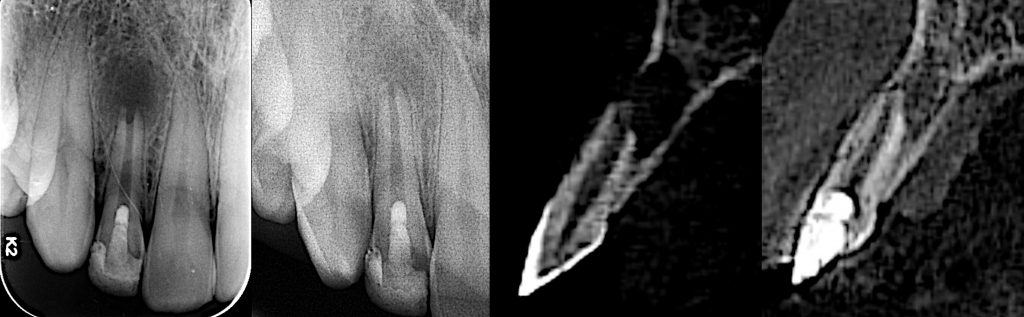
Fig. 1
A young male patient presented to the clinic in 2017 complaining of coronal discoloration in a previously restored maxillary lateral incisor, with intermittent appearance of a small gum swelling but without recognizable painful symptoms. Radiographic evaluation revealed an immature root with chronic apical periodontitis. CBCT evaluation confirmed the 2D radiographic evaluations and provided additional info about the cortical plate which was perforated labially due to infection
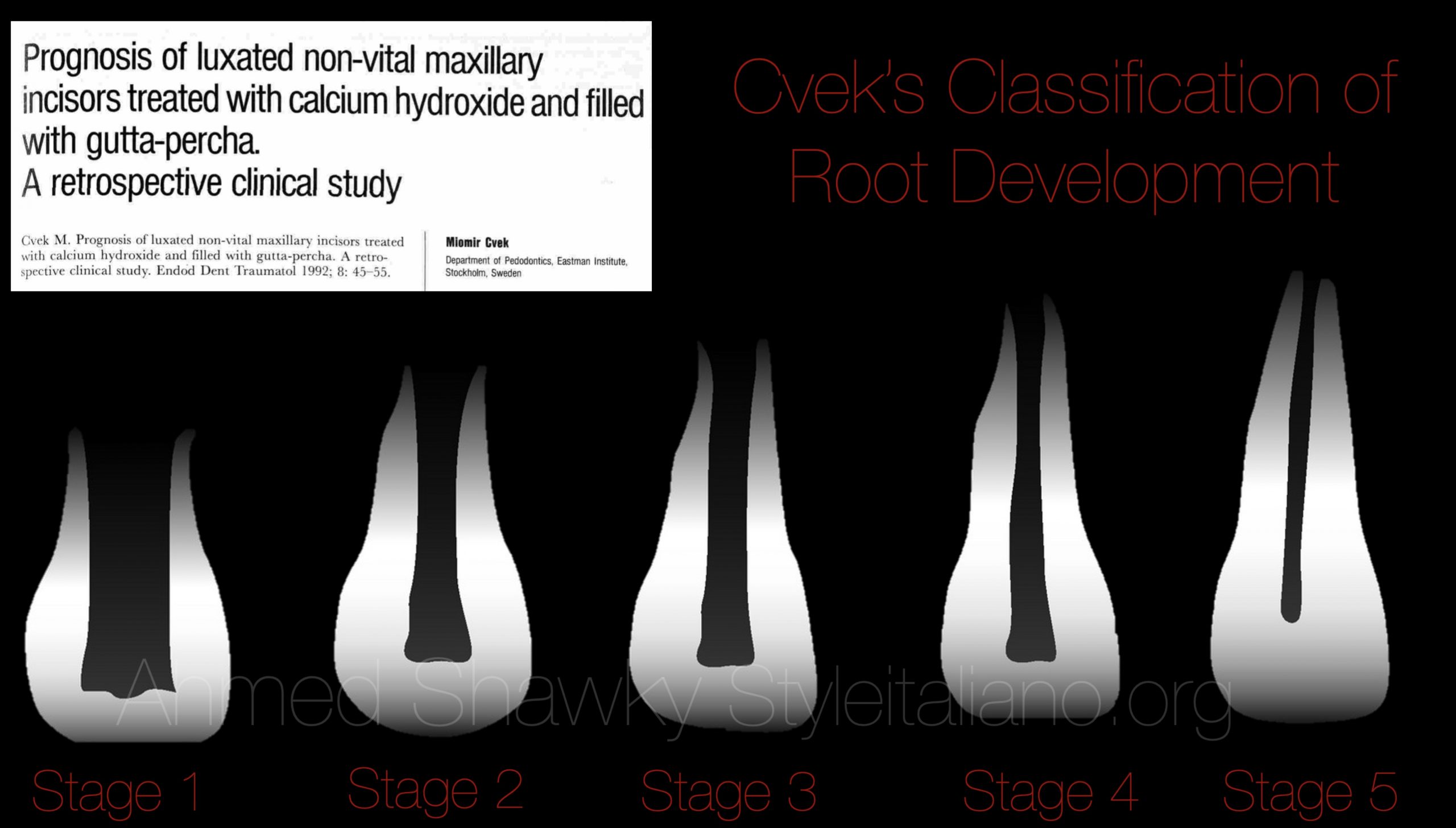
Fig. 2
The stage of root maturity was decided as Cvek’s stage 3

Fig. 3
Clinical examination revealed a previous old composite restoration that is discolored. The tooth was mildly tender to percussion. The mucosa was showing a small gum boil opposite to the root apex of the lateral incisor in question. A final diagnosis of pulp necrosis with chronic apical periodontitis was given at the end and regenerative endodontic treatment was advised.
The First visit:
The patient was consented about the regenerative treatment limitations, including; potential coronal discoloration and lack of remarkable continuation of root development. Also, the patient was informed that in case of failure of the procedure, the treatment will be shifted to either apical plug or apical microsurgery, depending on the case givens, if necessary.
RET protocol was carried out in this case on two visits. The first visit was dedicated to disinfection of the root canal system. After rubber dam application and access preparation, the canal was minimally instrumented using hand files and heavily irrigated using 20 ml 5.25% NaOCl over 5 minutes using a side vented needle adjusted 3 mm from the full working length. The canal was then flushed with 20 ml of sterile saline followed by a final rinse of 10 ml 17% EDTA solution over 5 min. The canal was then saline flushed and dried with sterile paper points. The dried canal was then medicated with a triple antibiotic paste (TAP) composed of equal portions of Metronidazole, Ciprofloxacin and Minocycline.
The tooth was sealed with a glass ionomer temporary filling for 3 weeks.

Fig. 4
The second visit
The patient returned back after 3 weeks with complete resolution of the signs and symptoms he previously had. That was the sign to move forward in the regenerative procedures (figure 4). In the second visit the tooth was anesthetized using a plain local anesthetic, in order to facilitate creating blood clot scaffold, rubber dam applied and the tooth re-opened.
The TAP was removed using a combination of copious irrigation and mechanical activation of the irrigant until no traces of the antibiotic paste remaining under magnification.
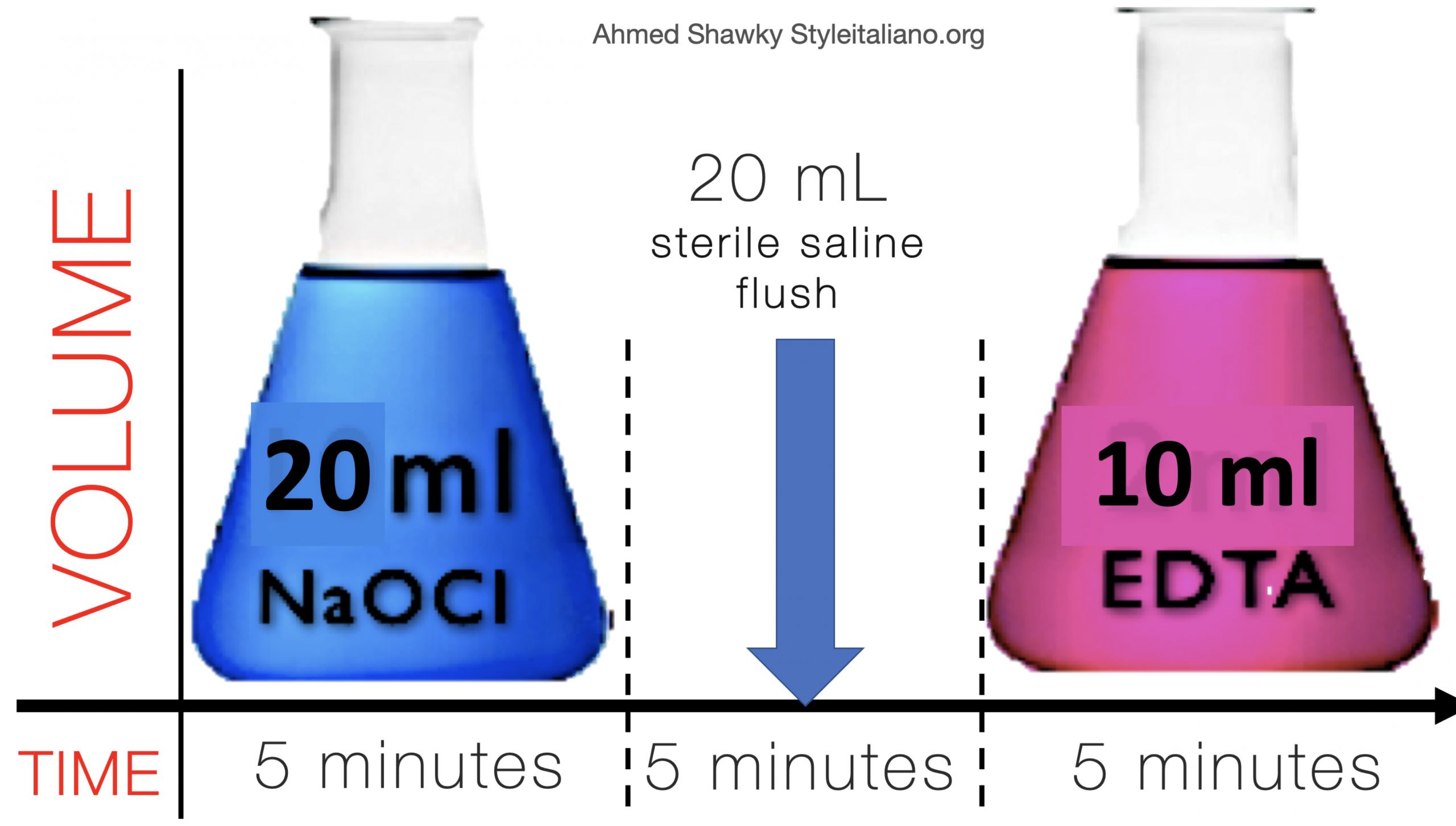
Fig. 5
Final rinse protocol in regenerative therapy:
The canal is irrigated using 20 ml 2.5% NaOCl over 5 minutes using a side vented needle adjusted 3 mm from the full working length. The canal is then flushed with 5ml of sterile saline followed by a final rinse of 10 ml 17% EDTA solution over 5 min.
EDTA is very important in RET protocols as it stimulates the release of various growth factors from dentin. These growth factors will help the attachment of the stem cells (SCAPs, stem cells from apical papilla) to the root canal walls and will promote their differentiation into hard tissue forming cells odontoblast-like cells)
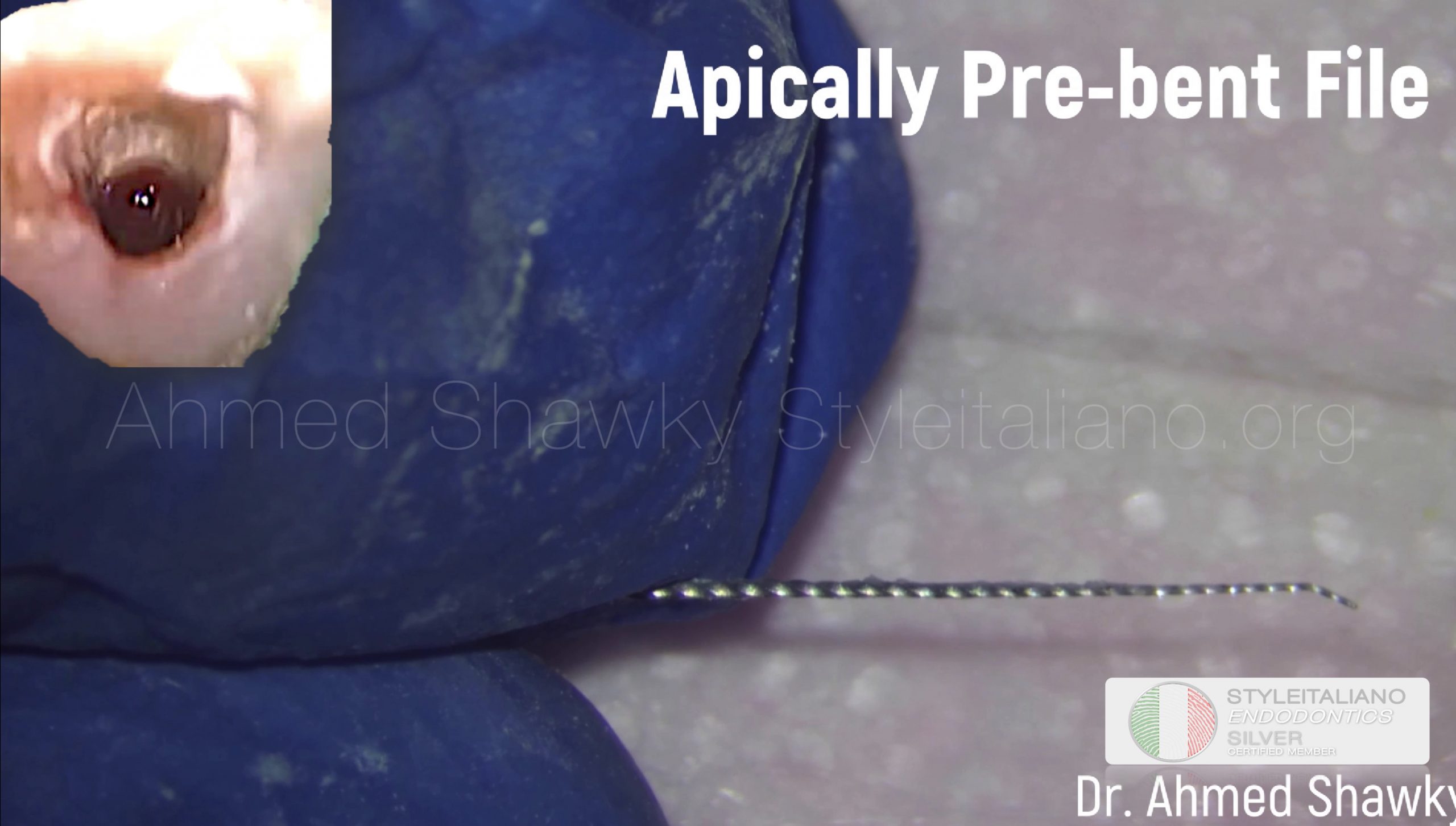
Fig. 6
Provision of the scaffold:
A pre-curved size #20 K-file was introduced to a length 2 mm beyond the apical foramen in order to initiate bleeding, which was confirmed under magnification. A lightly moistened, sterile cotton pellet was then placed into the canal, 3-4 mm apical to the CEJ, for 7-10 minutes to allow blood clot formation.

Fig. 7
Triple coronal seal
A layer of white MTA was then placed over the collagen barrier followed by a moist cotton pellet and The tooth was restored using a layer of reinforced glass ionomer followed by resin composite to establish a triple sealed hermetic structure. The patient was scheduled for recalls at 3, 6, 9 and 12 months to monitor the outcomes of the regenerative therapy.

Fig. 8
Image standardization in recalls:
The radiographic images along the follow up timeline were standardised using a custom-made index comprising of a Rinn film holder, a paralleling device and addition silicon impression material
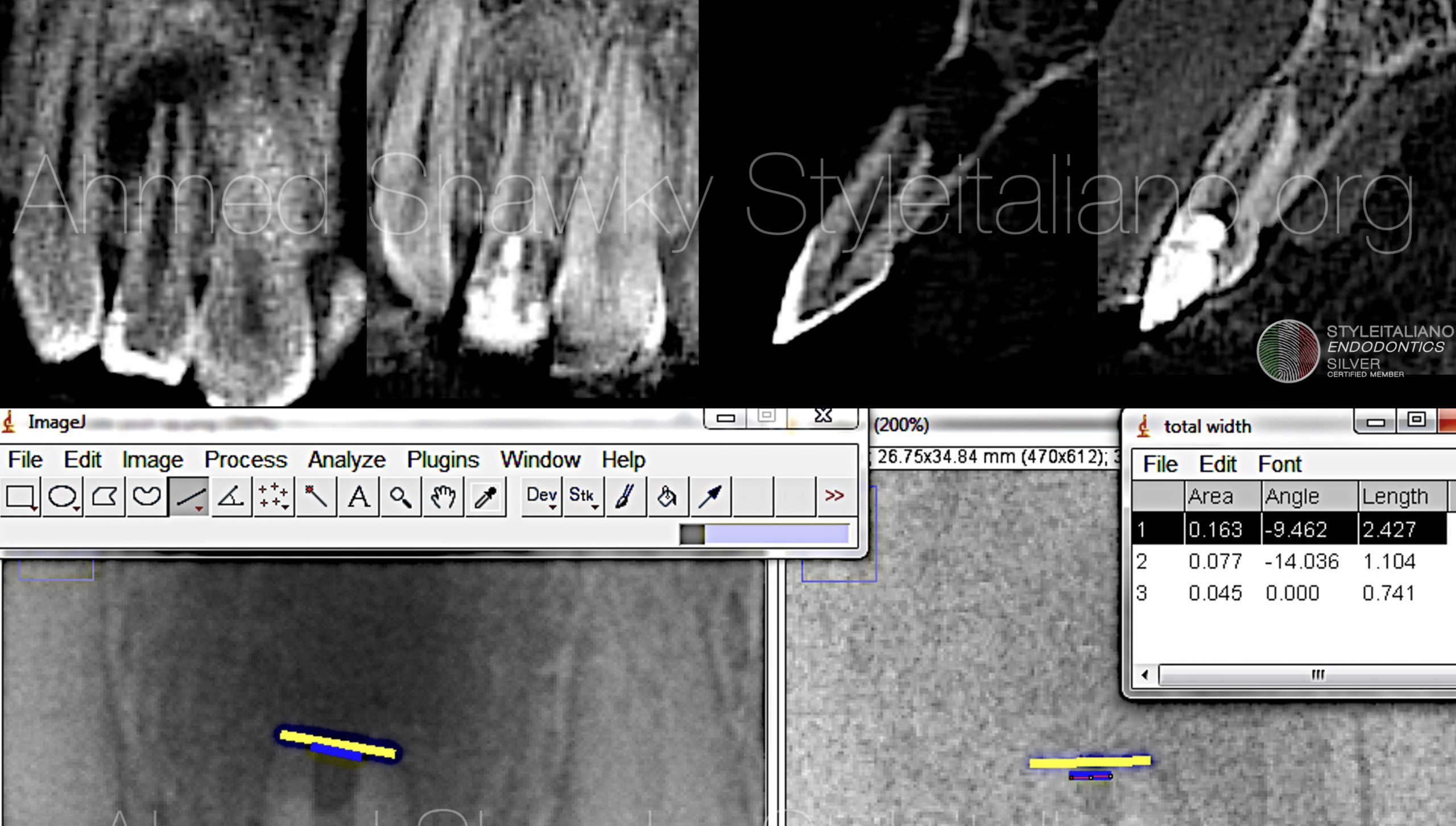
Fig. 9
One year recall:
At the 12months recall, CBCT evaluation showed complete healing of periapical bone and restoration of labial cortical plate integrity fulfilling the primary objective of the procedure.
Standardized Radiographic images were manipulated using the ImageJ software with turboreg plugin to perform alignment and mathematical correction of recall images. At 1 year, measurements of the apical foramen decreased from 1.10 mm to 0.74mm demonstrating a progress in apical closure, partly fulfilling the secondary objective of the procedure.

Fig. 10
18 months recall:
Standardized digital images revealed progressive apical closure with marked delineation of lamina dura around the whole root perimeter

Fig. 11
Before completing his 42 months, the patient sought full coverage to mask the discoloration that was caused partly due to minocycline containing TAP and partly due to interaction between the calcium silicate and blood clot

Fig. 12
Tooth preparation for full coverage

Fig. 13
A radiograph was taken to document full coverage of the tooth after 3 and a half years following regenerative therapy
Conclusions
Regenerative/revitalization endodontics is a very important treatment option for non-vital teeth with apical periodontitis especially those which lost vitality at an early stage of root development
Bibliography
- ElSheshtawy, A.; Nazzal, H.; El Shahawy, O.; El Baz, A.; Ismail, S.; Kang, J.; Ezzat, K. The effect of platelet-rich plasma as a scaffold in regeneration/revitalization endodontics of immature permanent teeth assessed using 2-dimensional radiographs and cone beam computed tomography: A randomized controlled trial. Int. Endod. J. 2020, 53, 905–921.
- Bose R, Nummikoski P, Hargreaves K (2009) A retrospective evaluation of radiographic outcomes in immature teeth with necrotic root canal systems treated with regenerative endodontic procedures. Journal of Endodontics 35, 1343–9.
- Tong HJ, Rajan S, Bhujel N, Kang J, Duggal M, Nazzal H (2017) Regenerative endodontic therapy in the manage- ment of nonvital immature permanent teeth: a systematic review- outcome evaluation and meta-analysis. Journal of Endodontics 43, 1453–64.
- Flake NM, Gibbs JL, Diogenes A, Hargreaves KM, Khan AA (2014) A standardized novel method to measure radio- graphic root changes after endodontic therapy in imma- ture teeth. Journal of Endodontics 40, 46–50.





