Post Endo Resto - Minimal Invasive Approach
09/12/2024
Massimo Giovarruscio
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Morphology Driven Preparation Technique
Morphology-Driven Preparation Technique (MDPT) is an advanced dental technique focused on preserving the natural morphology of teeth during restorative procedures.

Fig. 1
This approach is particularly important in adhesive dentistry and prosthodontics, where maintaining as much healthy tooth structure as possible is critical to long-term success. Adhesive preparations require removal of tooth structure about 50% lower than complete crown preparation
The technique has been described by the Italian Dentist Marco Veneziani in 2017

Fig. 2
New cavity preparation principles are based on morphological considerations in terms of geometry, and structure (dentin concavity and enamel convexity)
Form a 3D structural analysis of human teeth, it can be observed that the contours of the convex surface of enamel match concave profiles and sharp body dentin (sigmoid curve). The concavity of the dentin surface is particularly evident located in the middle third coronal to to the equator. Consequently the gold standard for cavity design constitutes a margin design with a beveled concave inclined plane that cuts the enamel convexity, following the dentin concavity without exposing it.
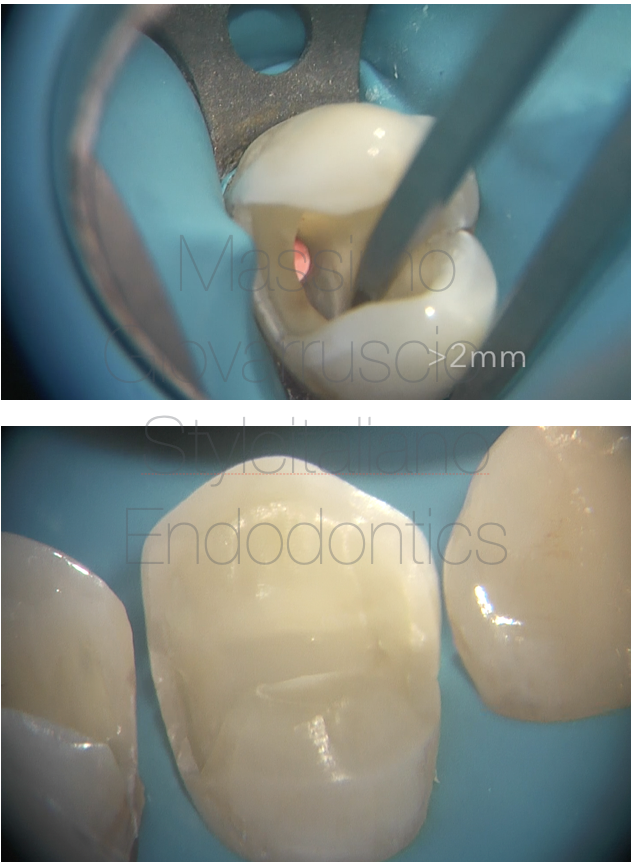
Fig. 3
Principles of Morphology Driven Preparation
- Preservation of Natural Tooth Structure:
- Focuses on removing only damaged or decayed tissue while retaining healthy enamel and dentin.
- Avoids unnecessary shaping that could weaken the tooth.
- Respect for Natural Contours:
-
- Maintains the natural anatomy and morphology of the tooth, such as cusps, ridges, and grooves.
- Ensures restorations integrate seamlessly with existing structures for both aesthetics and function.
- Minimally Invasive Approach:
-
- Guided by the principles of minimally invasive dentistry.
- Often utilizes magnification tools like loupes or microscopes to enhance precision.
- Guided by Biomimetics:
-
- Aims to replicate the biomechanical properties of natural teeth in restorations.
- Materials and techniques are selected to mimic natural tooth structure.
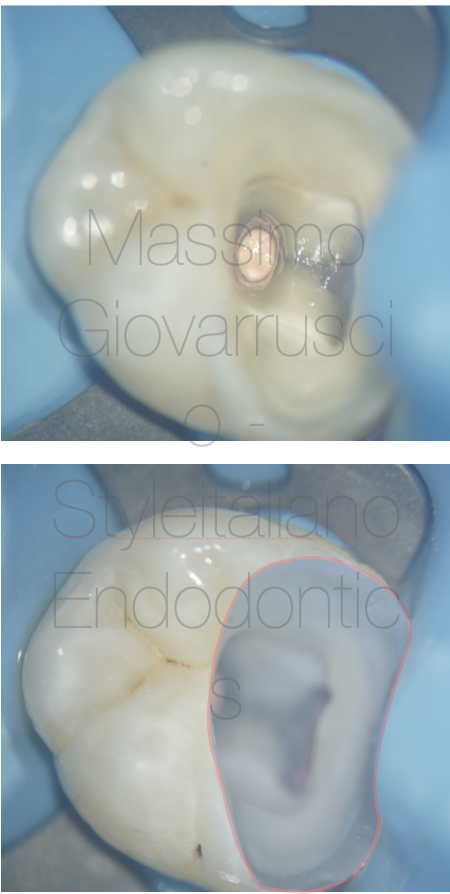
Fig. 4
Applications of MDPT in dentistry
Direct Restorations
-
- Composite fillings shaped to blend with natural morphology.
- Avoids over-reduction of enamel or dentin.
Indirect Restorations
-
- Preparation for inlays, onlays, veneers, or crowns with minimal tooth reduction.
- Ensures restorations adhere closely to existing tooth contours.
Endodontically Treated Teeth
-
- Shapes access cavities and post spaces to follow the tooth’s natural internal anatomy.
Guided Preparation Techniques
-
- CAD/CAM technologies or guided templates help execute precise preparations while preserving morphology.
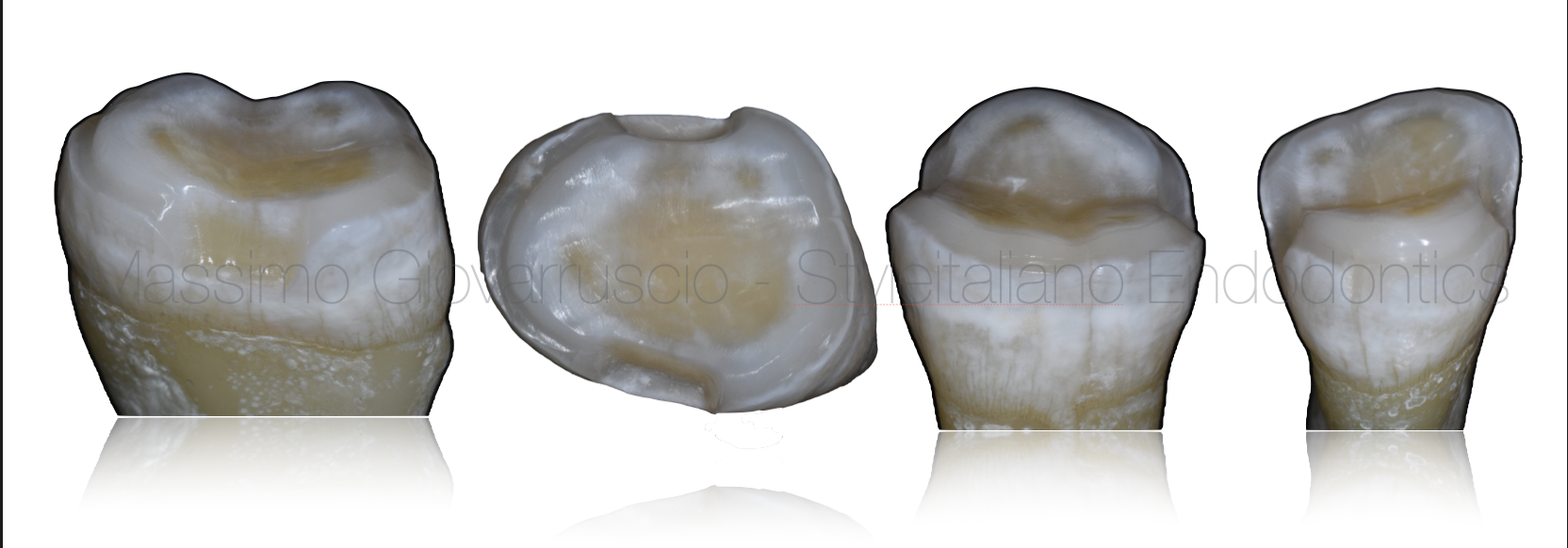
Fig. 5
The new cavity shape consists of continuous inclined plane cavity margins (concave bevel) on axial walls, whenever they are coronal to the equatorial tooth line.
A 1.2 mm thick BUTT-JOINT preparation is performed in the interproximal box and on the axial walls when the margins are apical to the equatorial line. The occlusal surface is anatomically prepared, free of slots and angles.

Fig. 6
1
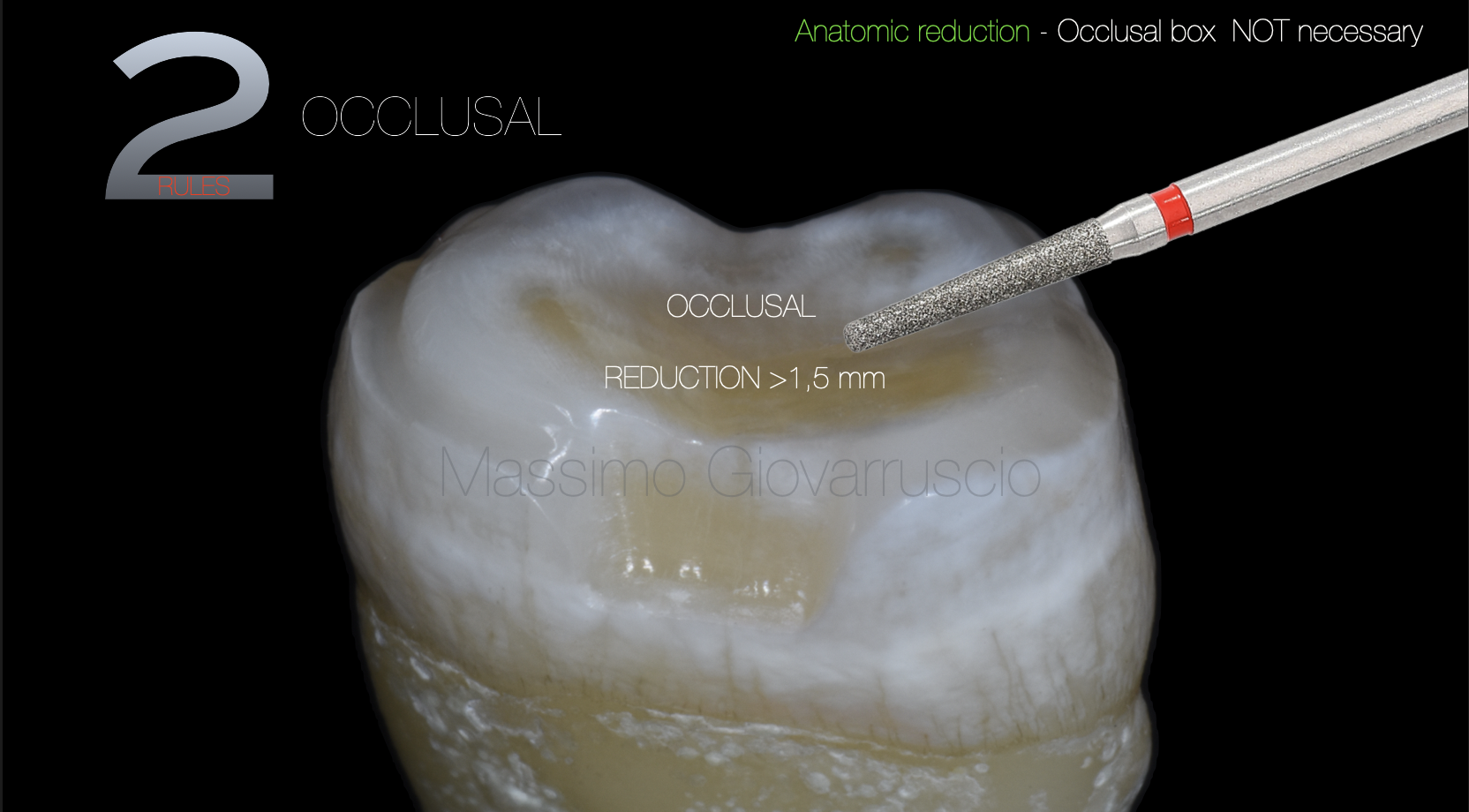
Fig. 7
2
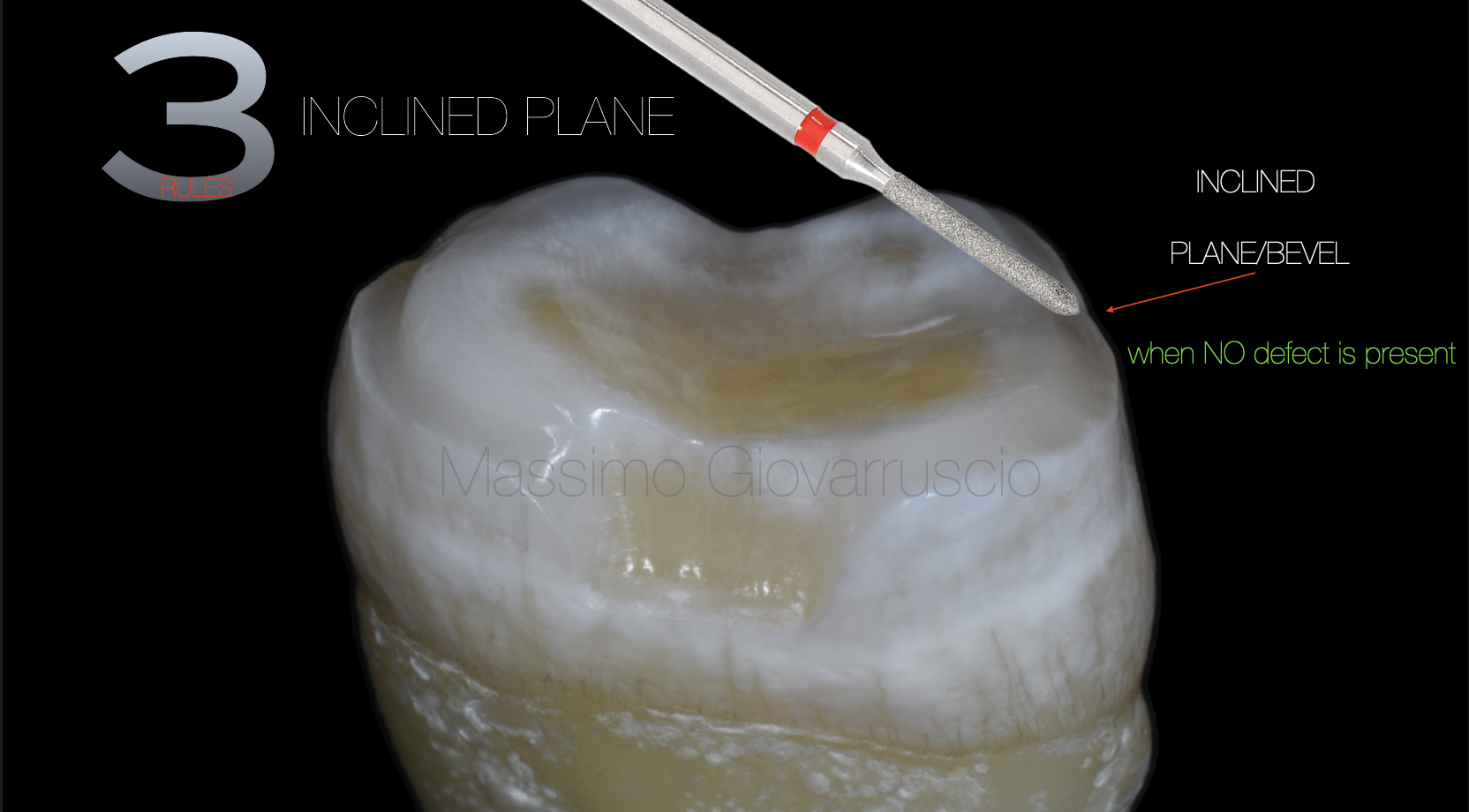
Fig. 8
3

Fig. 9
4
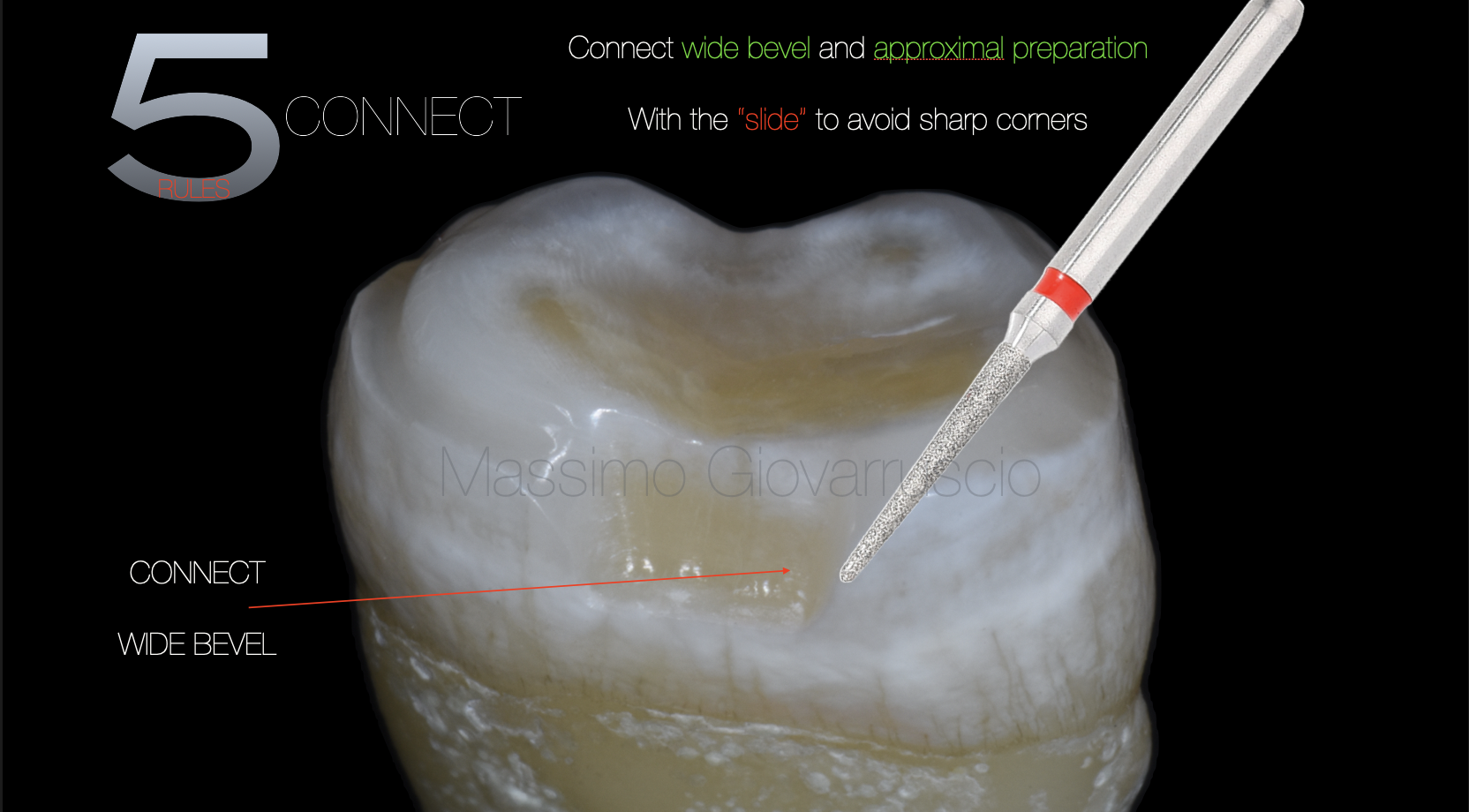
Fig. 10
5
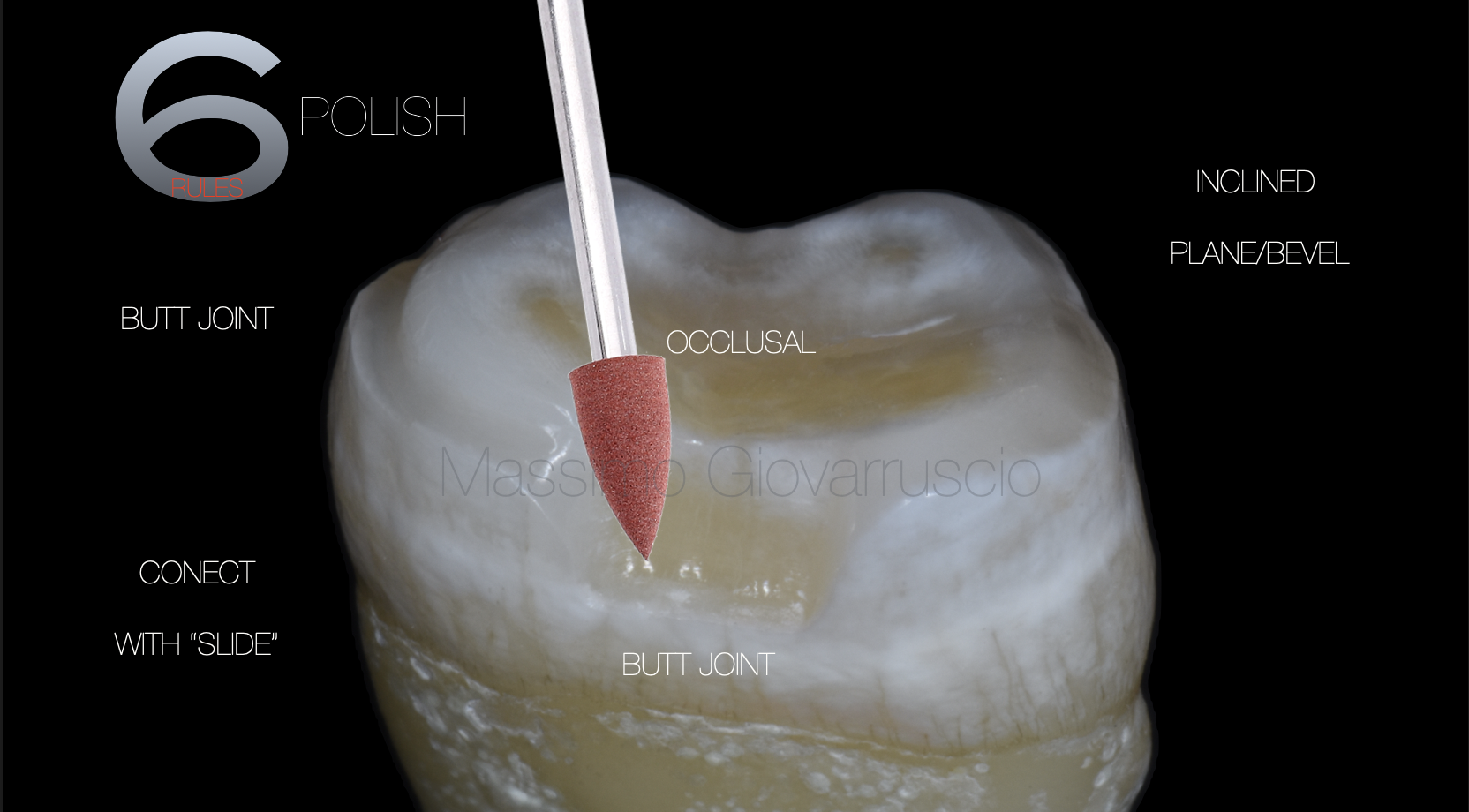
Fig. 11
6
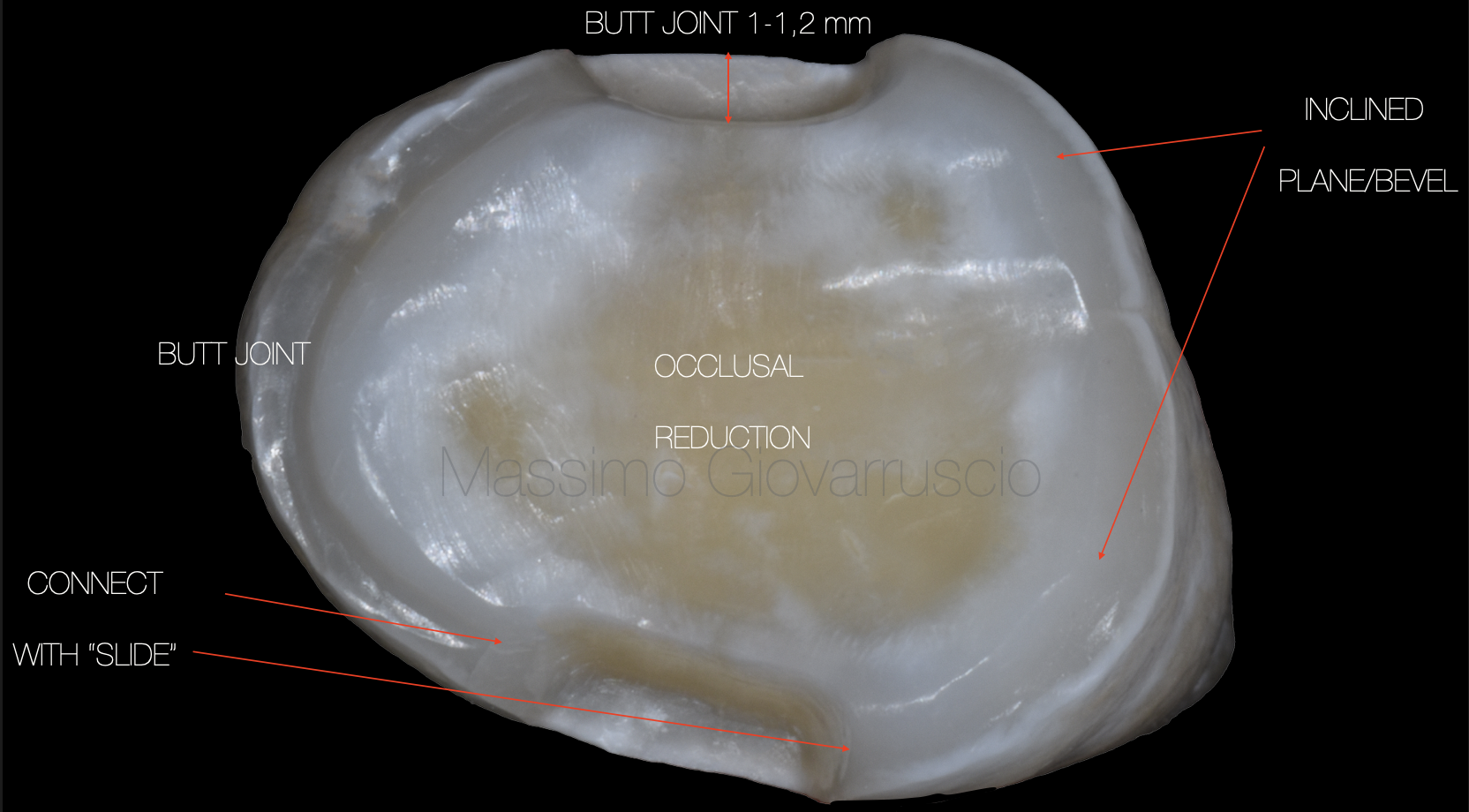
Fig. 12
Final shape of the preparation
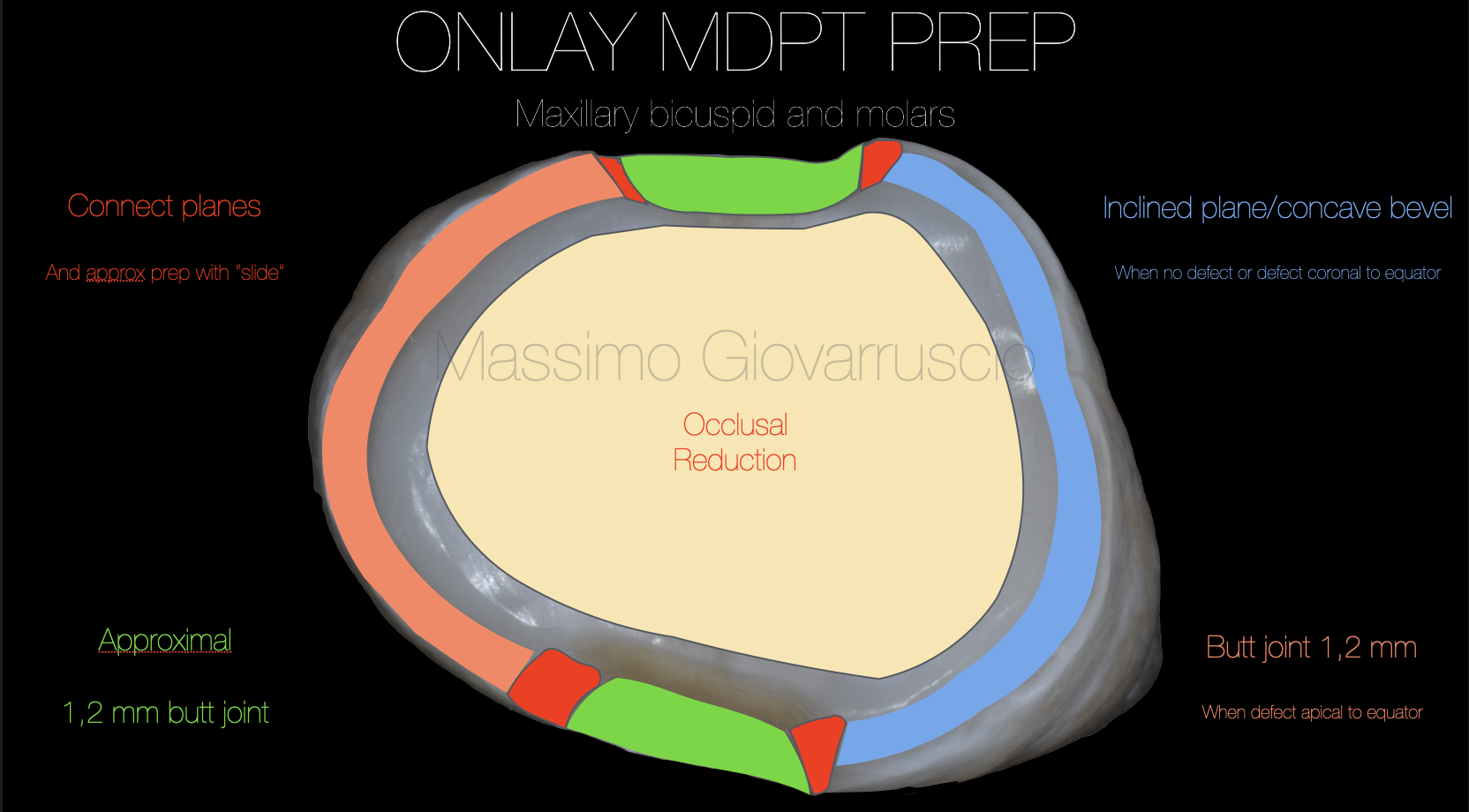
Fig. 13
ONLAY MDPT PREP
Maxillary bicuspid and molars

Fig. 14
The clinical advantages of anatomical preparation
- Improving adhesion quality (optimizing the cutting of enamel prisms, and increasing the available enamel surface)
- Minimizing dentin exposure
- Maximizing hard tissue preservation (the cavity being designed for cementation with reinforced composite resins, improvement of flow, and removal of excess material)
4) Optimization of esthetic integration due to the inclined plane design, which permits a better blending at the transition area between tooth and
restoration
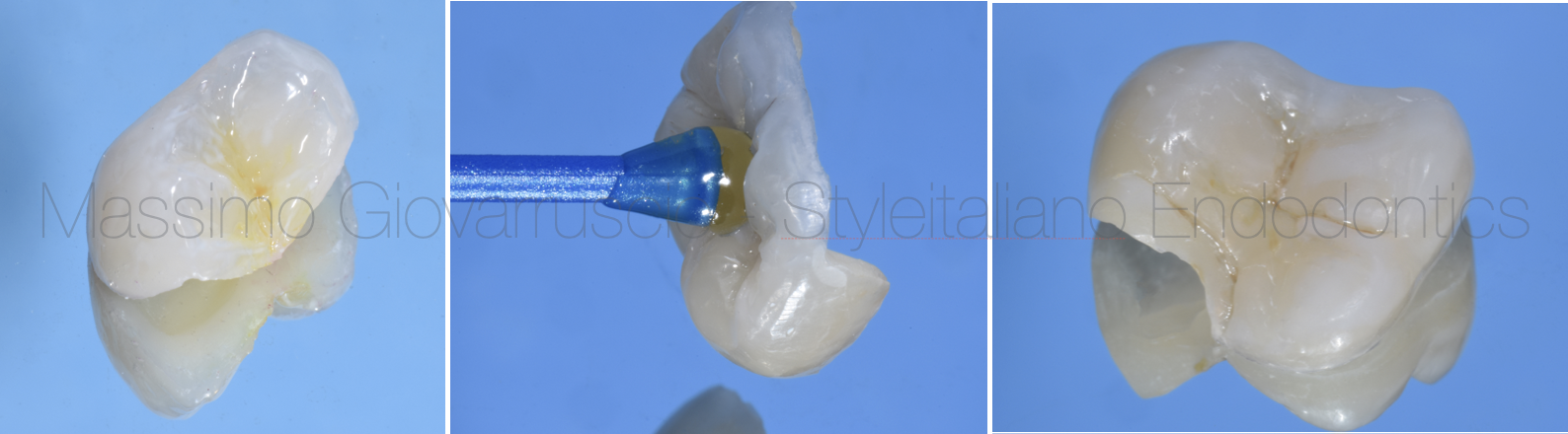
Fig. 15
These preparation principles may be effectively used for all adhesively cemented restorations, both according to traditional concepts (inlay, onlay, overlay) and new ones (additional overlay, occlusal veneer, overlay-veneer, long-wrap overlay, adhesive crown). Thus, a balance between restoration and prosthodontics is created, which is characterized by a more conservative and minimally invasive approach
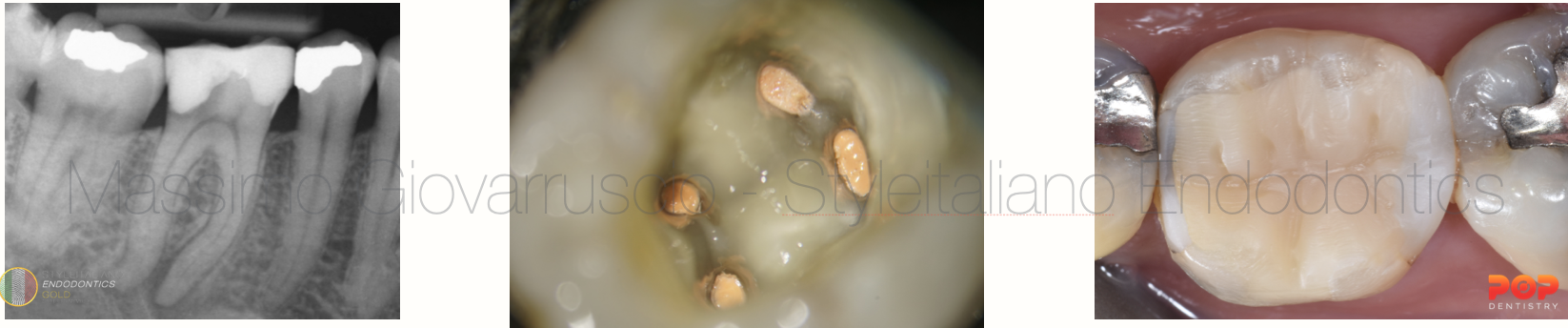
Fig. 16
Clinical case
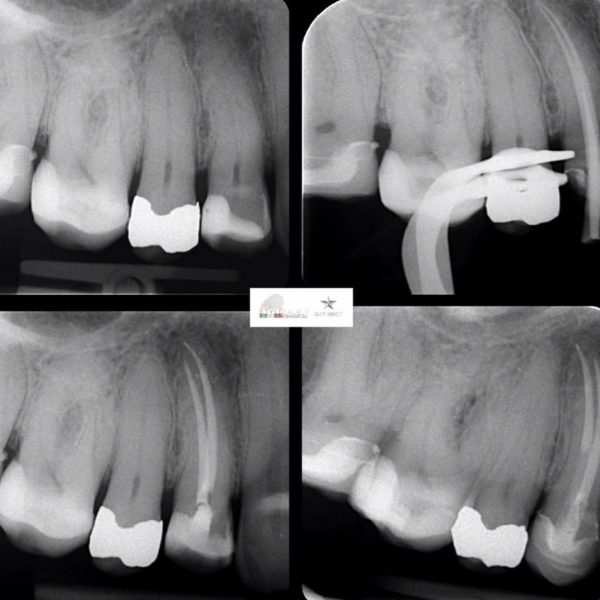
A 32 years old patient with has been referred to me to perform root canal treatment on the lower first molar
On clinical examination, the patient presents severe toothache and pain while biting. The Pre-operative X-ray shows a long and curved anatomy.
The root canal has been performed on all root canal system (ML, MB,Dl andDB canal). Minimal invasive files has been used to preserve the pericervical dentine and to respect the complex root canal anatomy. The chamber has been restored with dual-core restoration.
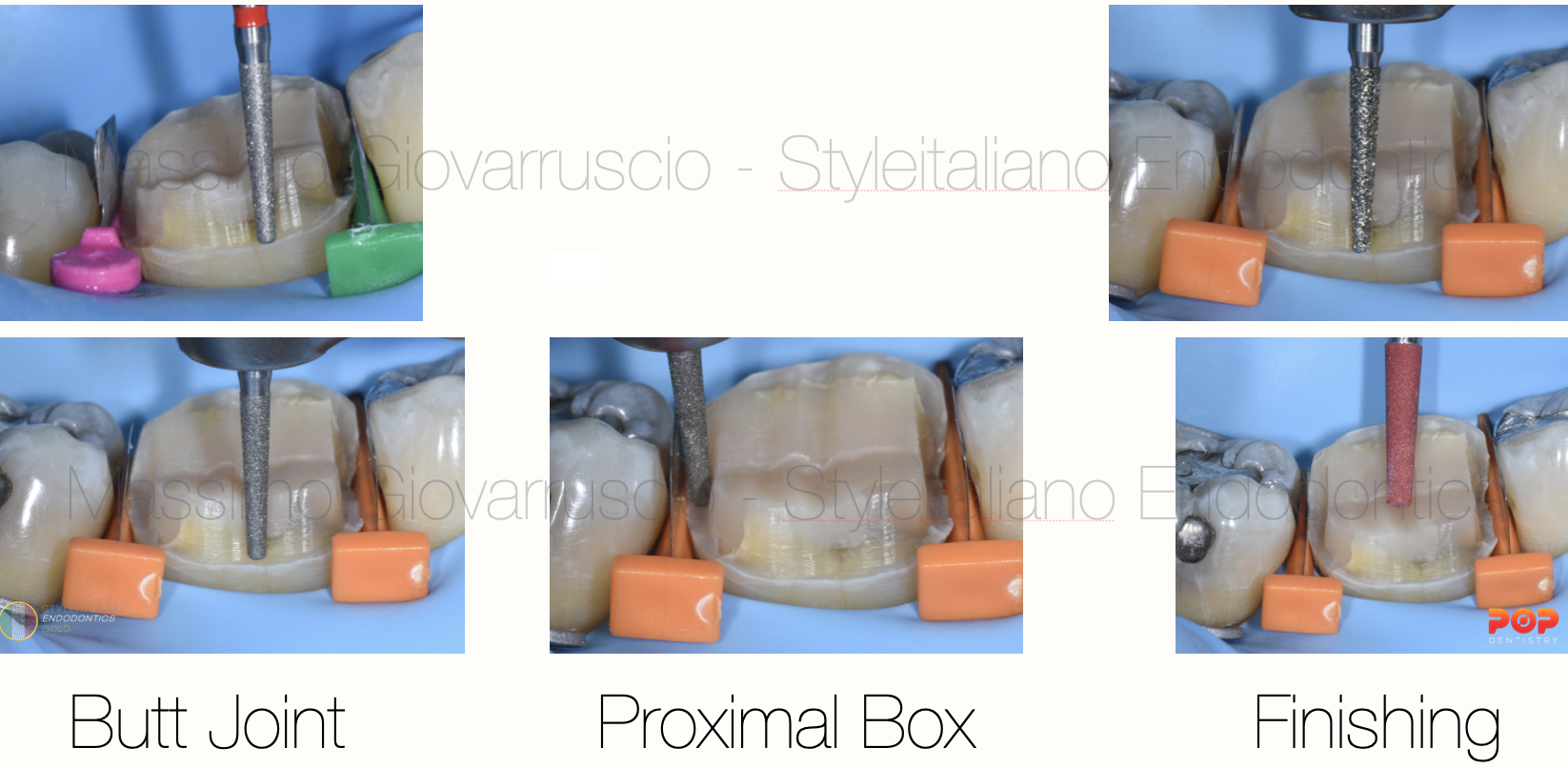
Fig. 17
Tooth preparation using selected burs

Fig. 18
ONLAY MDPT PREP
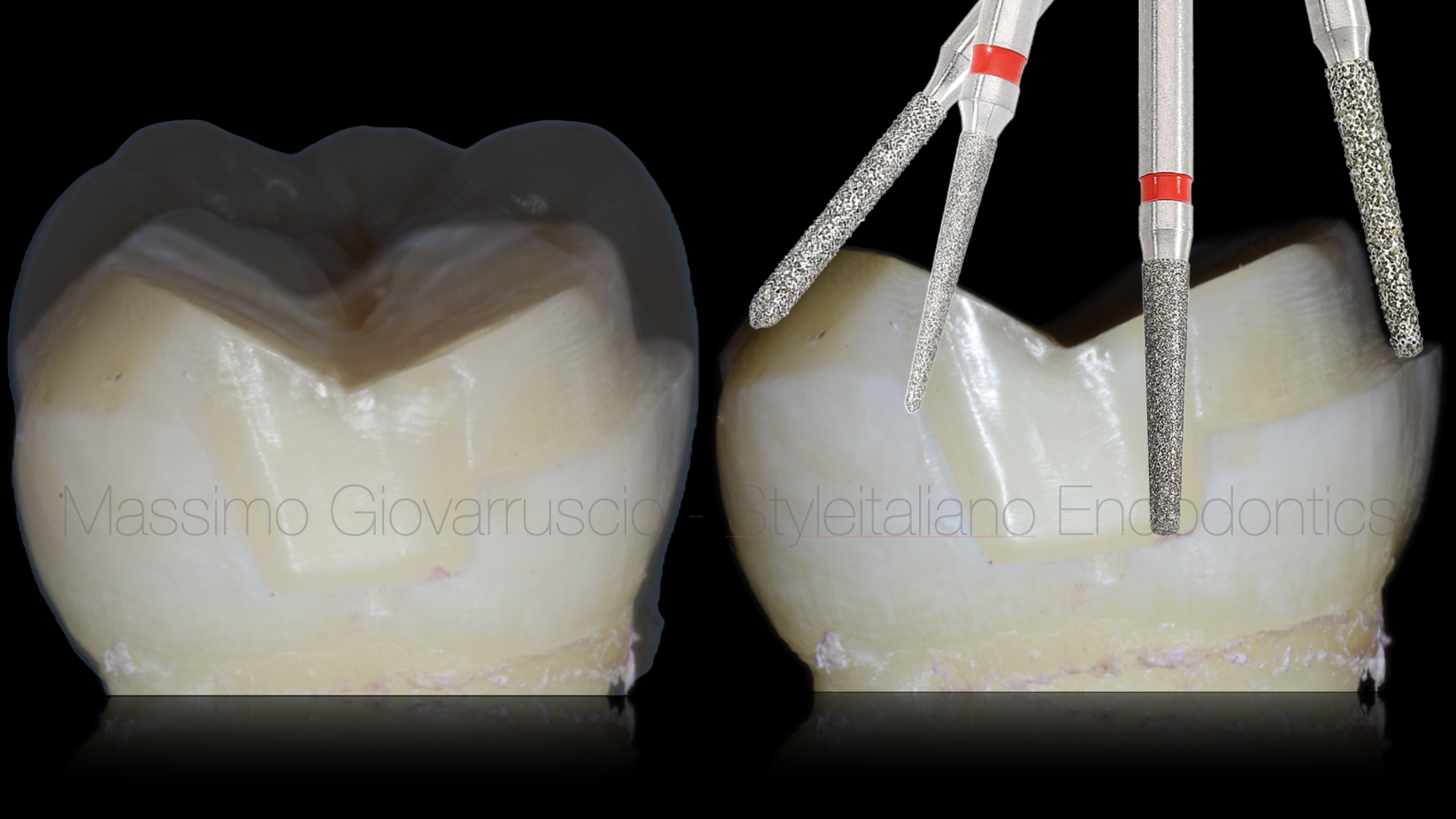
Fig. 19
Preparation
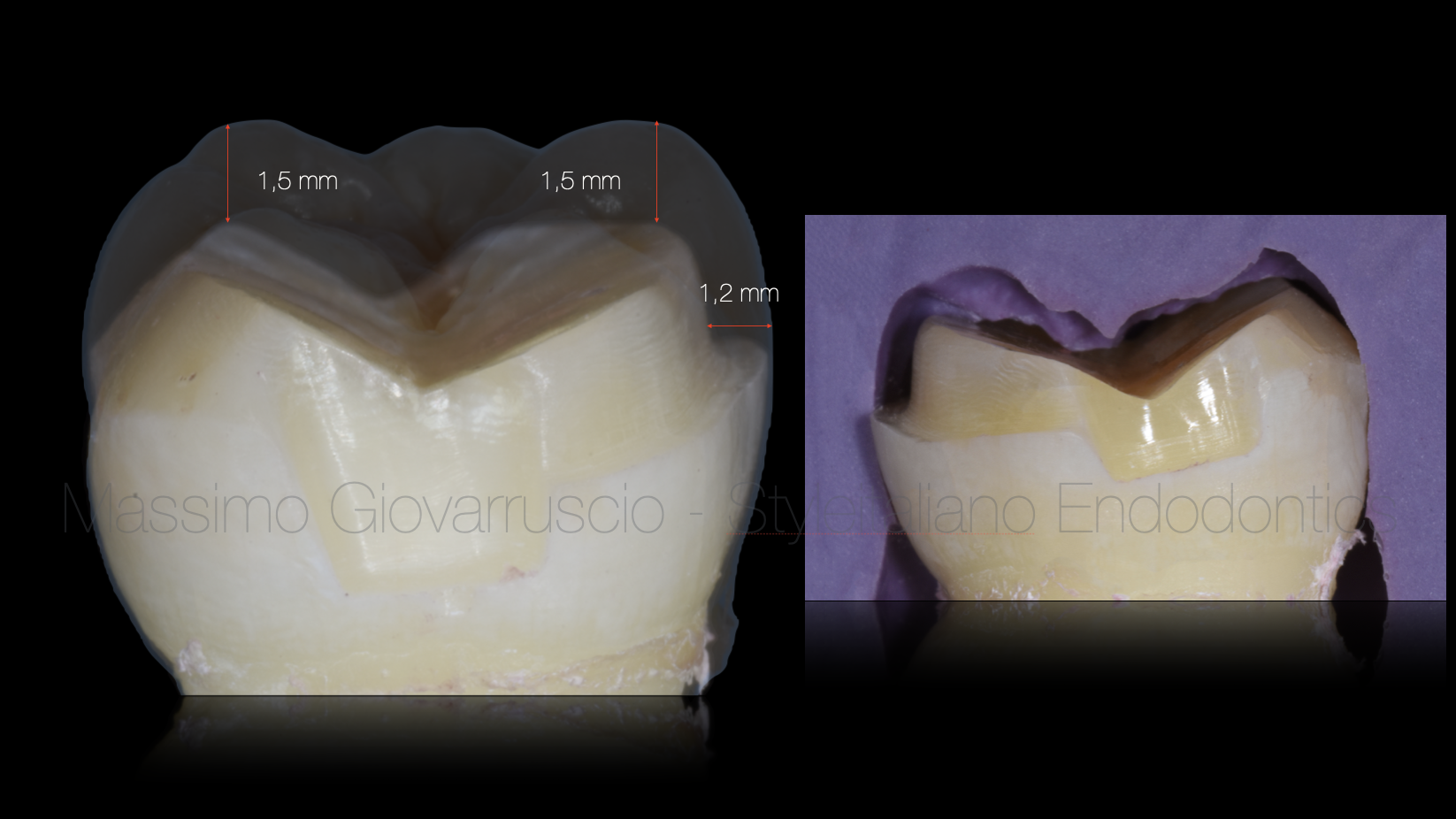
Fig. 20
Reduction

Fig. 21
ONLAY MDPT PREP
Mandibular molars and premolars

Fig. 22
Cavity design definition after root canal and adhesive build-up, for overlay.
Composite build-up with immediate dentin sealing (IDS), and, if necessary, Cervical Margin Relocation (CMR).
Preparation and finishing of the cavity according to new modified principles (morphology driven preparation
technique – MDPT).

Fig. 23
Overlay preparation
- Etch the internal surface of the overlay with hydrofluoric acid (if the composite overlay manufacturer recommends it).
- Rinse and dry the overlay thoroughly.
- Apply a silane coupling agent to the etched surface, allowing it to air dry
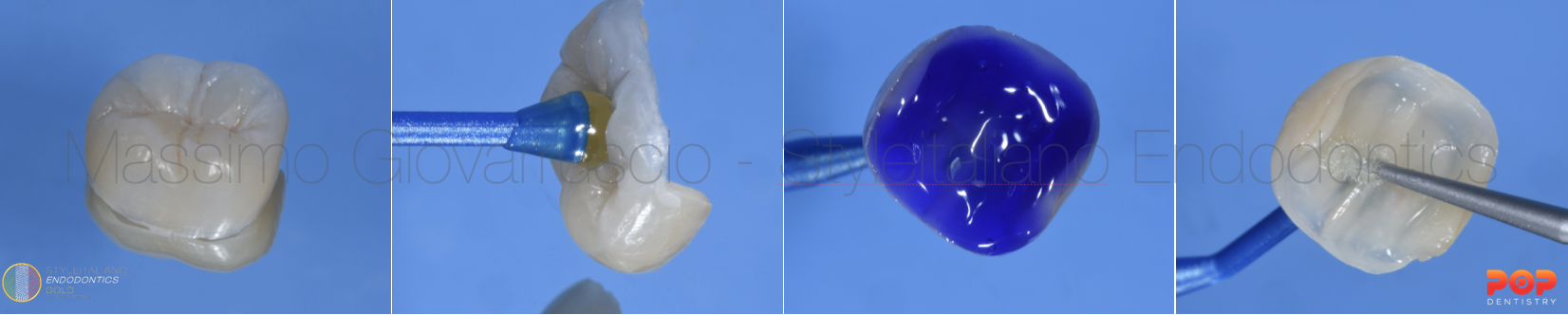
Fig. 24
Adhesive cementation procedure
a. Select the Right Cement (In this case Composite has been used)
- Use a light-cure resin cement suitable for composite overlays
b. Apply the heated Cement (Heated composite helps the cementation procedures)
- Coat the internal surface of the overlay with a thin, even layer of resin cement.
c. Seating the Overlay
- Carefully place the overlay onto the prepared tooth, ensuring complete seating without gaps.
- Apply gentle pressure to minimize the cement layer thickness.
- Using ultrasonic tip helps the overlay for a better sitting
d. Remove Excess Cement
- Gently tack-cure the margins for 1–2 seconds to stabilize the restoration.
- Remove excess cement with a floss and scaler or micro-brush before final curing.

Fig. 25
Restoration after adhesive cementation with esthetic restoration. Root canal procedure shows a minimal invasive treatment of all 4 canals. Restoration with morphology and functional buccal appearance
Conclusions
Preserving dental healthy tissue and pericervical dentine, has become the priority for a better conservative and minimal invasive approach.
With this technique, indirect adhesive restorations are indicated in large cavities associated with cuspal coverage.
This new cavity design allows for the following clinical advantages:
Improve adhesion quality through the optimization of the enamel cutting and the creation of a greater surface of enamel.
Minimal dentin exposure, avoiding wide shoulders, occlusal slots, and wells.
Maximum preservation of healthy residual tissue, adapting the cavity design to adhesive cementation procedures with composite resins, and improving the flow of excess material.
Optimization of the esthetic performance, which allows for better blending in the transition zones.
The new principles of preparation discussed in this article can be applied effectively to all types of traditional adhesive restorations (inlay, onlay, overlay)
Bibliography
-Veneziani M. “Posterior indirect adhesive restorations: updated indications and the Morphology Driven Preparation Technique” Int J Esther Dent 2017;12(2):204-230
-Dietschi D, Spreafico R. “Current clinical conceptsfor adhesive cementation oftooth-colored posterior restorations.” Pract PeriodonticsAesthet Dent 1998;10: 47–54.
-Magne P, Kim TH, CascioneD, Donovan TE. “Immediate dentin sealing improves bond strength of indirect restorations.” J Prosthet Dent 2005;94: 511–519.
-Veneziani M. “Adhesive restorations in the posterior area with subgingival cervical margins: new classification and differentiated treatment approach.” Eur J Esthet Dent 2010;5: 50–76.
-Bazos P, Magne P. “Bioemulation: biomimetically emulating nature utilizing a histo-anatomic approach;
structural analysis.” Eur J Esthet Dent 2011;6: 8–19.