
Non-vital tooth bleaching
02/09/2014
The Community
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
In this article the protocol of non-vital bleaching of extensively discolored anterior teeth was described with practical tips for practitioners. The more detailed protocols and more clinical cases can be found in author’s book edited by Quintessence (Warsaw, 2013, Polish language): “Endoprosthodontics: guidelines for clinical practice”
Dentist should always consider teeth bleaching at the beginning of the esthetic treatment plan, regardless of the method that will be chosen – conservative or prosthodontic. There are different reasons of teeth discolorations: beginning from changes connected to age of the patient and ending with trauma or tooth necrosis. Nowadays, in contemporary dental practice, applying the wright protocol we can achieve sufficient results with bleaching, even in case of endodontically treated discoloured teeth.

Fig. 1

Fig. 2
In summer 2004, 25-year-old woman reported to the authors office with a desire to improve her smile by esthetic full ceramic crowns(patients citation). Her chief concerns included extensive discolorations of teeth 11, 21 (Fig. 1, Fig 2) .
Because of malocclusion, orthodontic treatment was discussed but has been rejected by the patient.
From the patients interview it was concluded that patient underwent endodontic treatment around 12 years ago and gradually discolorations appeared within few years after.
The following treatment plan was proposed:
In phase 1. endodontic retreatment (root canals were filled by paste not gutapercha), fiber post placement and replacement of existing composite restorations
As teeth discoloration was extensive, the phase 2. was considered depending on the result of the non-vital bleaching.
The phase 2. assumed covering the teeth with porcelain veneers or full ceramic crowns.
RETREATMENT

Fig. 3

Fig. 4

Fig. 5

Fig. 6

Fig. 7
In order to understand the position of the periodontal ligaments during the barrier placement, the length between the interdental papilla and the incisal edge was measured with periodontal probe and transferred to the pulp chamber.

Fig. 8

Fig. 9

Fig. 10
The barrier was created with glass- ionomer cement in semilunar shape to protect the periodontal ligament from the diffusion of bleaching agent while allowing for diffusion towards discolored buccal wall of the tooth.
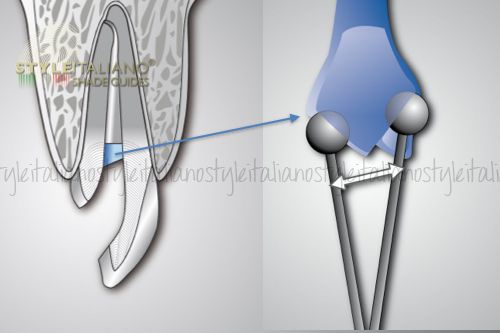
Fig. 11
Prolonged 10 minutes setting time of the glass ionomer was calculated to achieve stabile barrier.
The position of the barrier and appropriate shape is extremely important for the safety and final result of the bleaching.
BLEACHING AGENT PLACEMENT

Fig. 12
The bleaching agent was prepared in situ from Natrium Perborate Tetrahydrate mixed with 3% hydrogen peroxide and the paste of wet snow consistency was obtained. The bleaching agent was applied to the pulp chamber with spatula instrument and condensed with wet cotton pellet.
As temporary material GI cement was used . The patient was informed about increased risk of the fracture during the bleaching procedure.

Fig. 13
The bleaching agent was replaced twice in next appointments: 7 days and 14 days following the first bleaching appointment.
As satisfactory bonding to bleached dental hard tissues can be achieved after a period of 2 weeks, during this period the color of the bleached tooth stabilized and a calcium hydroxide dressing was placed in the pulp cavity in order to buffer the acid pH that can occur on cervical root surfaces after intra-coronal application of bleaching agents.

Fig. 14

Fig. 15
Surprisingly good result of non-vital bleaching put aside the decision about tooth preparation and indirect restoration.
Two weeks after the bleaching has been completed, appointment for teeth reconstruction has been scheduled. The old restorations and GI cement from temporary restoration and barrier was removed and canals were prepared to place fiber posts without additional hard dental tissue reduction but only by removing of gutta-percha with Gates instruments and in microscope magnification.

Fig. 16

Fig. 17

Fig. 18
After adjustment of fiber posts the dentin has been cleaned with 50 µm of Aluminium Oxide, etched with phosphoric acid (Fig 16), irrigated by distillate water and delicately dried with air stream and paper points (Fig 17). Then Bonding agent (Enabond) mixed with the chemical catalizator (EnaCat) was applied in 2 layers onto the dentin and sprayed by air (Fig 18).

Fig. 19

Fig. 20
A first layer of ligther dentin (UD1, Enamel Plus) composite was placed palatally towards the buccal wall of the teeth (Fig 19-20).

Fig. 21
Afterwards the fiber posts (EnaPost) of opalescent effect characteristics were cemented into the canal.

Fig. 22
Composite reconstruction was made.

Fig. 23
Clinical result on month after bleaching and composite reconstruction.

Fig. 24
The comparison between initial situation and final result shows that surprisingly great result can be achieved in case of root canal discolored teeth bleaching (Fig24).
To prolong the good result of bleaching and prevent the discoloration reoccurrence, the special bleaching trays can be applied with buccal and lingual reservoir for bleaching agent. In bleaching maintenance protocol patient should be instructed to re-bleach the previously discolored teeth once a 6 months for a period of 7 nights.
Conclusions
1.Bleaching of root canal treated discolored tooth with Natrium Perborate Tetrahydrate should be considered as a first option in esthetic treatment plan.
2. The precise removal of the old cements, restorations, pulp remnants , as well as the exact barrier placement under the microscope magnification are crucial in effective non-vital teeth beaching.
3. The knowledge of proper patient indication for non-vital bleaching, barrier placement and calcium hydroxide dressing constitute important elements in order to prevent external cervical resorption.
4.Delate adhesive bonding (at least 14 days) and preventive bleaching trays can play important role in bleach teeth color maintenance.
Bibliography
- Zarow M, D’arcangelo C, Paolone G, Felipe L, Paniz G; Endoprosthodontics – Clinical Guide for Dental Practitioners; Quintessence Int , Warsaw, 2013
- Plotino G, Buono L, Grande NM, Pameijer CH, Somma F. Nonvital tooth bleaching: a review of the literature and clinical procedures. J Endod. 2008; 34(4):394-407.
- Lado, E.A., Bleaching of endodontically treated teeth: an update on cervical resorption. Gen Dent, 1988. 36(6): p. 500-1.
- Dietschi, D., Nonvital bleaching: general considerations and report of two failure cases. Eur J Esthet Dent, 2006. 1(1): p. 52-61.
- Paolone G, Saracinelli M, Devoto W, Putignano A. Esthetic direct restorations in endodontically treated anterior teeth. Eur J Esthet Dent. 2013; 8(1):44-67.



