MB2: locating and accessing
09/10/2023
Fellow
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
As we know, the presence of a 4th canal in upper molars is highly frequent, especially in the first molar but also in the 2nd molar. According to the literature, in the first molar it is present in more than 90%, while in the 2nd molar, its presence is above 50%.
We know that when this canal is not treated, the risk of endodontic failure increases, being the main cause of endodontic failure in these teeth.
The management of this canal during endodontic treatment is usually more complex, both because of its location, since it is frequently under a wall of dentin, and because of its size, since it is usually narrower and more sinuous than the rest of the canals.
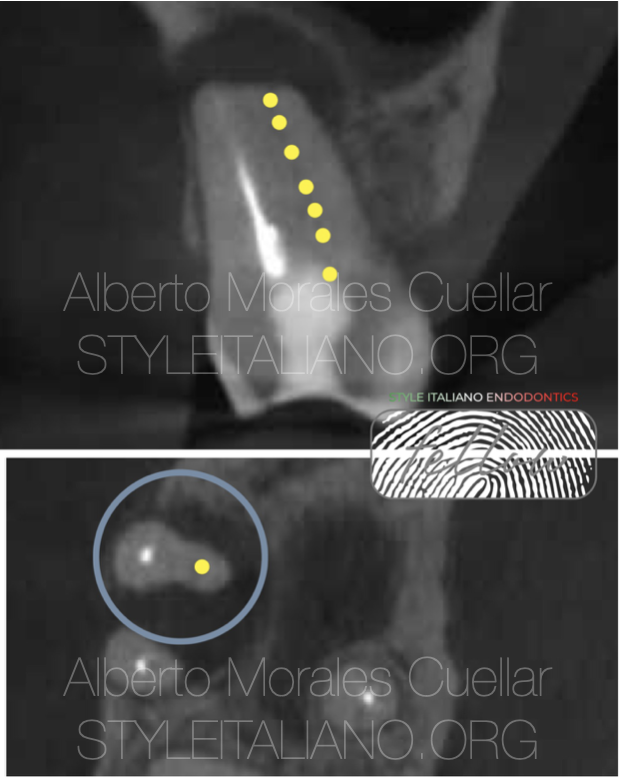
Fig. 1
To treat this canal, first of all, we must identify its presence. To do this, we have a very helpful tool, such as CBCT, where we can observe its presence or sometimes, by analyzing the shape of the root in the axial section, assume of his presence. CBCT helps us minimize the limitations of periapical radiography in this purpose.

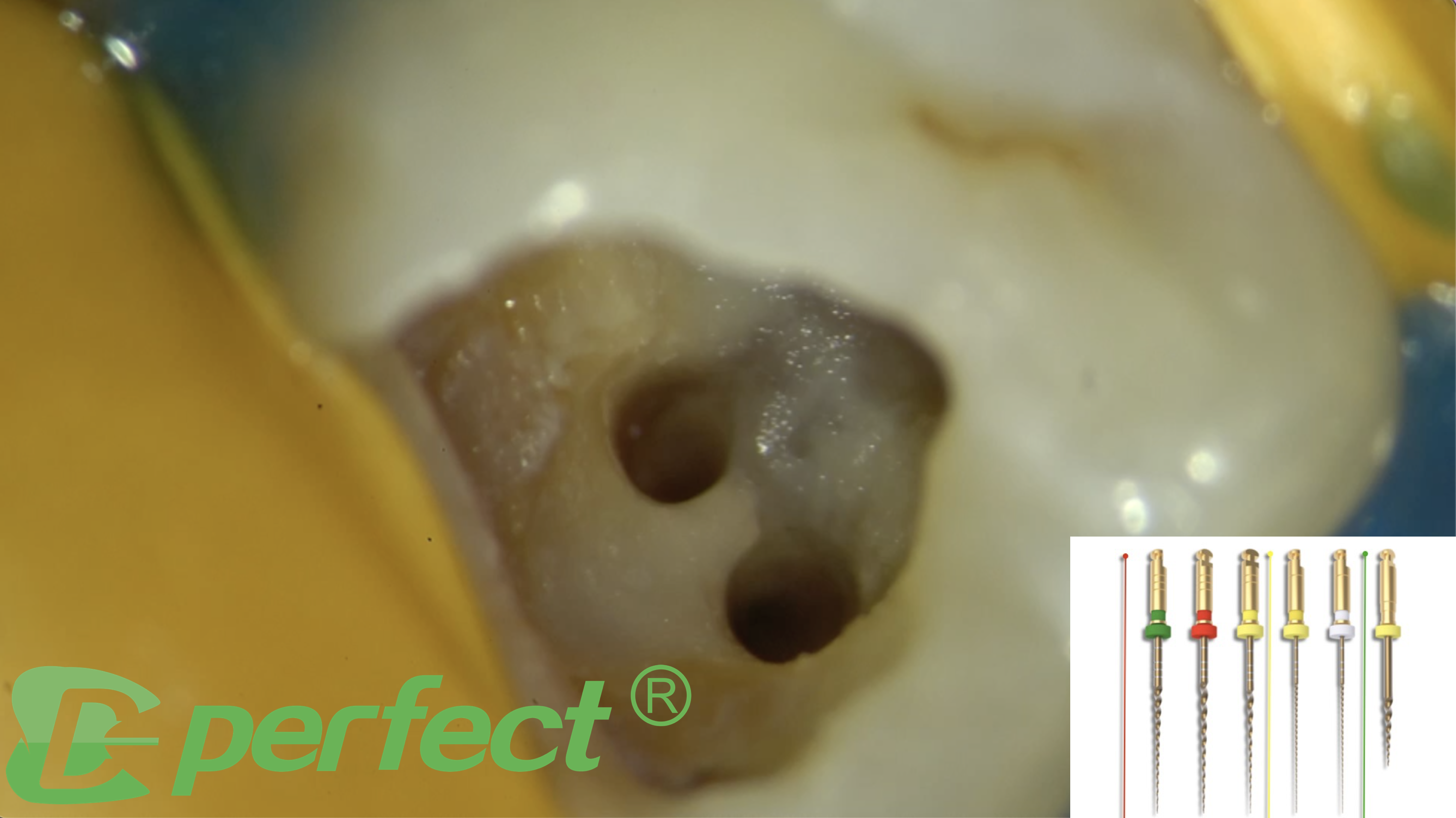
Fig. 2
Images from previous case before and after shape MB2 canal.
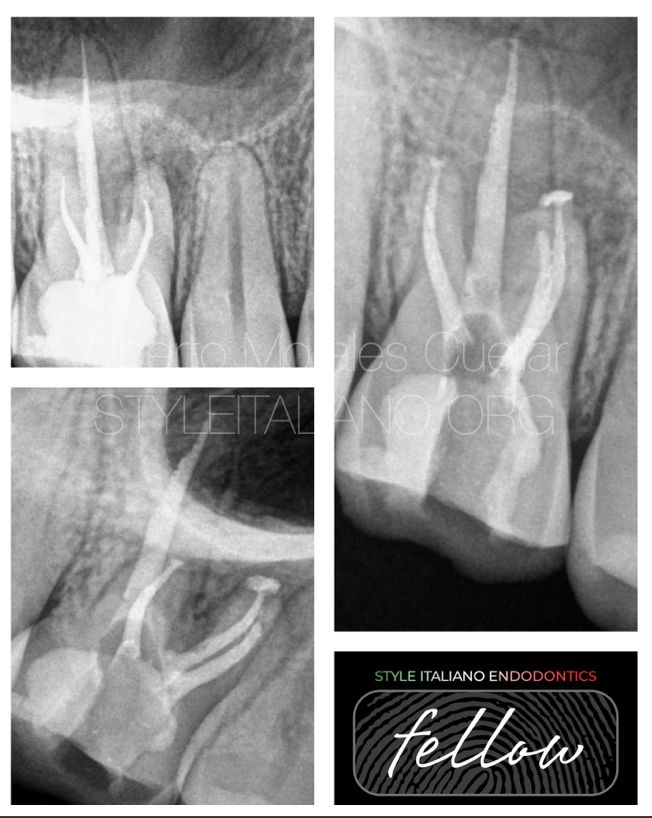
Fig. 3
X- ray from previous case.
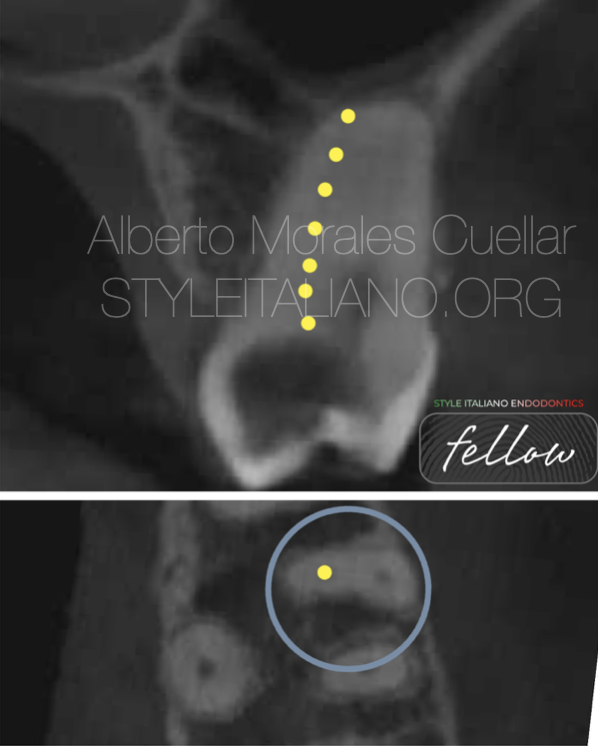
Fig. 4
Other case where CBCT help to locate MB2 entrance.

Fig. 5
Case completed
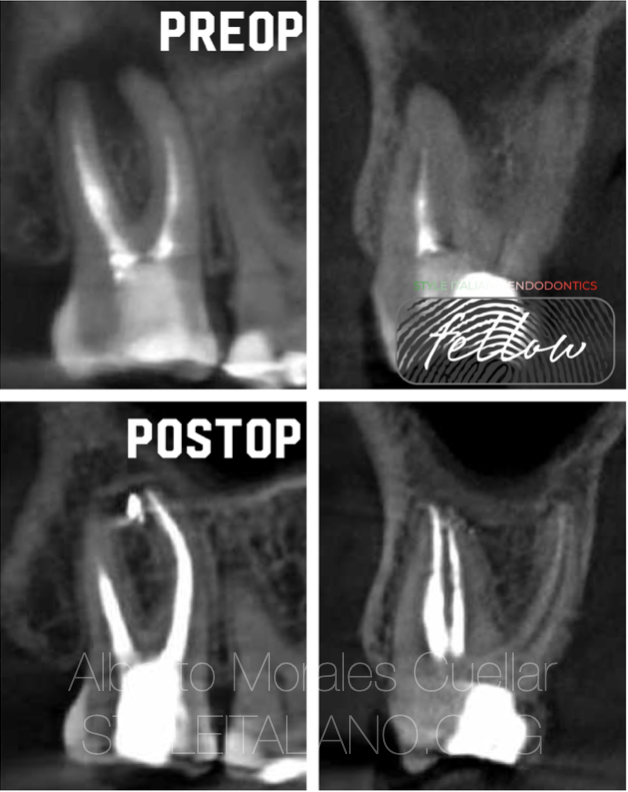
Fig. 6
The presence of untreated MB2 canal is one of the most frequent cause for endodontic failure in upper molars.
As we can see in this endotontic retreatment of a second molar, after correct endodontic retreatment, endodontic lesion is healing.
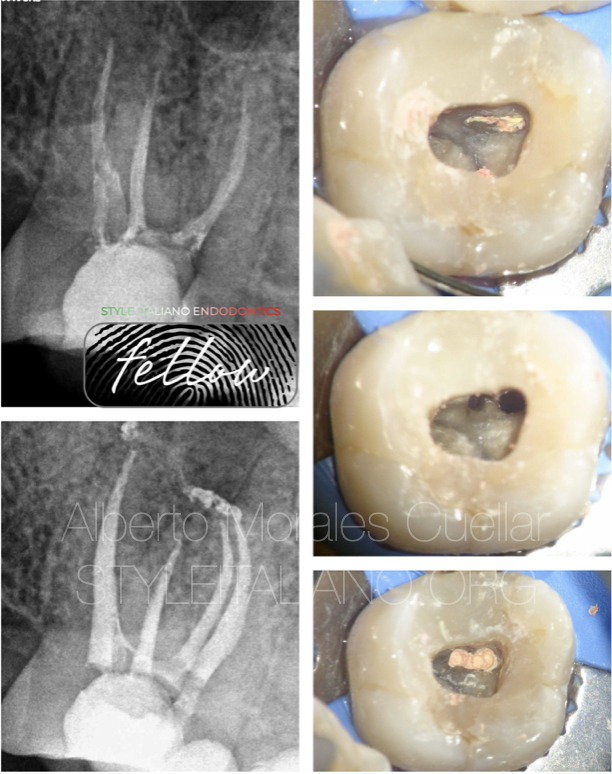
Fig. 7
Images and x-rays of previous retreatment.

Fig. 8
Another case failure, because of missed MB2.
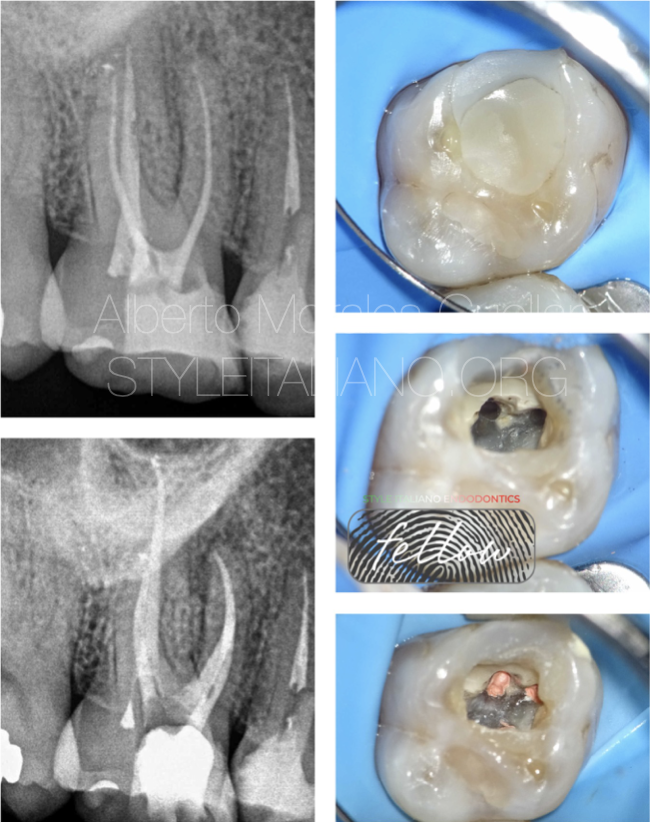
Fig. 9
Case after location and treatment of MB2 canal.
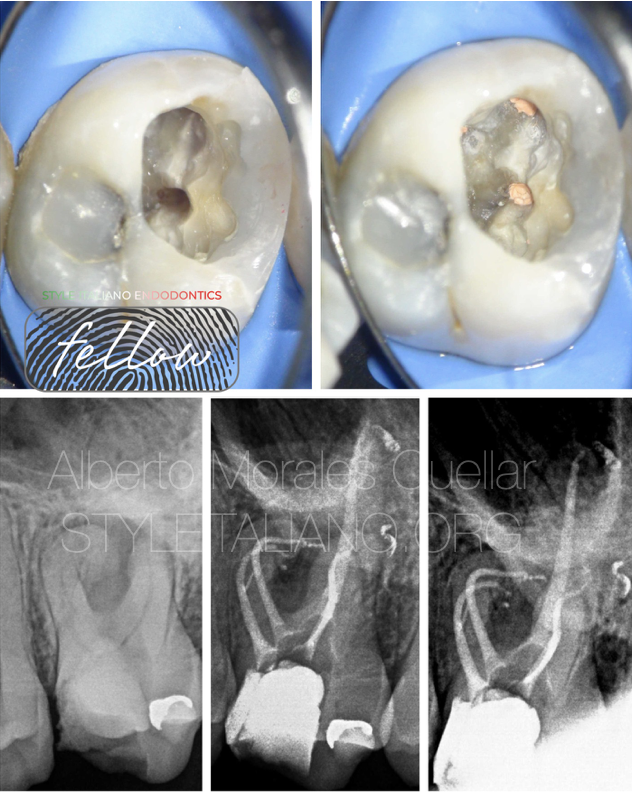
Fig. 10
Once we suspect its presence, the next step is to have correct access to it.
To do this, we must have a correct access cavity, which we will later refine with ultrasonic, to selectively remove the dentin that normally covers the entrance of the canal.
The use of ultrasound allows us to be more precise and conservative, due to better control of the cut and better visualization.
With ultrasonic, we remove dentine where we suspect the canal is located.
The next tool that we will need will be the use of magnification and correct lighting, ideally, the use of an operating microscope will help us visualize it.
We must also take into account that its location will be visual, so we must work with mirrors that correctly reflect light, are not damaged and reduce our visibility and we can correctly analyze the colors of the pulp chamber.
They allow us to perfectly observe the color changes that exist in the map of the floor of the pulp chamber.
Once we have access in a straight line to the entrance of the canal, with the DG16 probe we will look for the point where the entrance of the duct may be, and to permeabilize the first millimeters, we can use a microopener (file with handle) that will allow us to have good visibility and will help us penetrate that narrower canal.
We can “activate” the micro opener with ultrasonic vibration to modify the access or to mechanically clean the isthmus between MB1 and MB2.
If the canal is very narrow, once we have entered the first millimeters with the microopener, we can use a C plus 08 file to make the coronal part permeable.
In my case, I like to use an 18 mm file, as it will give us greater sensitivity tactile.
We can manage the manual file with the pliers in order to have better vision of the procedure.
Once the coronal third has been opened with file 08 and 10, we will perform preflaring, a very important step before trying to access the apical third, since we will eliminate coronal interferences, and we will be able to better access the apical third, which we will make permeable with a K-file file of little size.
Once we reach the apical level, we will treat it as a complex case, but we will have already overcome the most difficult part.

Fig. 11
About the author
Alberto Morales Cuellar
Degree in dentistry at the Complutense University of Madrid, 2013
Master in Advanced Endodontics at Rey Juan Carlos University, 2017
Master Periodontics and soft tissue management at CEU Cardenal Herrera, 2020
Professor of Master of Microscopic Endodontics and Apical Surgery (URJC)
Opinion leader of Zarc4Endo
Style Italiano Endodontics Fellow member
Full member of the Spanish Association of Endodontics.
Member of the American Association of Endodontists.
Winner of the Best Training Presentation of the College of Dentists of Madrid
Conclusions
The MB2 canal can be difficult to treat, so we must have the knowledge and appropriate tools to manage it.
CBCT, microscope, quality mirrors, ultrasound, microopener and manual files can be tools that help us treat the first millimeters in these more complex canals.
Bibliography
Fernandes NA, Herbst D, Postma TC, Bunn BK. The prevalence of second canals in the mesiobuccal root of maxillary molars: A cone beam computed tomography study. Aust Endod J. 2019 Apr;45(1):46-50. doi: 10.1111/aej.12263. Epub 2018 Mar 23. PMID: 29573065.
Sujith R, Dhananjaya K, Chaurasia VR, Kasigari D, Veerabhadrappa AC, Naik S. Microscope magnification and ultrasonic precision guidance for location and negotiation of second mesiobuccal canal: An in vivo study. J Int Soc Prev Community Dent. 2014 Dec;4(Suppl 3):S209-12. doi: 10.4103/2231-0762.149045. PMID: 25625081; PMCID: PMC4304061.
Tabassum S, Khan FR. Failure of endodontic treatment: The usual suspects. Eur J Dent. 2016 Jan-Mar;10(1):144-147. doi: 10.4103/1305-7456.175682. PMID: 27011754; PMCID: PMC4784145.
Chakradhar Raju RV, Sathe N, Morisetty PK, Veeramachaneni C. Endodontic management of a maxillary first molar with unusual location of second mesio buccal orifice. J Conserv Dent. 2010 Jul;13(3):162-4. doi: 10.4103/0972-0707.71652. PMID: 21116395; PMCID: PMC2980616.
Chi-Chun Su, Ren-Yeong Huang, Yu-Chiao Wu, Wan-Chien Cheng, Ho-Sheng Chiang, Ming-Pang Chung, Yi-Wen Cathy Tsai, Chi-Hsiang Chung, Yi-Shing Shieh,
Detection and location of second mesiobuccal canal in permanent maxillary teeth: A cone-beam computed tomography analysis in a Taiwanese population,