Management of Iatrogenic Furcal Perforation in tooth with obliterated root canal
28/10/2020
José Conde Pais
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Perforation is a pathologic or iatrogenic communication between root canal system and the supporting tissues of teeth or the oral cavity. Root perforations are common complications of endodontic treatment or post preparation and often lead to tooth extraction.
Iatrogenic root perforations occur in approximately 2‑12% of endodontically treated teeth. Successful treatment depends mainly on immediate sealing of the perforation and prevention of infection. Root perforations adversely affect the prognosis of teeth. Several factors related to infection of the perforation site affect the prognosis of the treatment of root perforations, the most important of which are: time between occurrence and treatment size, and location of the perforation. The essential requirement for repair of root perforations is the use of cements with physical, chemical and biological properties that neither adversely affect cells involved in the repair process nor act as a foreign body. Mineral trioxide aggregate (MTA) is being successfully used to repair perforations .
MTA is an endodontic cement that is extremely biocompatible, hydrophilic, and capable of stimulating the healing processes and osteogenesis. An important problem associated with the use of some cements is the difficulty to limit the amount of cement placed in the perforation canal. The lack of a barrier or stop at the moment of condensation of the cement results in extrusion of obturation material into the periodontal space. In order to remediate this problem, some authors have indicated the use of an internal matrix that acts as a barrier, preventing extrusion of cement.
This case report shows how to solve these types of complications.
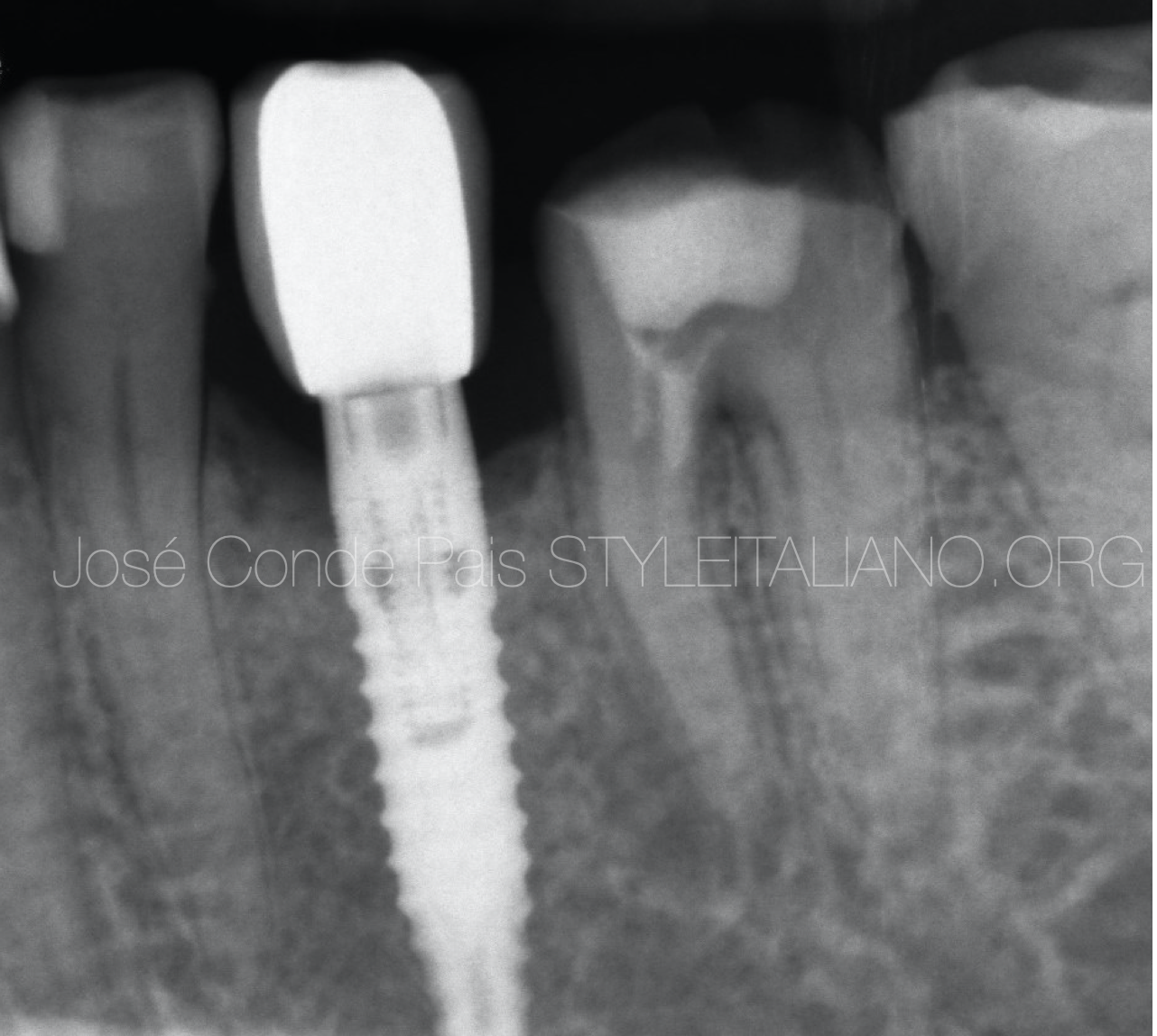
Fig. 1
A 60 years old male patient was referred from a general Practitioner to my clinic for management of furcal perforation and root canal treatment.
After a clinical and radiographic examination, we observe the following :
Tooth 36 presents an iatrogenic furcal perforation , obliterated pulp canal, asymptomatic apical periodontitis and physiological probing.
We explain the situation to the patient and decide on a non-surgical approach under surgical microscope.

Fig. 2
Initial situation: We remove temporary cement and cotton using a Ultrasonic Tip

Fig. 3
Once the temporary filling was removed, poor furcal perforation sealing was found (possibly MTA). We decided to clean and seal it again under a surgical microscope.
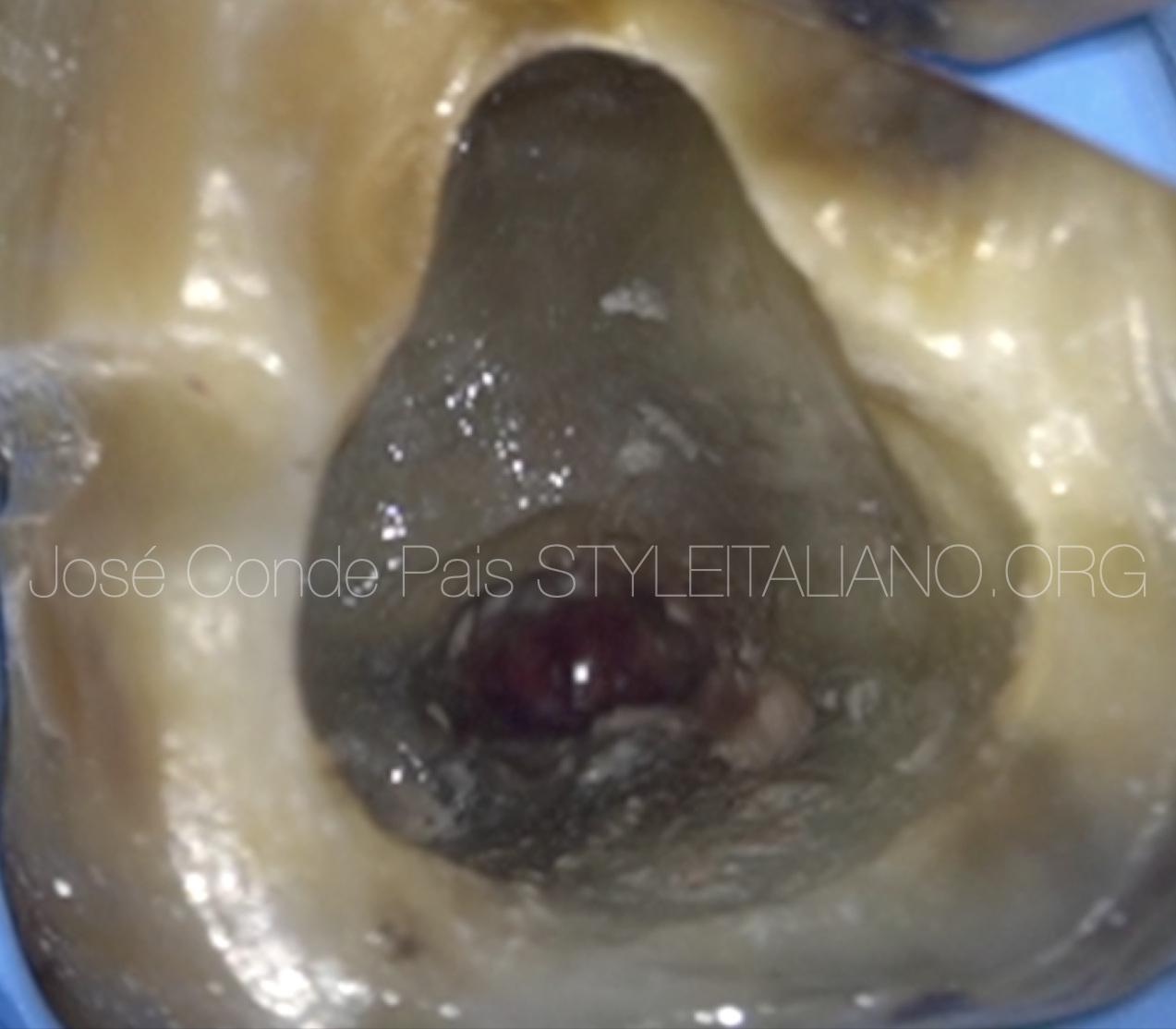
Fig. 4
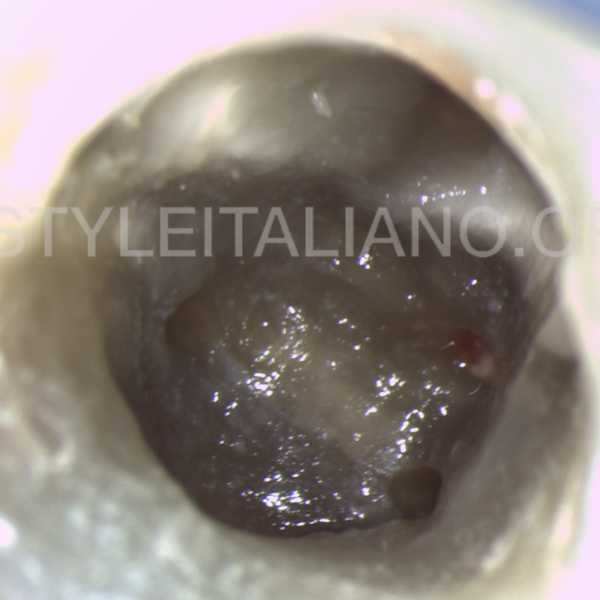
A tapered ultrasonic tip was used to remove the old MTA. In this image we can see the perforation located between the mesial canals.
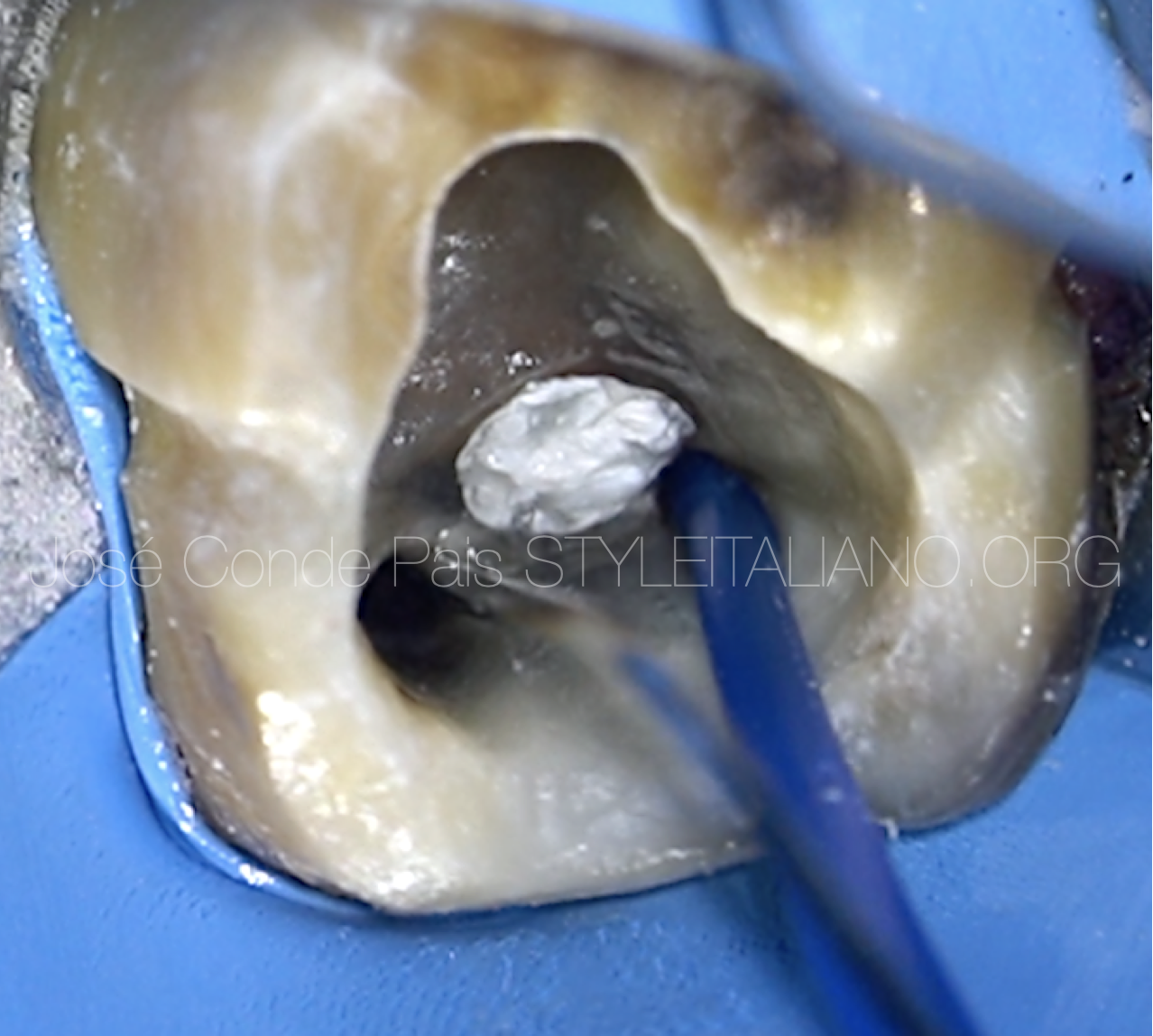
Fig. 5
After cleaning the perforation, we temporarily sealed it with sterile Teflon and proceeded to the location and instrumentation of the root canals. In this image we can see how the confluence is cleaned by a continuous flow of irrigant (5.25% sodium hypochlorite).
The following protocol was used in root canal treatment:
Glide Path ; #08 C+, #10 C+
Preflaring ; Proglider File
Instrumentation ; Protaper Next X1, X2
Irrigation; Sodium hypochlorite 5,25% + Saline Solution+ Edta 17% PUI + sodium hypochlorite 5,25% PUI
Obturation; Continuous Wave + Conform Fit #25 *+ AH
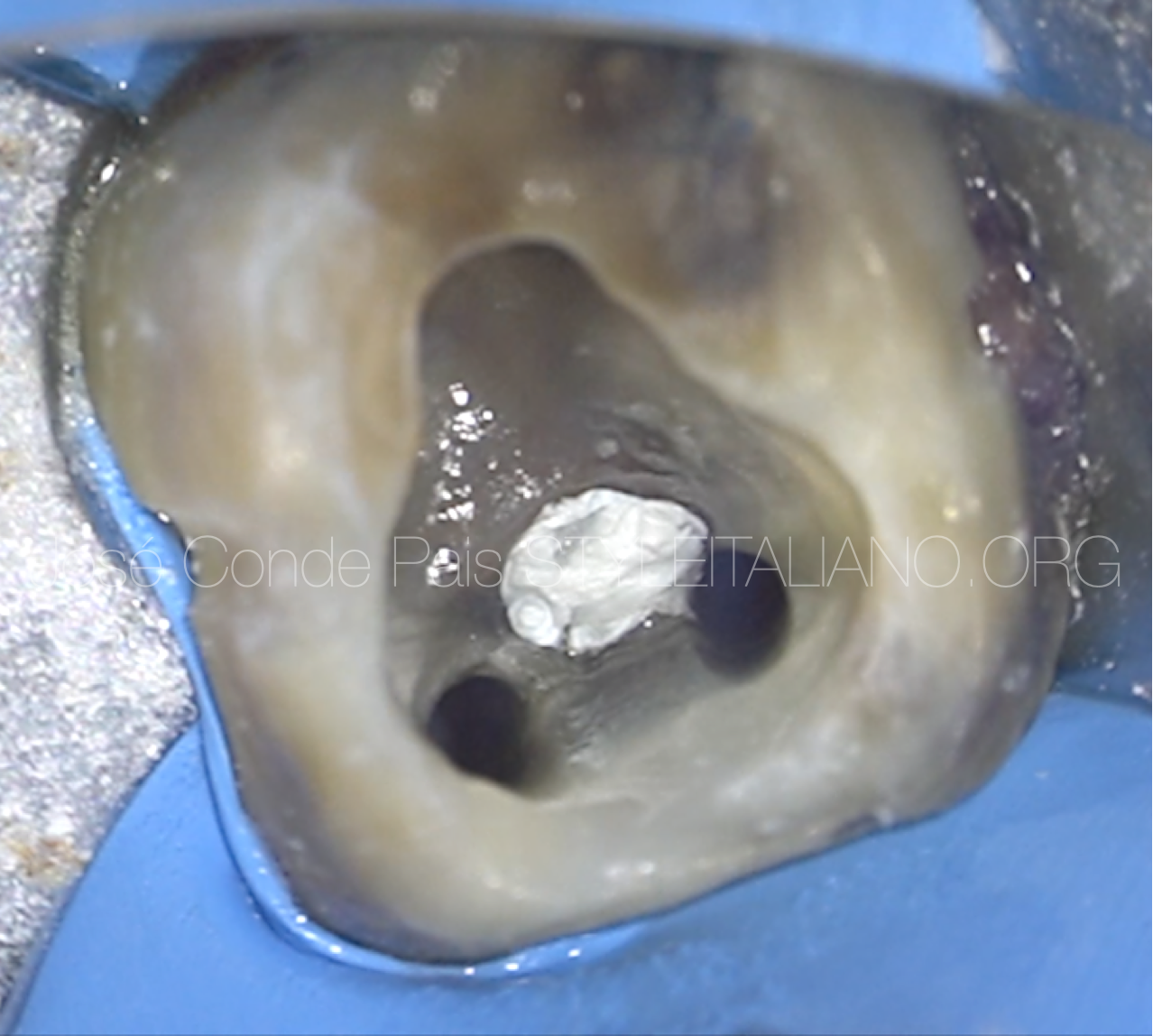
Fig. 6
This image shows the situation before root canal filling.
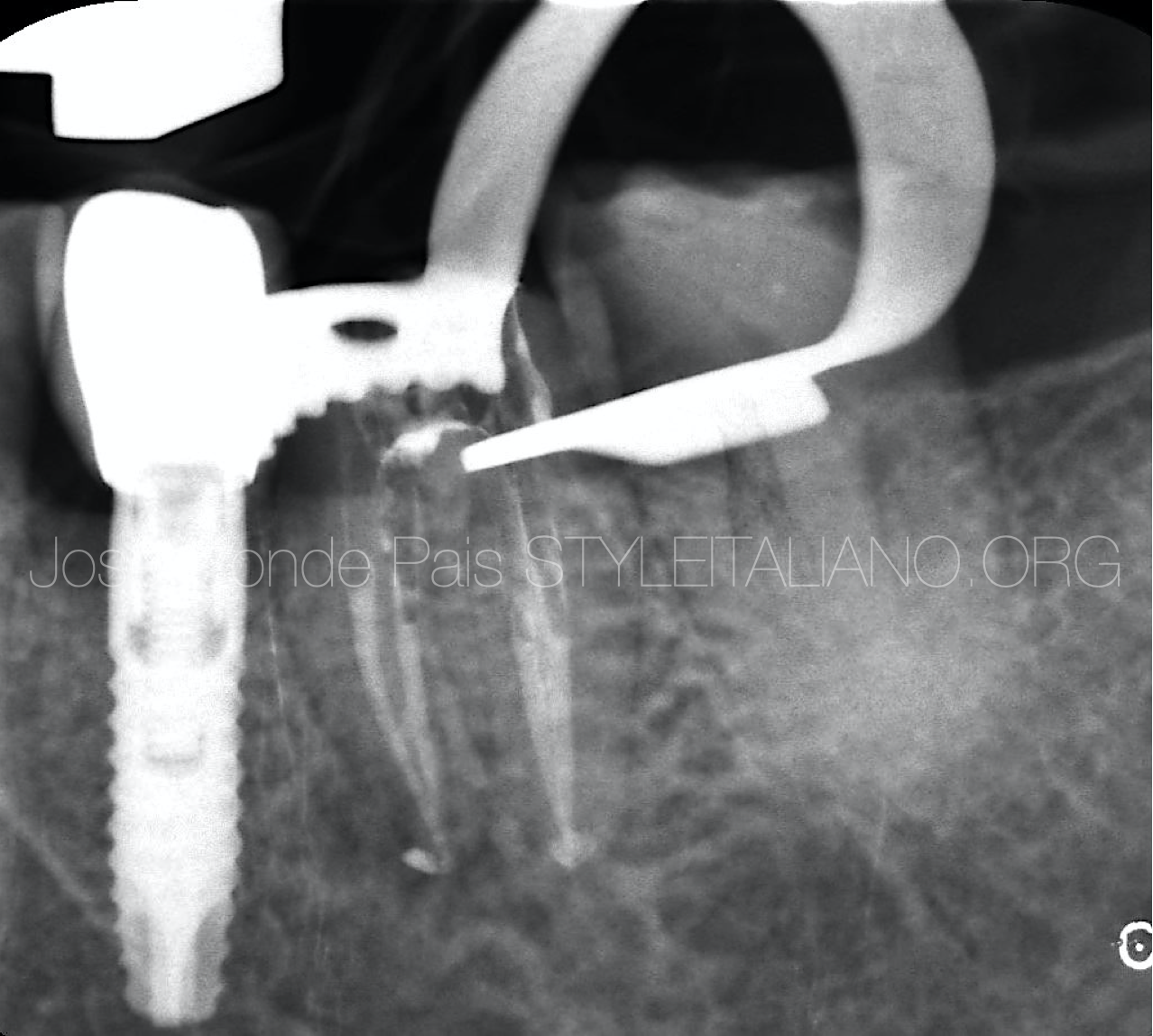
Fig. 7
Downpack x-ray

Fig. 8
Root canal filling with continuous wave of condensation of gutta percha.

Fig. 9
Collagen matrix was placed in the perforation to prevent mta extrusion.

Fig. 10
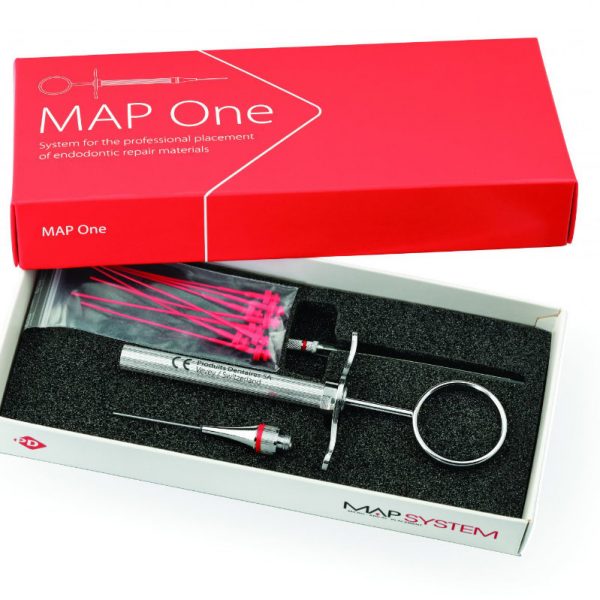
To seal the perforation, MTA was used. It was placed with the MAP System (Produits Dentaires SA, Vevey, Switzerland), which allows us a simple and predictable use of bioceramic cement.

Fig. 11
Image of repaired furcal perforation and root canal treatment performed

Fig. 12
Final Orthoradial xRay
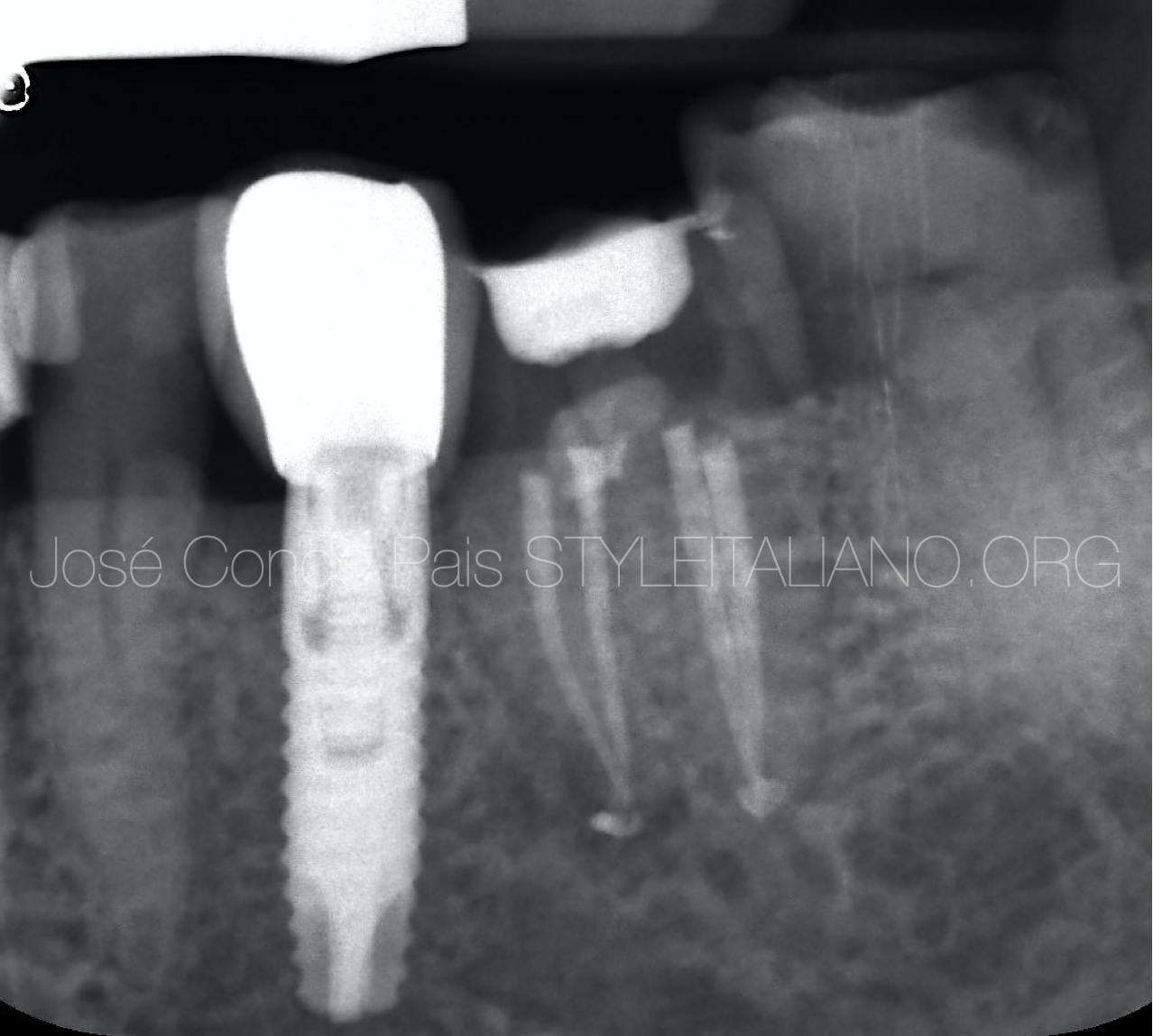
Fig. 13
Final Mesioradial xRay .
Full case video
Conclusions
We can conclude that the non surgical approach is predictable, conservative and with su cess rates above 70%.
In view of the relatively high rate of clinical success, nonsurgical repair may be considered as the preferred treatment to handle this complication that arises during root canal therapy. We consider that the use of the magnification and the MAP System Kit are of great help in handling these cases.
Bibliography
Fuss Z. Trope M. Root perforations: classification and treatment choices based on prognostic factors. Endod Dent Traumatol. 1996; 12: 255-264
Sinkar RC, Patil SS, Jogad NP, Gade VJ. Comparison of sealing ability of ProRoot MTA, RetroMTA, and Biodentine as furcation repair materials: An ultraviolet spectrophotometric analysis. J Conserv Dent. ; 2015;18(6):445–8.
Parirokh M, Torabinejad M, Dummer PMH. Mineral trioxide aggregate and other bioactive endodontic cements: An updated overview - part I: Vital pulp therapy. Int Endod J. 2017;1–34.