
Internal inflammatory root resorption: a case report
26/06/2020
João Meirinhos
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Internal root resorption is rare in permanent teeth. The altered canal anatomy resultant from the resorptive process poses a challenge for the chemo-mechanical debridement and sealing of the root canal. The purpose of this article is to report the successful treatment of an upper central incisor with an internal root resorption.

Fig. 1
Internal root resorption is a rare occurrence in the permanent dentition, more frequently found in maxillary incisors and with a slight predilection for males. Trauma is considered the major etiological factor, and for the inflammatory resorptive process to be sustained, vital tissue must be present apical to the resorption. Teeth are usually asymptomatic and are occasionally detected during routine radiological examinations. Internal resorption is often confused with external resorption, and a careful differential diagnosis is necessary to proceed with the appropriate therapy. The use of Cone Beam Computerized Tomography (CBCT) is considered essential for a correct assessment of the location, shape and size of the dentinal defect. Because the resorptive defect is the result of an inflamed pulp and the clastic precursor cells are predominantly recruited through the blood vessels, controlling the process of internal root resorption is conceptually easy, by interrupting the blood supply to the resorbing tissues with conventional root canal therapy.

Fig. 2
A 41-year-old male patient was referred to the Postgraduate Specialization Course in Endodontics at the Faculty of Dental Medicine of the University of Lisbon (FMDUL) to evaluate the upper central incisor after the referring colleague detected and usual canal anatomy on a periodical radiograph.
The patient reported a history of trauma 10 years ago. There was no obvious discoloration. The maxillary central incisor was diagnosed with necrotic pulp and normal periapical tissues. Radiographic examination revealed a well-defined radiolucency in the middle third of tooth 11, compatible with internal resorption

Fig. 3
After clinical and radiographic examination, a CBCT was requested as a complementary diagnosis means and for treatment planning. The CBCT images aided in the diagnosis of inflammatory non-perforating internal resorption for tooth 11. As a treatment plan, non-surgical endodontic treatment was suggested and accepted by the patient.
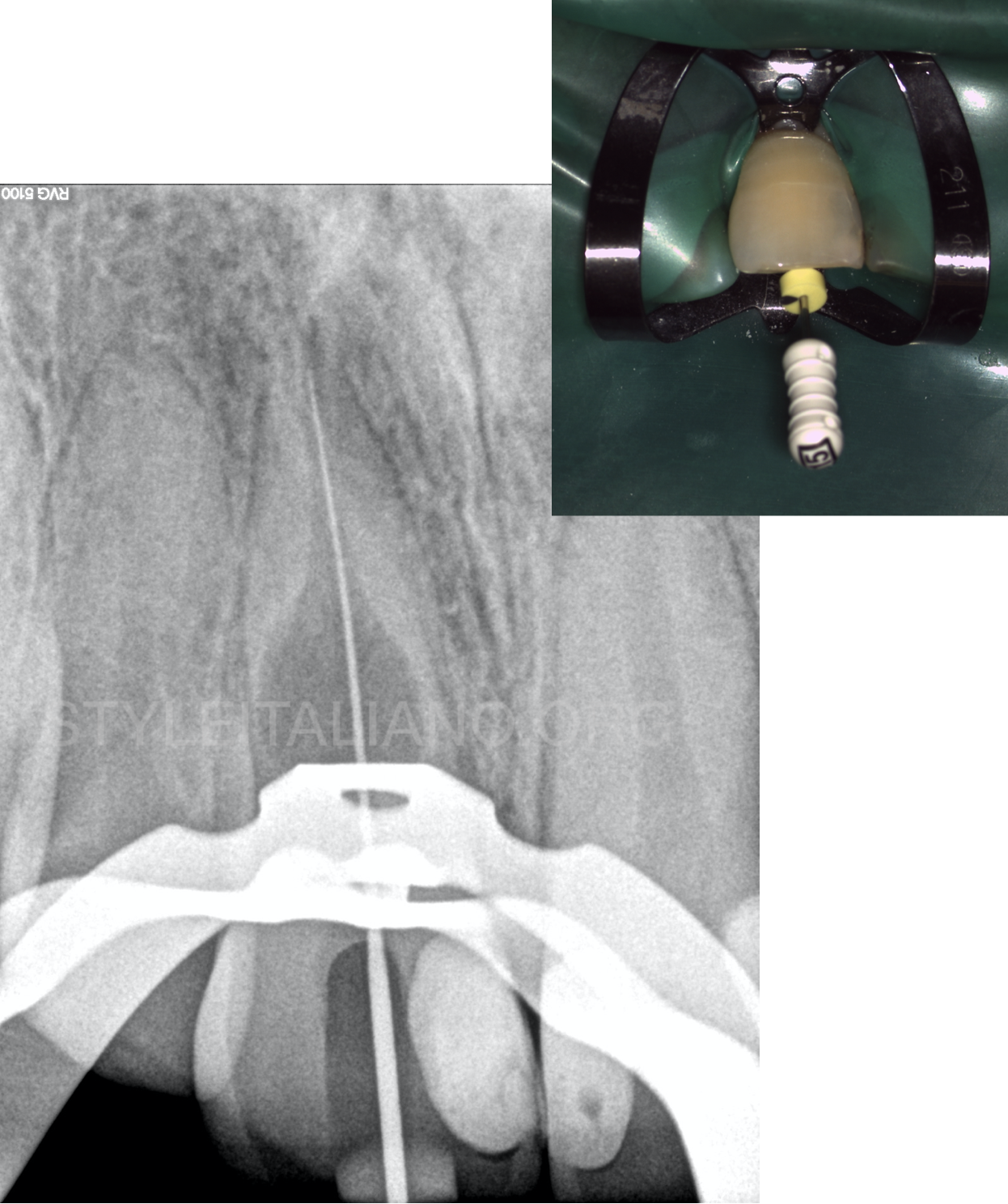
Fig. 4
The treatment was performed under an operating microscope, in 2 appointments. Upon establishing access with Ultrasonic tips, the canal was scouted with 10k and 15k stainless-steel hand files. Working length was established with the help of an electronic apex locator and confirmed radiographically.
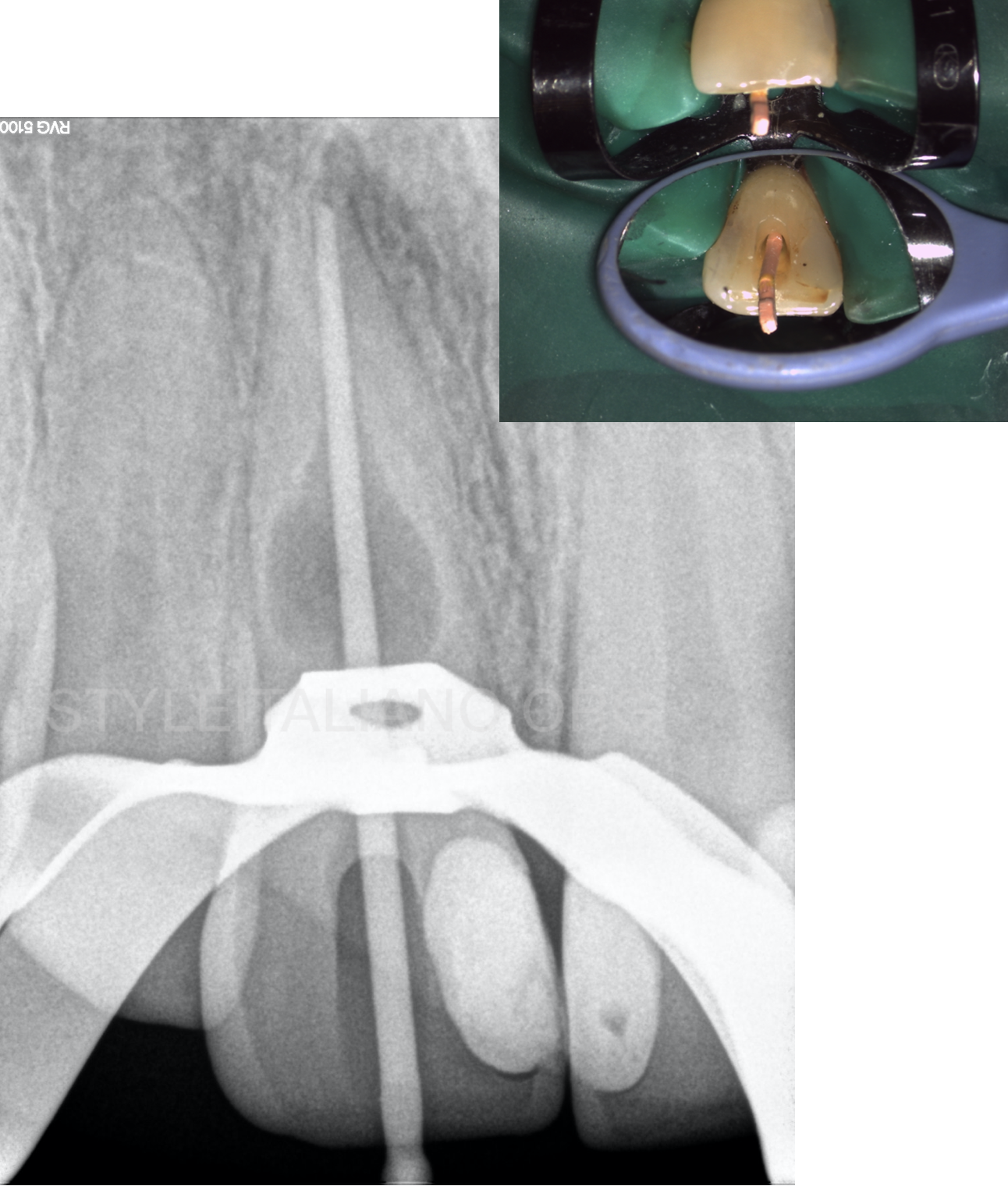
Fig. 5
The canal was shaped with reciprocating files according to the manufacturer’s instructions.
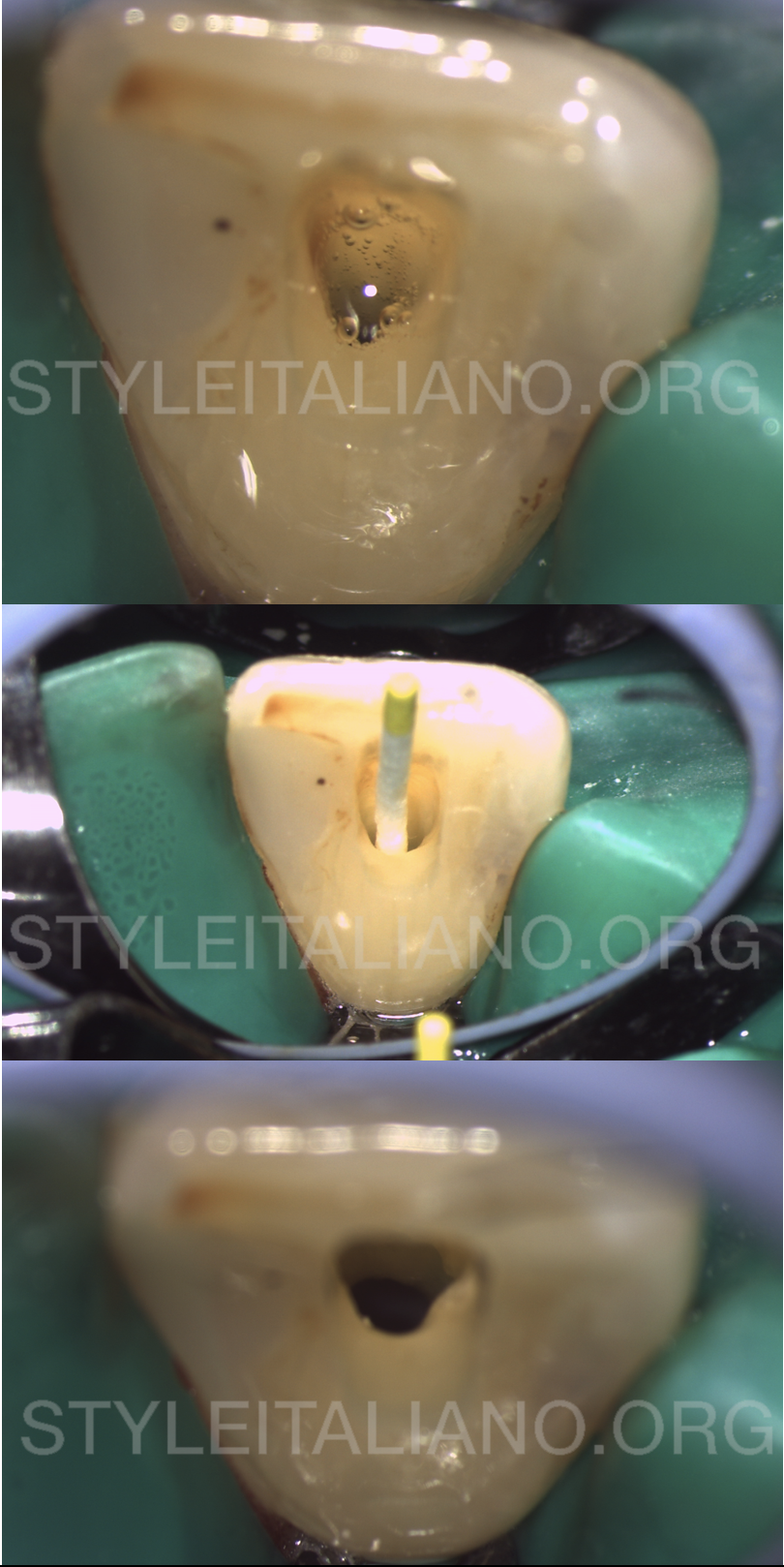
Fig. 6
Copious irrigation with 5mL syringe and a 27G notched needle with 5,25% sodium hypochlorite was done all throughout the endodontic treatment, as well as ultrasonic irrigation using ultrasonic tips. After the final irrigation protocol, that included a flush with 17% EDTA, the canals were dried with paper points.
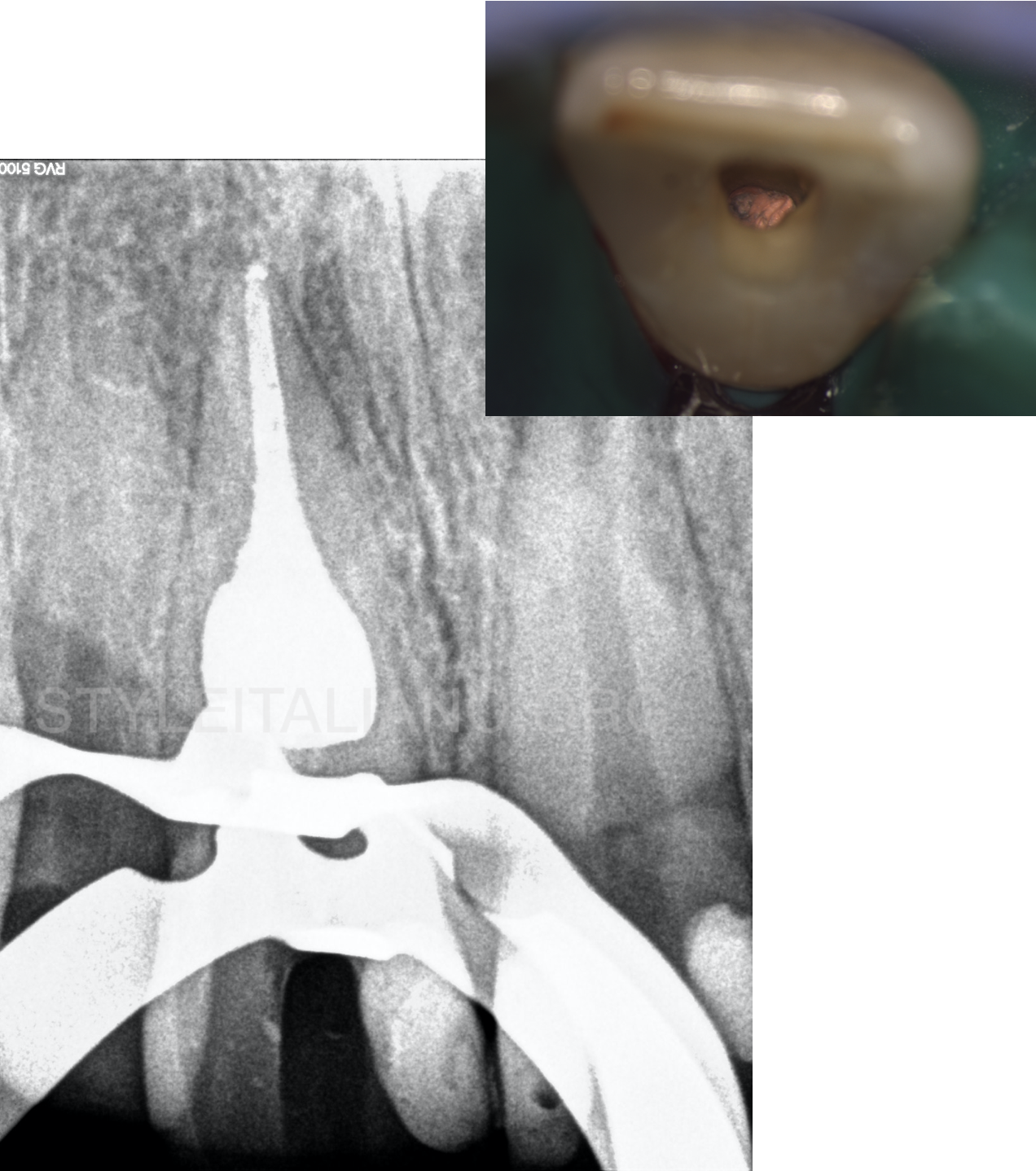
Fig. 7
The canal was filled with gutta-percha and resin sealer with a continuous wave of obturation technique.

Fig. 8
Intracoronal sealing was done with a flowable composite resin and the crown was subsequently restored directly with composite resin.

Fig. 9
At 6 months, the patient remained free of symptoms.
Conclusions
Root canal treatment remains the only treatment of choice for teeth diagnosed with internal resorption. Early detection and a correct differential diagnosis are essential for successful management of internal resorption. The goal of endodontic therapy is the removal of the inflammatory tissue and three-dimensional shaping, cleaning and filling of the enlarged canal space, while also avoiding unnecessary removal of dentin that could further weaken the remaining tooth structure.
Bibliography
- Fuss, Z., Tsesis, I., & Lin, S. (2003). Root resorption - diagnosis, classification and treatment choices based on stimulation factors. Dental Traumatology, 19(4), 175–182.
- Haapasalo, M., & Endal, U. (2006). Internal inflammatory root resorption: the unknown resorption of the tooth. Endodontic Topics, 14(1), 60–79.
- Heithersay GS. Management of tooth resorption. Australian Dental Journal. 2007 Mar 1;52(s1).
- Patel, S., Ricucci, D., Durak, C., & Tay, F. (2010). Internal Root Resorption: A Review. Journal of Endodontics, 36(7), 1107–1121.
- Gabor, C., Tam, E., Shen, Y., & Haapasalo, M. (2012). Prevalence of Internal Inflammatory Root Resorption. Journal of Endodontics, 38(1), 24–27.


