Good Manners for Good Endodontists
07/07/2017
Calogero Bugea
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Not one dentist I know who doesn’t find, in his daily practice, teeth that are earmarked for RCT (e.g. emergency, destructive caries, prothesis treatment planning) or that have had an RCT and need further treatment (e.g. post-endodontic build-up, fiber post positioning, prosthetic abutment preparation, orthodontic extrusion and so on).
For this reason even if Endodontics is a specialty that requires a lot of studying, long learning curve and specific armamentarium, each one of us has to deal with this discipline following some simple basic rules, in order to increase the success rates in RCT and the patient’s comfort, while decreasing the operative times of the endodontic treatment together with the patient’s stress.
On the other hand, it’s advisable for the endodontist to be able to do a proper composite restoration, crown lengthening, etc… and he must facilitate the work of the colleagues that will follow the patient after the endodontic treatment.
Outer sealing of the endodontic space. The most common mistake at the end of the endodontic treatment, even if a second session scheduled, is the lack of sealing of your own work.In order to facilitate a comprehensive treatment, it is very important to follow these simple rules.

Fig. 1
Presence of plaque and calculus. Patients come into the dental office, sometimes to begin a restorative treatment or with pain. Obviously, even when it come to endodontics, working with healthy tissues is better than inflamed tissues; working in a clean manner without plaque is even better. Placement of the rubber dam and restoration procedures are much easier in a healthy mouth thus providing a cleaner and safer environment for the operator. In case of emergencies, even if the primary aim of the appointment is, obviously, to eliminate the pain, we always have to think of the next steps to be taken: scaling of the area only requires a few minutes and improves workflow. Of course, an appointment with the hygienist is mandatory to decrease the amount of bacteria. This simple step plays a fundamental role in the following restorative procedures.

Fig. 2
Caries elimination. It’s imperative to remove caries prior to performing an endodontic treatment. A thorough cleaning of the cavity before starting an RCT is mandatory in order to work in an environment that is as clean as possible.

Fig. 3
Pre-endodontic restoration. In general pre-endodontic restorations can be avoided if you complete the treatment in one visit. If you think that you can’t finish the endodontic therapy in one session or a complication occurs during treatment, you must create a perfect sealing of the access. Schilder said: “it’s more important what you keep out than what you put in”; the evolution of this concept is: it’s better to protect the endodontic space than putting a paste inside it.

Fig. 4
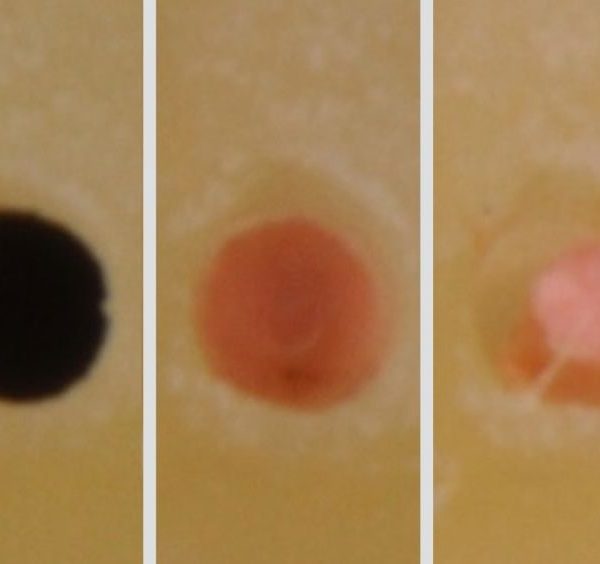
Leaving a tooth open only in case of pulpitis or necrosis is a really wrong approach; bacteria can enter the Root Canal System and the biofilm can be then very hard to remove.

Fig. 5
A poor temporary restoration is the same as leaving a tooth open.

Fig. 6
Cuspal reduction is mandatory in case of cracks, and it is the first step. The risk of crack creation and/or propagation between two appointments is very high. In general, all endodontically treated teeth require an indirect restoration or a crown: for this reason, having a flat surface as a reference point may make it easier to young colleagues to measure the working length, when compared to cuspidate teeth.

Fig. 7
Pulp chamber cleaning. It sometimes happens that, when I restore teeth treated by a colleague, I find a dirty pulp chamber. My only thought about these situations is: WHY?

Fig. 8
Pulp chamber walls have to be cleaned by instruments, air abrasion or burs. The prosthodontist or the following colleague has to work in a clean space. It's necessary to pass a simple silicone tip to renew the surface. The tooth is then ready for adhesion procedures. About post placement, please follow the endodontist’s instructions.

Fig. 9
It's advisable to prepare the post space after Root Canal Treatment; in this manner, prosthodontists only have to try the post and, only if necessary, renew the dentin and start with adhesive procedures.

Fig. 10
In this case, my advice was to place only one post. After the appointment with the prosthodontist, the patient came back because of pain. I noticed a perforation in the MB2 canal, due to incorrect post space preparation. I treated this perforation with MTA and the pain was resolved in one week.

Fig. 11
Cotton Pellets and temporary materials. About 90% of my cases end with a definitive restoration that allows the colleagues that will follow to prepare the tooth for a composite restoration or a prosthetic crown. In the other 10% of the cases, I only use cured materials that are able to perfectly adapt to margins thus preventing plaque from entering the prepared space.

Fig. 12
Outer sealing of the endodontic space. The most common mistake at the end of the endodontic treatment, even if a second session scheduled, is the lack of sealing of your own work.

Fig. 13
Temporary margin adaptation. The same concept is to be taken into consideration for the restorative phase: overlapping and invasion of the operative space by the gingiva and rough surface adaptation with the temporary restoration create an ideal hollow for bacterial growth.

Fig. 14
Together with a cured temporary sealing, I prefer teflon as a temporary filling, as it is easier than cottons pallets to completely remove before adhesive procedures.

Fig. 15
Even if you’re not an endodontist, as a dentist you have to know the basic rules for treating a patient with pain, by respecting the endodontic space and correctly (from an endodontic perspective, obviously) opening the pulp chamber and by not laving the tooth with a poor restoration.

Fig. 16
If you, in fact, are an Endodontist, you have to know which the next clinical step will be. In this case the tooth was prepared for a crown the day after, so there was non sense in creating an accurate occlusal anatomy during restoration, nor a correct contact point with the neighboring teeth. After the endodontic treatment, only 15 minutes were needed to restore the tooth properly for prosthodontics.
Conclusions
Dentists sometimes work hard but forget the basic rules to decrease the operative time, for themselves and for the other colleagues. In the next article we will describe, step by step, the clinical procedures to increase success in these steps of the treatment.
Bibliography
Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J 1995;28: 128.
Iqbal MK, Johansson AA, Akeel RF, et al. A retrospective analysis of factors associated with the periapical status of restored, endodontically treated teeth. Int J Prosthodont 2003;16:318.
Saunders WP,Saunders EM.Coronal leakage as a cause of failure in root canal therapy: a review. Endod Dent Traumatol 1994;10:1058.
Alves J, Walton R, Drake D. Coronal leakage: endotoxin penetration from mixed bacterial communities through obturated, post-prepared root canals. J Endod 1998;24: 58791.
Torabinejad M, Ung B, Kettering J. In vitro bacterial penetration of coronally unsealed endodontically treated teeth. J Endod 1990;16:5669.
Chuang SF, Jin YT, Lin TS, et al. Effects of lining materials on microleakage and internal voids of class II resin-based composite restorations. Am J Dent 2003;16: 8490.