
Favourable outcomes of a massive peri-apical lesion with the use of bioceramics
28/08/2024
Ahmed Alwaidh
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Healing of big periapical lesion is a real challenge. But with the use of contemporary devices, techniques, tools and materials, have increased the outcomes of such situations

Fig. 1
A 26 years old female presented complaining of discomfort in her right lower wisdom tooth especially during eating, and a fistula that annoys her. History of amalgam restoration a year ago, then she experienced a severe pain a month later, which subsided few days later after the use of antibiotics and pain killers that been prescribed by her treating dentist. Few months later, a fistula developed next to her lower right wisdom tooth, with pus discharge from time to time.
Clinically, LR8 with amalgam restoration, LR7 and LR6 with composite restorations, with fistula buccal to LR8. LR6 responded normally to cold test, unlike LR7 & LR8.

Fig. 2
IOPA revealed large PA lesion around the roots of LR8, and smaller PA lesion around the roots of LR7.
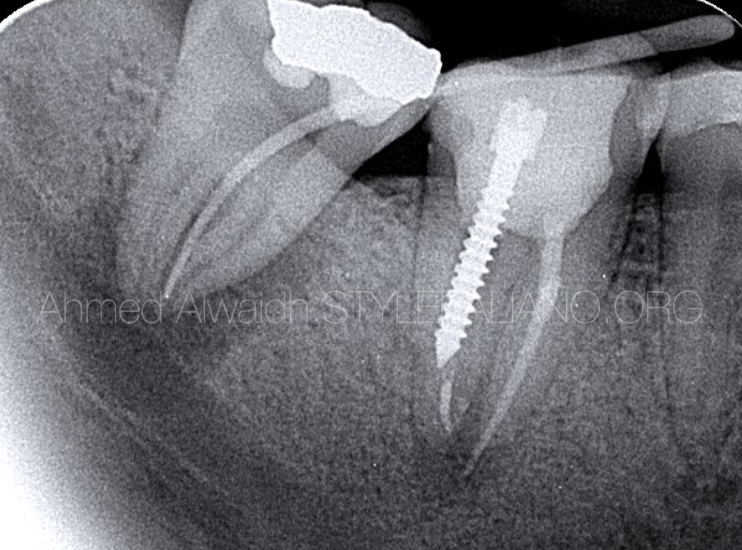
Fig. 3
To know exactly what is the source of the fistula, a GP cone been inserted in to the fistula, and been traced to the apices of LR8 roots.
CBCT images revealed the actual size of the lesion around LR8, which was very big.
Diagnosis: LR8 with necrotic pulp and chronic apical abscess.
Treatment options:
1- Extraction of LR8.
2- Root canal treatment for LR8.
After discussing the treatment options with patient and pros and cons of each option, considering occlusion and outcomes, it has been decided to go with root canal treatment option.

Fig. 4
After IDN block anaesthesia and isolation with rubber dam, access opening been made for LR8 to reveal a necrotic pulp. Only two canals, both prepared to full working length with #25/06. NaOCl 5.25%, US activation (PUI), and the canals been dressed with non-setting calcium hydroxide, and LR8 been temporised.

Fig. 5
Next visit was a month later, absence of symptoms and the fistula.
Irrigation with NaOCl 3%, EDTA 17%, PUI.
Hydraulic obturation with pre-mixed bioceramic cement. LR8 been restored with composite and been made out of occlusion.
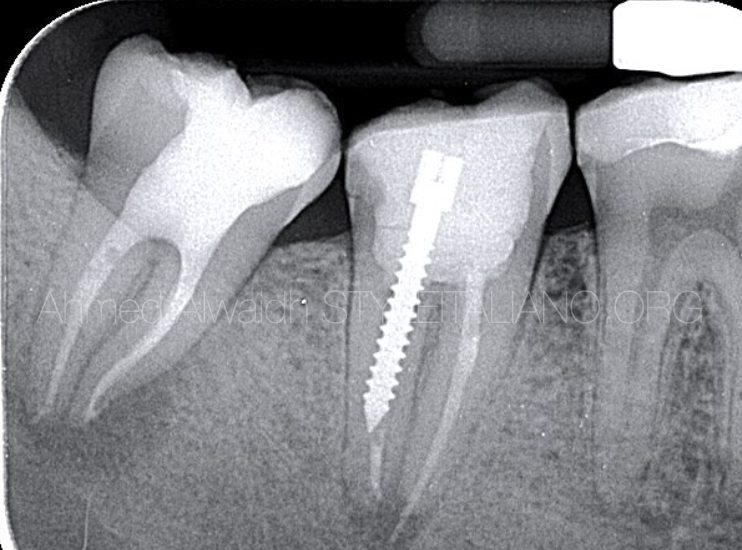
Fig. 6
Immediate post operative IOPA radiograph.
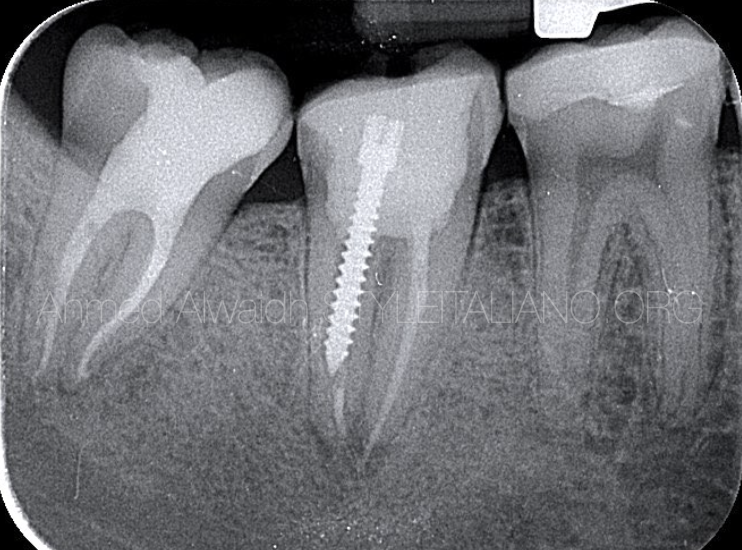
Fig. 7
Six months follow up IOPA revealed complete absence of PA lesion around the roots of LR8 with evident bone trabeculae formation.
Conclusions
Although root canal treatment of lower wisdom teeth are challenging due to many factors like complex anatomy, difficulty to access, and neighbouring inferior dental nerve to the apices, and this is the reason why many prefer extraction of lower wisdom teeth over root canal treatment. However, if the lower wisdom tooth is restorable, well aligned and oriented, in good occlusion with upper wisdom tooth, then root canal treatment is an important option.
Success rate of root canal treatment without a periapical lesion has much better outcomes than teeth with existing periapical lesion (Strindberg 1956, Seltzer and Bender 1963, Sjögren et al. 1990).
In this case, Although LR8 has a very big lesion with majority of bone around it been destructed, but it was well oriented, restorable, and in Avery good occlusal relationship with opposing UR8. And the patient was eager for root canal treatment over extraction.
Although contemporary root canal treatments using advanced techniques, instruments, and materials have increased the outcomes of root canal treatment, but for such a big lesion to be completely healed within a six months is interesting. This is most probably due to the use of premixed calcium silicate cement as an obturation material, which possess many advantages when compared to other types of sealers like high antibacterial activity due to its high pH (>11), in addition to its high tendency to release calcium ions (Candeiro et al. 2012, Wang et al. 2014, Candeiro et al. 2016, Lee et al. 2017, Bukhari & Karabucak 2019), they are highly hydrophilic, and the moisture in the dentinal tubules not only does not affect the sealer, but also promotes setting, decreases setting time, allowing the sealer to expand slightly during the process (Hench 1991, Richardson 2008, Gandolfi et al. 2009, Koch & Brave 2009, Zhang et al. 2009b, Nekoofar et al. 2010, Zhang et al. 2010a, Loushine et al. 2011, Jefferies 2014a, Jefferies 2014b).
Premixed bioceramic cement also have superior biocompatibility and bioactivity that induce bone regeneration due to calcium phosphate that exists in these sealers, which is also the main inorganic component of the hard tissues (Bae et al. 2010, Bryan et al. 2010, Cheng et al. 2010).
Bibliography
- Bae WJ, Chang SW, Lee SI et al. (2010) Human periodontal ligament cell response to a newly developed calcium phosphate–based root canal sealer. Journal of Endodontics 36(10), 1658-1663.
- Bryan TE, Khechen K, Brackett MG et al. (2010) In vitro osteogenic potential of an experimental calcium silicate–based root canal sealer. Journal of Endodontics 36(7), 1163-1169.
- Bukhari S., Karabucak B. (2019) The Antimicrobial Effect of Bioceramic Sealer on an 8-week Matured Enterococcus faecalis Biofilm Attached to Root Canal Dentinal Surface. Journal of Endodontics 45(8), 1047-1052.
- Candeiro GTDM, Correia FC, Duarte MAH, Ribeiro-Siqueira DC, Gavini G (2012) Evaluation of radiopacity, pH, release of calcium ions, and flow of a bioceramic root canal sealer. Journal of Endodontics 38(6), 842-845.
- Candeiro, GTDM, Moura‐Netto CD, D'Almeida‐Couto RS et al. (2016) Cytotoxicity, genotoxicity and antibacterial effectiveness of a bioceramic endodontic sealer. International Endodontic Journal 49(9), 858-864.
- Cheng L, Ye F, Yang R et al. (2010) Osteoinduction of hydroxyapatite/β-tricalcium phosphate bioceramics in mice with a fractured fibula. Acta Biomaterialia 6(4), 1569- 1574.
- Gandolfi MG, Iacono F, Agee K et al. (2009) Setting time and expansion in different soaking media of experimental accelerated calcium-silicate cements and ProRoot MTA. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 108, e39–45.
- Hench LL (1991) Bioceramics: from concept to clinic. Journal of the American Ceramic Society 74(7), 1487-1510.
- Koch K, Brave D (2009) Bioceramic technology—the game changer in endodontics. Endodontic Practice 12, 7–11.
- Jefferies SR (2014a) Bioactive and biomimetic restorative materials: a comprehensive review. Part I. Journal of Esthetic and Restorative Dentistry 26(1), 14-26.
- Jefferies SR (2014b) Bioactive and biomimetic restorative materials: a comprehensive review. Part II. Journal of Esthetic and Restorative Dentistry 26, 27–39.
- Lee JK, Kwak SW, Ha JH, Lee W, Kim HC (2017) Physicochemical properties of epoxy resin-based and bioceramic-based root canal sealers. Bioinorganic Chemistry and Applications, 2017.
- Loushine BA, Bryan TE, Looney SW et al. (2011) Setting properties and cytotoxicity evaluation of a premixed bioceramic root canal sealer. Journal of Endodontics 37, 673–677.
- Nekoofar MH, Stone DF, Dummer PMH (2010) The effect of blood contamination on the compressive strength and surface microstructure of mineral trioxide aggregate. International Endodontic Journal 43(9), 782-791.
- Richardson IG (2008) The calcium silicate hydrates. Cement and Concrete Research 38(2), 137-158.
- Seltzer S, Bender IB, Zionitz M. The interrelationship of pulp an periodontal disease. Oral Surg Oral Med Oral Pathol 1963: 16: 1474–1490.
- Sjo¨gren U, Hagglund B, Sundqvis G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod 1990: 16: 498–504.
- Strindberg LZ. The dependence of the results of pulp therapy on certain factors. An analytic study based on radiographic and clinical follow-up examinations. Acta Odont Scand 1956: 14: 1177–1180.
- Wang Z, Shen Y, Haapasalo M (2014) Dentin extends the antibacterial effect of endodontic sealers against Enterococcus faecalis biofilms. Journal of Endodontics 40(4), 505-508.
- Zhang W, Li Z, Peng B (2010b) Effects of iRoot SP on mineralization-related genes expression in MG63 cells. Journal of Endodontics 36(12), 1978-1982.
- Zhang W, Li Z, Peng B (2010a) Ex vivo cytotoxicity of a new calcium silicate-based canal filling material. International Endodontic Journal 43, 769–774.




