Does MTA ensure a good seal?
07/12/2023
Ahmed Alwaidh
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Large apices and root canal perforations are always challenging to seal with traditional root filling materials, for many reasons like shrinkage, toxicity, inflammatory response, and sealing ability of those materials.
Since it was first introduced (Torabinejad et al. 1995), MTA (Mineral Trioxide Aggregate) been widely used in many clinical applications in Endodontics. In this article, I will discuss the sealing ability of MTA in three clinical cases.

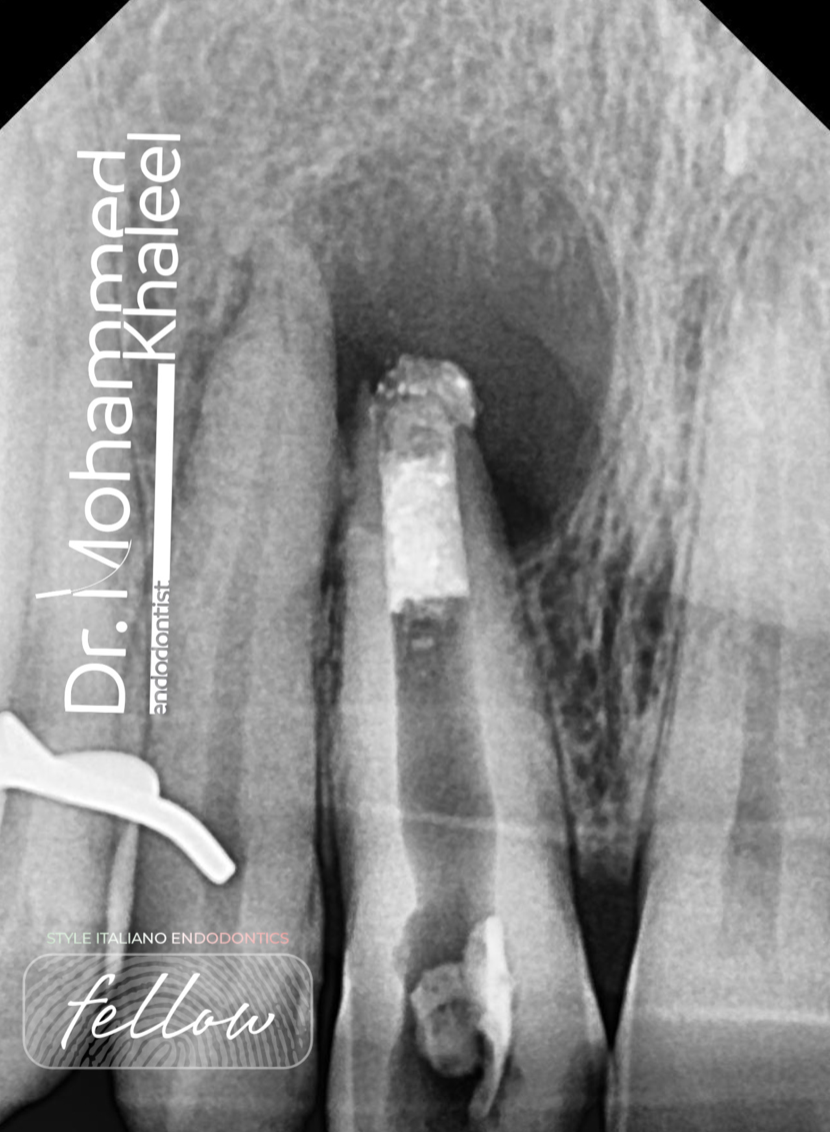
Fig. 1
A 42 years old female presented complaining of a severe spontaneous pain. History of restoration in LR7 and implant in LR6 two years ago. Clinically, LR7 had a defective restoration with severe lingering painful response to cold test, while LR6 implant was normal with no mobility, pocketing, nor tenderness.
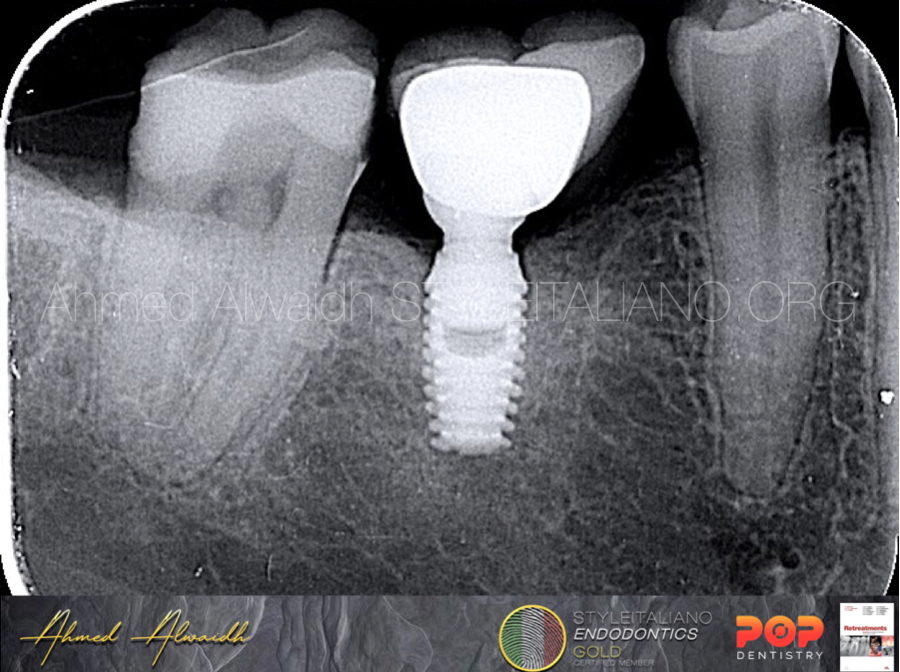
Fig. 2
IOPA revealed calcified pulp chamber in LR7.

Fig. 3
After access to LR7 and removing the inflamed pulp chamber tissue, pulp stone been removed using ultrasonic tips.
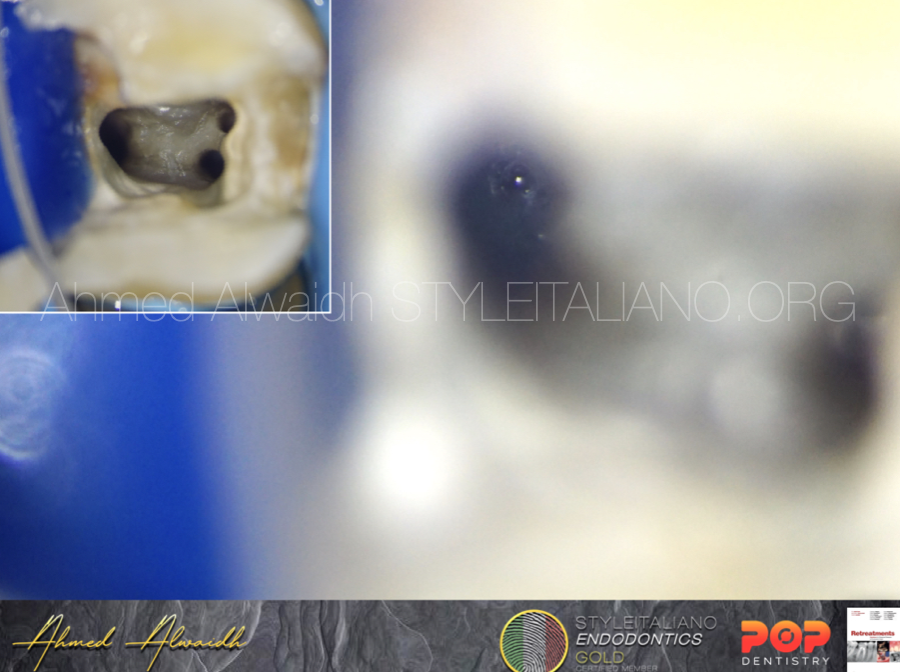
Fig. 4
After finishing the chemo-mechanical preparation of LR7 and the tooth was ready for obturation, D canal was very wide making obturation of D canal with thermal gutta percha questionable, due to shrinkage of gutta percha.
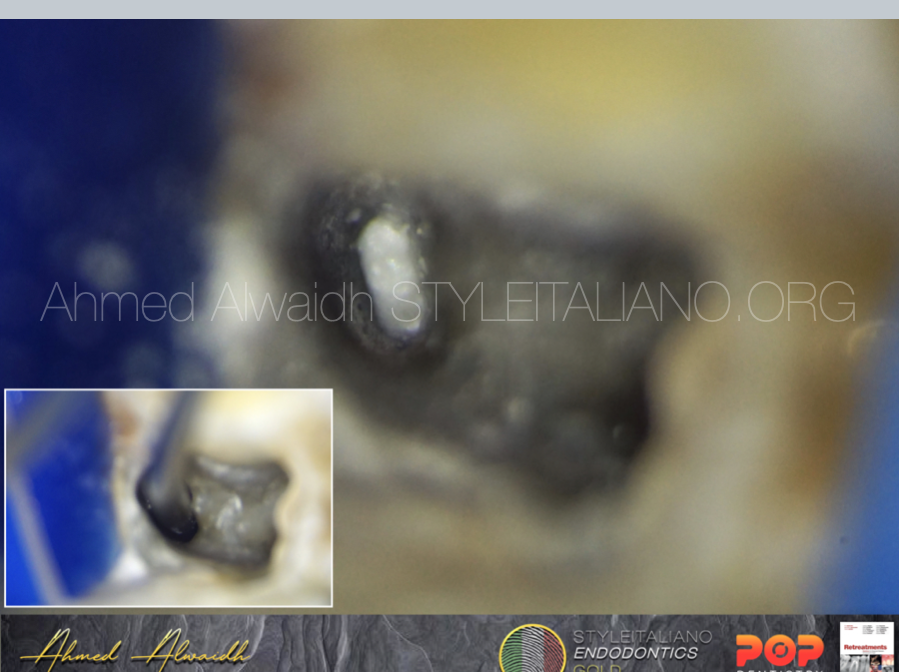
Fig. 5
D canal of LR7 been obturated with MTA apical plug, then the rest of the D canal been obturated with thermoplasticised GP. While M canals been obturated with Continuous Wave of Condensation (CWC) and calcium hydroxide-based sealer.
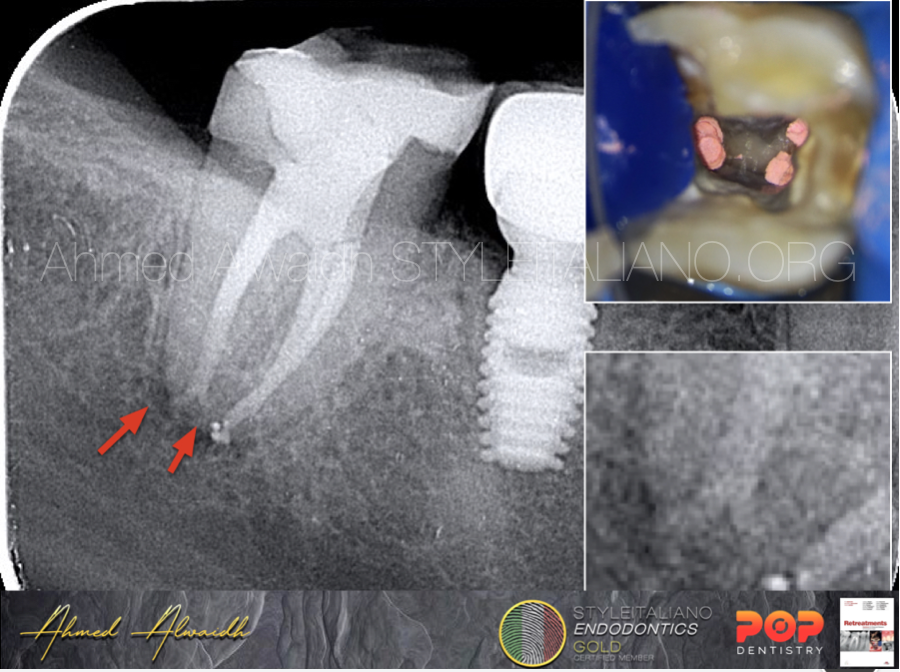
Fig. 6
Post operative radiograph shows clearly how MTA penetrated and filled lateral canal in the D root of LR7.
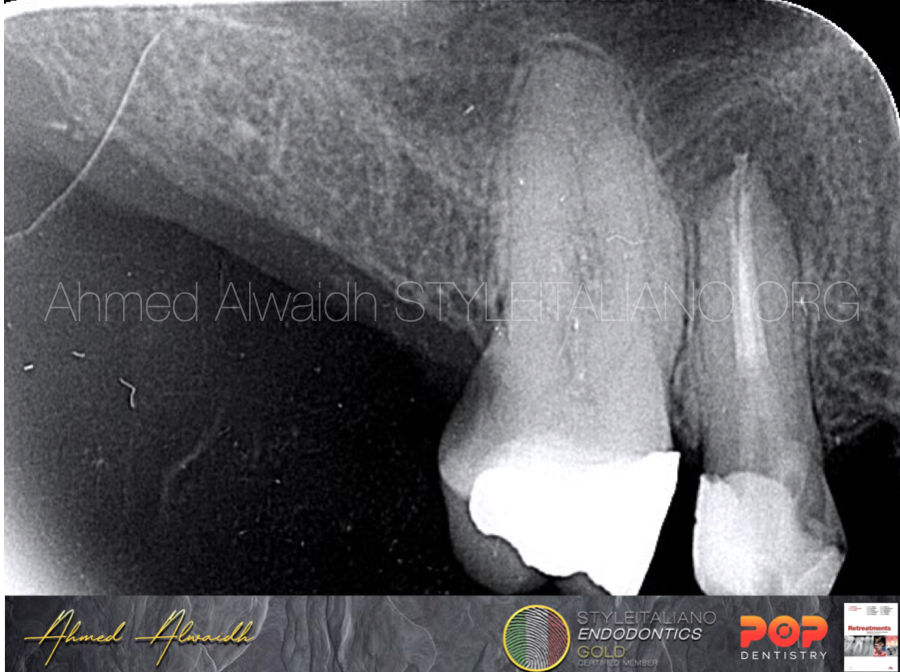
Fig. 7
UR6 been diagnosed with symptomatic irreversible pulpitis (SIP) and normal apical tissue

Fig. 8
After chemo-mechanical preparation, P canal was very wide.

Fig. 9
It has been decided to obturate P canal with MTA apical plug, to overcome the shrinkage of thermoplasticised gutta percha.
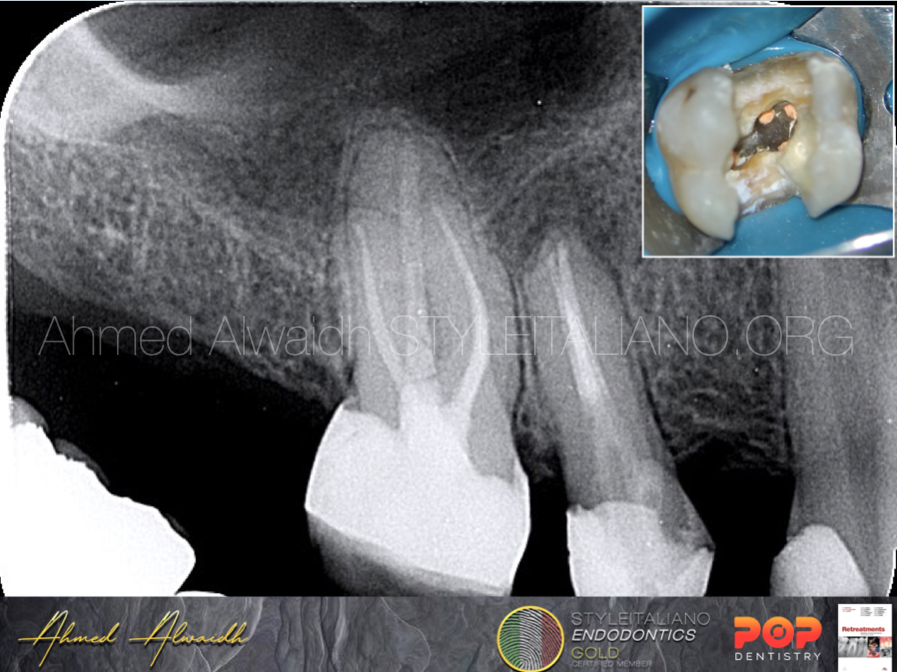
Fig. 10
The rest of the P canal then been filled with thermoplasticised gutta percha, and other canals with hydraulic obturation by premixed Bioceramic cement.

Fig. 11
Three years follow up, UR6 was functional and asymptomatic, with no resorption in the MTA plug now periapical changes
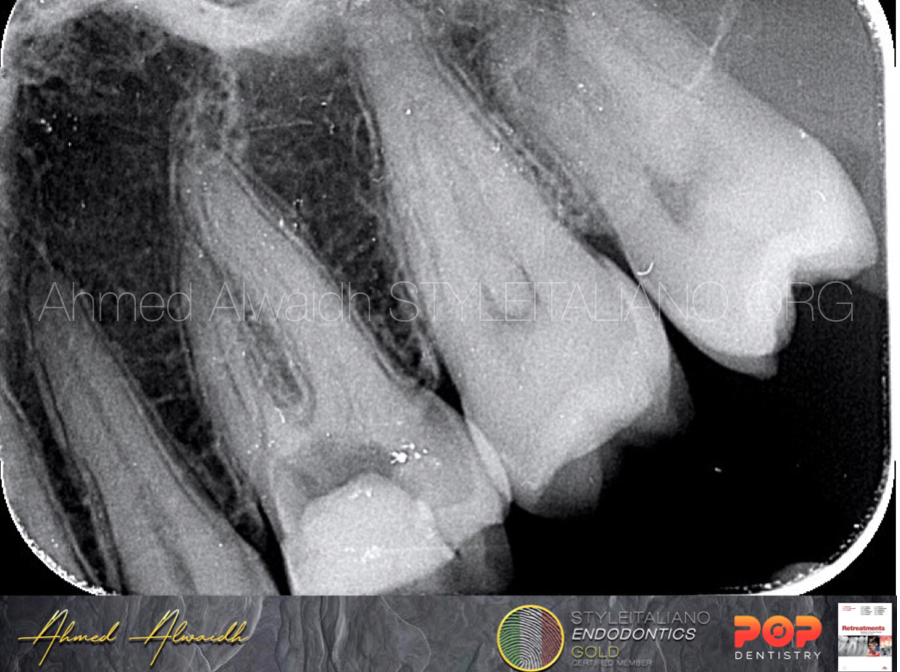
Fig. 12
A 31 years old male been referred by a colleague to do RCT for UL6, as he couldn’t locate the canals. Patient was complaining of a severe pain started a night before.
IOPA revealed clearly a calcified pulp chamber of UL6.

Fig. 13
After removing the pulp stone with ultrasonic tips, there was a piece of the pulp stone in the furcation area, which was mobile and leaking blood from underneath (the inflammatory response led to the invasion of the furcation area). This piece had to be removed and the site should be sealed after.

Fig. 14
After removing the mobile stone piece from furcation area, the site underneath been disinfected and the bleeding was seized with NaOCl 1.5% for 5 minutes.

Fig. 15
A piece of gelatine hemostatic absorbable sponge been placed at the perforation site; to act as a platform so we can pack the MTA on, and to act as a hemostatic until the MTA is fully set (which takes 48-72 hours).
Fig. 16
MTA then been packed on the absorbable sponge.

Fig. 17
A layer of GIC (glass ionomer cement) been applied over the MTA, so the irrigation solutions don’t affect the MTA, as it was on primary set only.
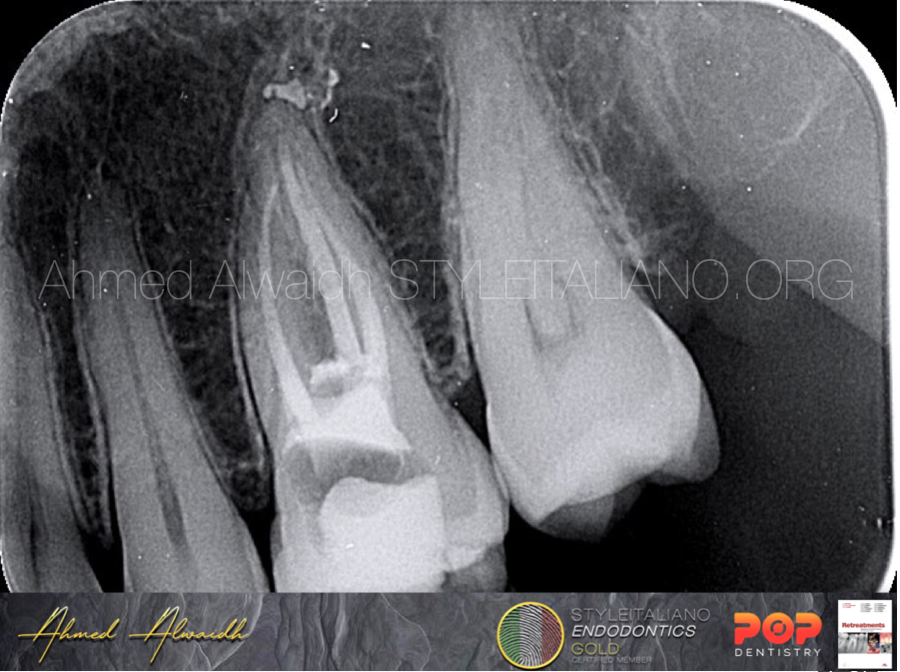
Fig. 18
Immediate post operative IOPA of UL6.

Fig. 19
6 years recall, although the patient didn’t put full crown, but UL6 was functional, asymptomatic, and the MTA as there with no radiographic changes.
Conclusions
MTA has superior properties compared to other materials like biocompatibility, high antibacterial activity, sealing ability, promoting regeneration of bone tissue, hydrophilic material, and expansion during setting, make it as a good material of choice to seal large apices and perforations, especially when it comes to direct contact with vital tissues. Many papers have tested the sealing ability of MTA (Torabinejad & Chivian 1999, Pereira et al. 2004, Yildirim et al. 2009, Hirschberg et al. 2013, Agrafioti et al. 2016), and they have found that MTA it is one of the best materials to be used, due to its high sealing ability, among other properties mentioned above.
Bibliography
- Agrafioti A, Tzimpoulas N, Chatzitheodoridis E, Kontakiotis E G (2016) Comparative evaluation of sealing ability and microstructure of MTA and Biodentine after exposure to different environments. Clinical oral investigations 20, 1535-1540.
- Hirschberg C S, Patel N S, Patel L M, Kadouri D E, Hartwell G R (2013) Comparison of sealing ability of MTA and EndoSequence Bioceramic Root Repair Material: a bacterial leakage study. Quintessence international 44(5).
- Pereira C L, Cenci M S, Demarco F F (2004) Sealing ability of MTA, Super EBA, Vitremer and amalgam as root-end filling materials. Brazilian oral research 18, 317-321.
- Torabinejad M, Hong C U, McDonald F, Ford T P (1995) Physical and chemical properties of a new root-end filling material. Journal of endodontics 21(7), 349-353.
- Torabinejad M, Chivian N (1999) Clinical applications of mineral trioxide aggregate. Journal of endodontics 25(3), 197-205.
- Yildirim T, Taşdemir T, Orucoglu H (2009) The evaluation of the influence of using MTA in teeth with post indication on the apical sealing ability. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 108(3), 471-474.