Bubble Free Access Sealing
17/03/2017
Calogero Bugea
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Several studies have highlighted how crucial an effective coronal restoration is to the success of the endodontic treatment.

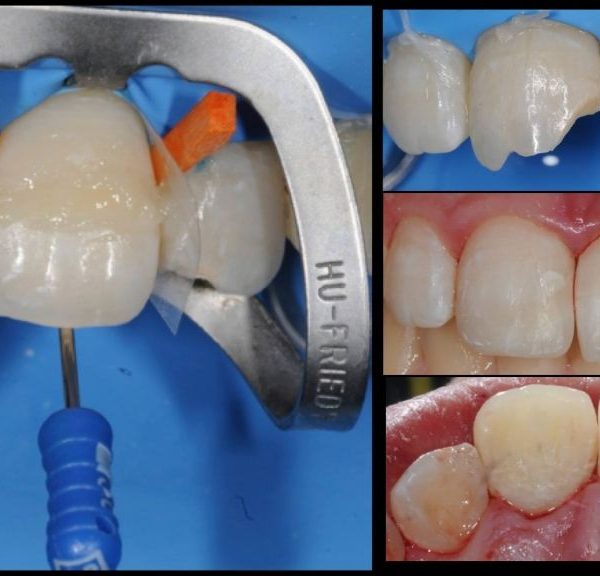
Fig. 1
For this reason, the prognosis of endodontic therapy could be heavily influenced by contamination of the root canal system through marginal or internal gaps of the coronal restoration. Therefore, an effective coronal seal constitutes a fundamental aspect long-term success of the endodontic therapy. Although adhesive procedures have shown – both in vitro and in clinical practice – very high performance, gap formation and marginal microleakage caused by adhesive bond failure are still the most reported issues; these are potentially caused by several factors, including composite shrinkage stress, mechanical properties of restorative materials, C factor, and the composite layering technique. Clinicians prefer to use a flowable composite at the bottom of the pulp chamber after canal filling, it ensures better marginal integrity and improves the fit between adhesive systems and composite materials, creating fewer voids and decreasing microleakage.

Fig. 2
In this article will be described a technique to minimize gap between flowable layer and pulp chamber floor, with the help of the LM Fissura instrument, powered by Style Italiano (Smileline Switzerland).

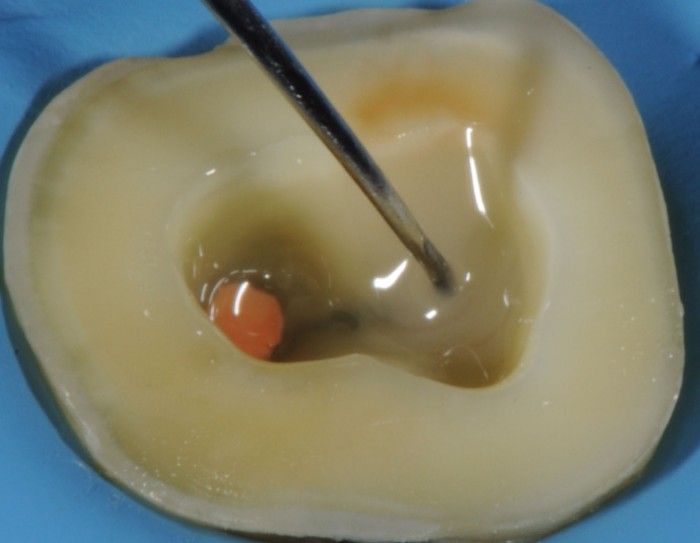
Fig. 3
After ending the endodontic procedure, it’s advisable to have a regular and flat floor because it is easier to fill a flat floor without voids than an irregular floor. img left show an irregular floor due to the excess of guttapercha Img right show the same floor, regularized. In this manner it's possible reduce the amount of voids.

Fig. 4
Some kind of adhesive agents are very viscous and tend to create a thick layer and sometimes bubbles: for this reason it is necessary to reduce the thickness in order to minimize the amount of bonding agent at the bottom of the restoration.

Fig. 5
The first step is to introduce an amount of flowable composite in a corner of the prepared chamber: this is my favorite spot to inject the flowable material because it eases the flowing of the composite from an almost-external position; gravity leads the process and with the Fissura instrument it is very easy to get the material in all the nooks of tha chamber floor.

Fig. 6
Sometimes it’s possible to see some air bubbles emerging from the composite; this accident is not to be considered important, as during the following step we can eliminate this voids.

Fig. 7
With a gentle, circular movement with the Fissura instrument we can adapt the mass of flowable composite to the cavity.
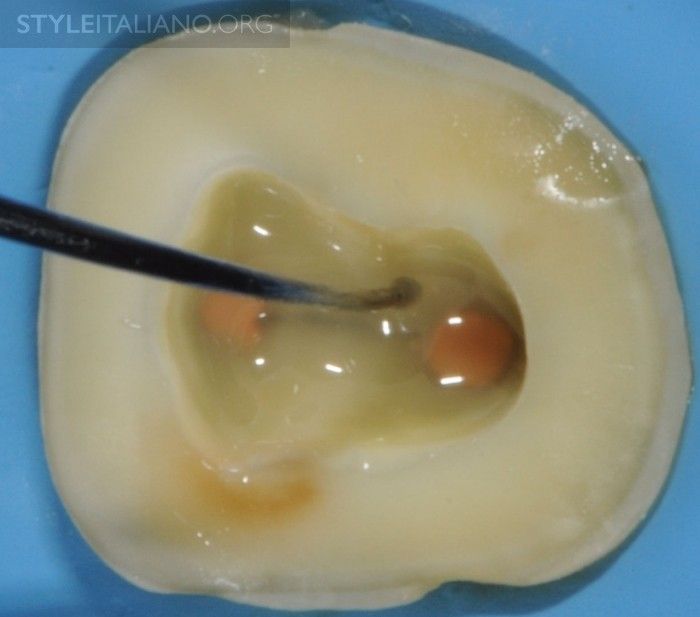
Fig. 8
Alternating a linear movement to the circular one ensures the exploration of the whole mass.

Fig. 9
The objective of this step is to create a uniform and flat plane, on which we can safely build up the rest of our restoration.

Fig. 10
Thanks to the solid base we have obtained with this manoeuvre we can now restore directly the tooth, build up, or introduce a temporary filling material.
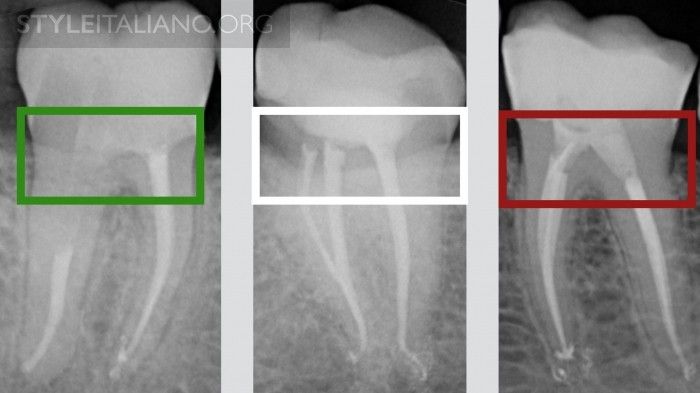
Fig. 11
Post operative Rx: left image shows a perfect adaptation of the material on the floor of the pulp chamber using the technique described in this article; the Rx in the middle shows the presence of small bubbles in the correspondence of mesial canals; the image on the right shows the presence of a gap.
Conclusions
Previous studies have reported a significant reduction in shrinkage stress through the interposition of an intermediate layer of flowable composite because of its superior internal flow and adaptation, which partially compensates for shrinkage stress, creating an elastic layer between the substrate and the restorative material.
The absence of interfacial gaps between the restoration and root canal filling materials is essential and directly determines the long-term success of endodontic therapy
Furthermore, the gap at the interface between the restorative material and dental tissue, or within the restorative material itself, increases the probability of the formation and propagation of cracks.
Bibliography
Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J 1995;28: 128.
Iqbal MK, Johansson AA, Akeel RF, et al. A retrospective analysis of factors associated with the periapical status of restored, endodontically treated teeth. Int J Prosthodont 2003;16:318.
Saunders WP,Saunders EM.Coronal leakage as a cause of failure in root canal therapy: a review. Endod Dent Traumatol 1994;10:1058.
Alves J,Walton R,Drake D. Coronalleakage:endotoxin penetration from mixed bacterial communities through obturated, post-prepared root canals. J Endod 1998;24: 58791.
Evaluation of Composite Adaptation to Pulpal Chamber Floor Using Optical Coherence Tomography.
Scotti N, Alovisi C, Comba A, Ventura G, Pasqualini D, Grignolo F, Berutti E. J Endod. 2016 Jan;42(1):160-3.
Drummond JL. Degradation, fatigue and failure of resin dental composite materials. J Dent Res 2008;87:7109.
Torabinejad M, Ung B, Kettering J. In vitro bacterial penetration of coronally unsealed endodontically treated teeth. J Endod 1990;16:5669.
Chuang SF, Jin YT, Lin TS, et al. Effects of lining materials on microleakage and internal voids of class II resin-based composite restorations. Am J Dent 2003;16: 8490.
Haak R, Wicht MJ, Noack MJ. Marginal and internal adaptation of extended class I restorations lined with flowable composites. J Dent 2003;31:2319.
Oliveira LC, Duarte S Jr, Araujo CA, Abrahmao A. Effect of low-elastic modulus liner and base as stress-absorbing layer in composite resin restorations. Dent Mater 2010;26: 5969.