A goal in the hole
21/01/2021
Ahmed Shawky
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The main goal of endodontic treatment is the treatment and/or prevention of peri-radicular periodontitis aiming for a long term disease-free survival. The presence of any form of communication between the pulp space and the periodontist and/or the oral cavity will lead eventually to development or recurrence of peri-radicular disease which will prevent the clinician from reaching success in his/her treated cases.
Iatrogenic perforations during endodontic procedures represent a bacterial pathway between the oral cavity &/or periodontium from one side and the root canal space from the other side. Literature reported a 10-12% decrease in the success rate of endodontic treatments in the presence of iatrogenic perforation.
The most common type of perforations are the floor perforation, which may occur due to;
- Searching for canal orifices with cutting tools
- Lack of anatomical reference in badly decayed, crowned or heavily restored teeth
- Recession of the pulp chamber as a result of pathologic or physiologic process
- Mis-orientation in the mesiodistal or faciolingual plane during post space preparation
The aim of this article is to present a case with chamber floor perforation, its procedural steps for repair and its follow up for 8 months.
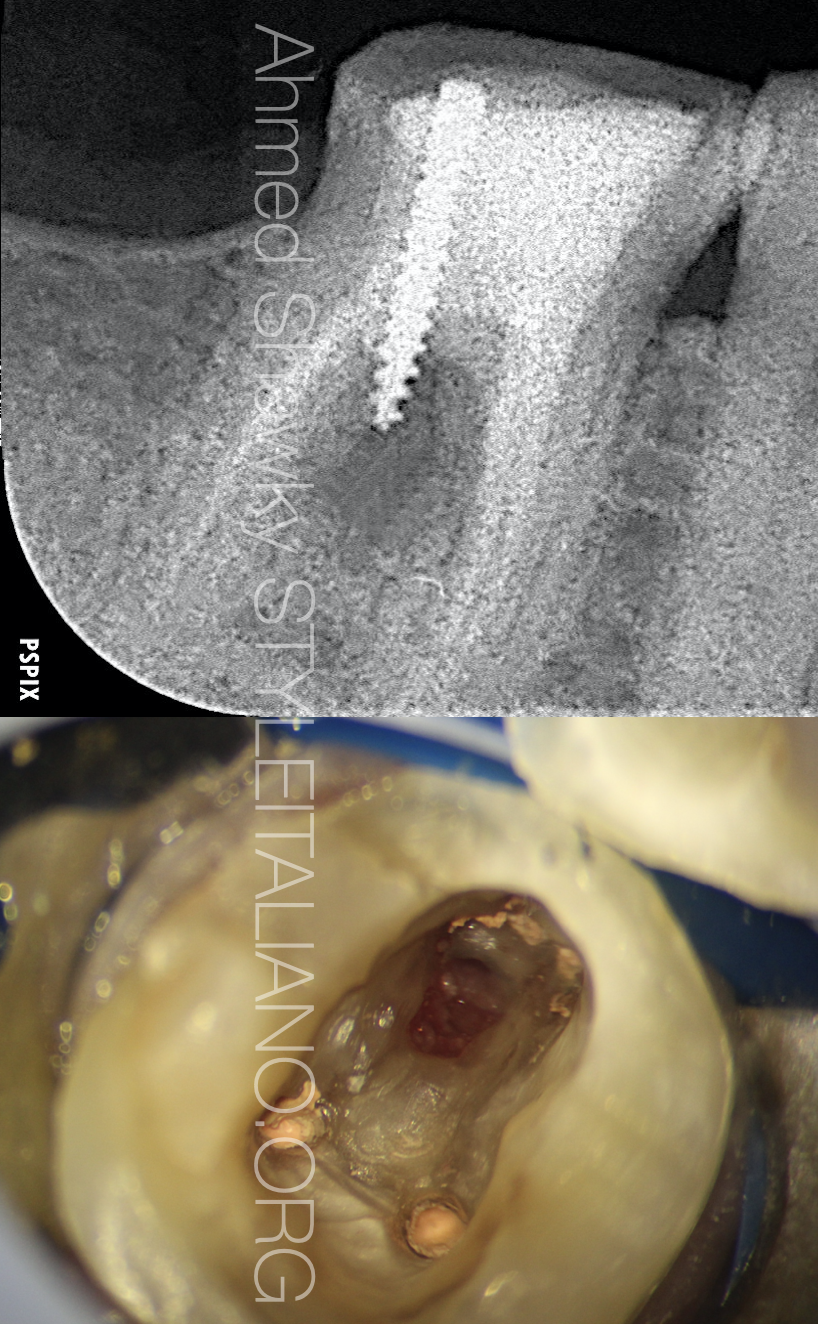
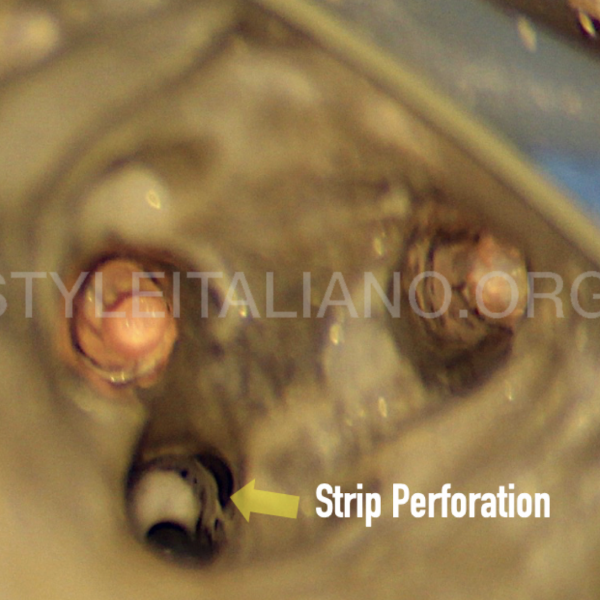
Fig. 1
Pre-operative evaluation
A 35 years old, medically fit female presented complaining of a persistent swelling near the marginal gingiva of her mandibular right first molar after restorative procedures. She reported intermittent discharge through the buccal gingival margin with continuous tenderness to biting on the tooth.
Clinical examination revealed a restored mandibular first molar with moderate severe tenderness to gentle vertical and lateral percussion.
The buccal gingival tissues was swollen, easily retracted and upon digital pressure showed some bloody discharge.
Periodontal probing depths were examined. The probing depth was normal all around the tooth. Probing of the furcation area buccally revealed a 9 mm probing defect.
Radiographic examination revealed a previously treated molar with a screw post perforating the chamber floor. The furcation region displayed a large inter-radicular lesion.
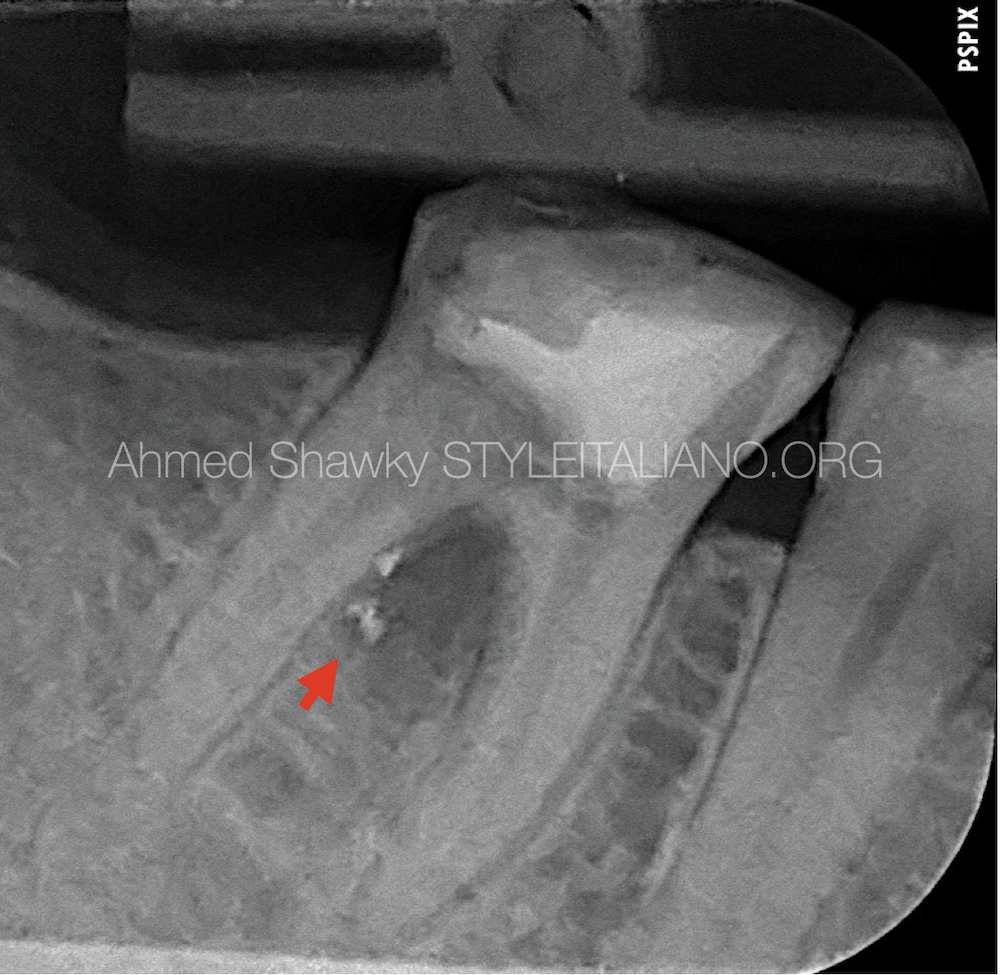
Fig. 2
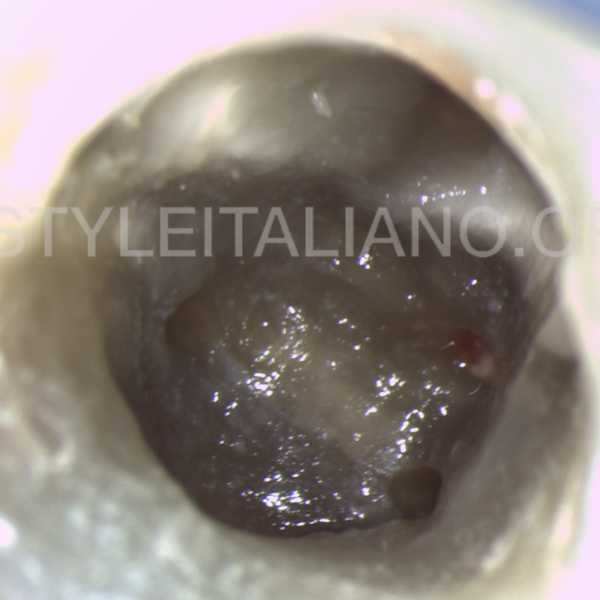
Regaining access to the pulp chamber
Disassembly of the coronal restoration was performed under rubber dam isolation and microscopic magnification using high speed diamond burs till reaching the area near to the post head.
The material around the post head was removed using a mid-power ultrasonic instrument to avoid extensive damage to the post head.
Counterclockwise application of ultrasonics facilitated unscrewing the post. However, some metal fragments were separated from the post (red arrow) and remained in the already inflamed inter-radicular tissues.
Removal of the root canal filling was done due to compromised sealing and the presence of apical periodontitis
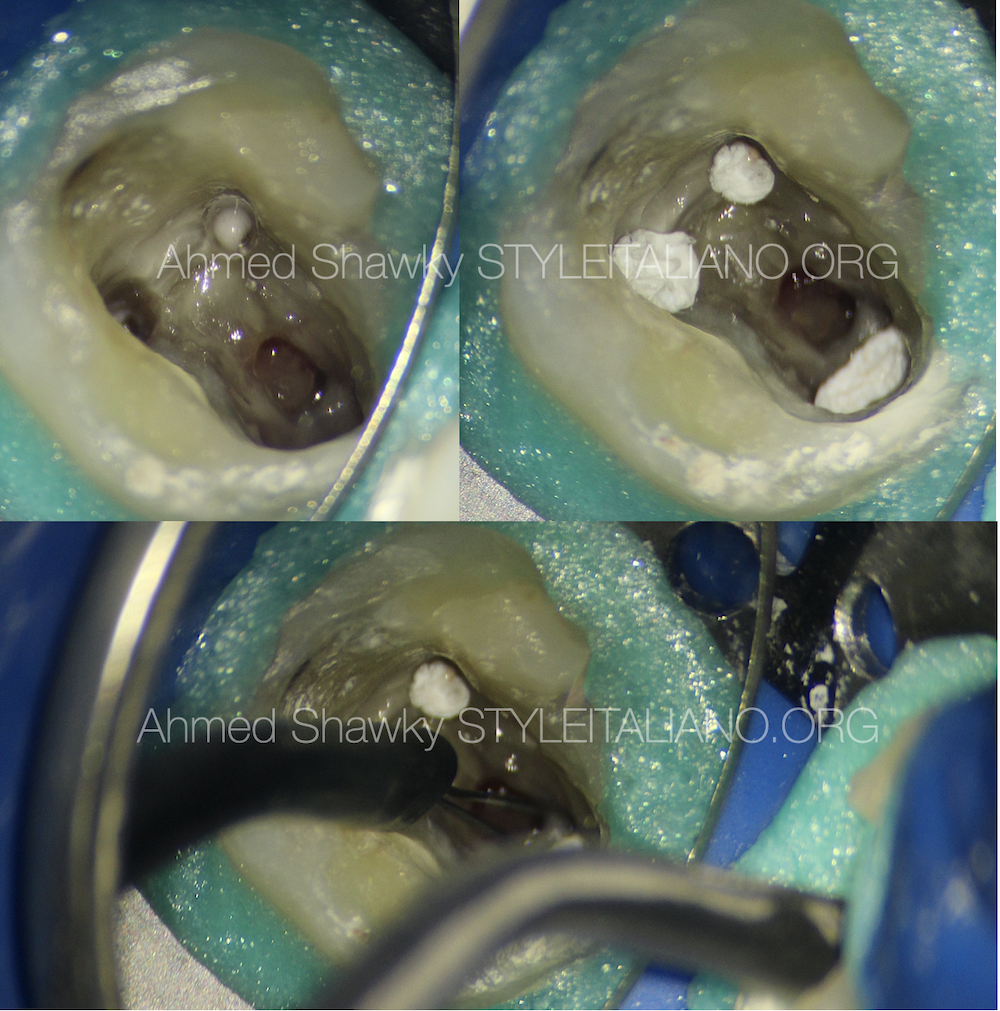
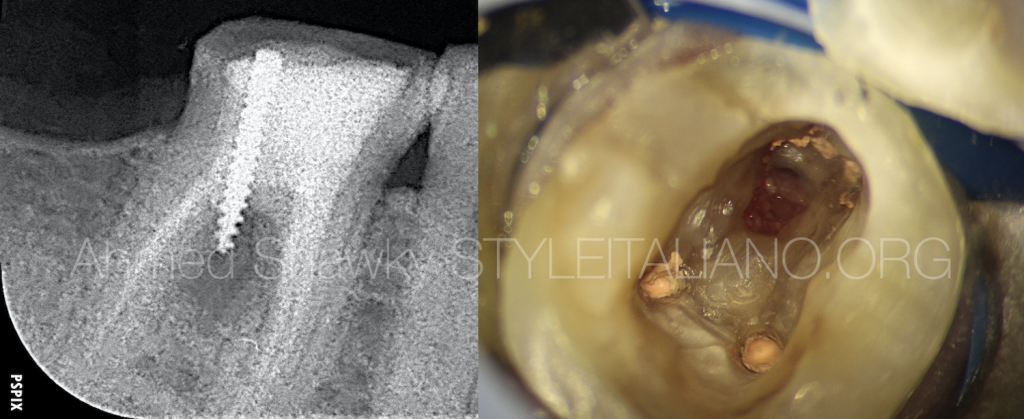
Fig. 3
Removal of the inter-radicular metal fragments
Removal of the metal fragments was impossible before removal of the inflammatory tissues projecting into the floor perforation.
The cleaned and shaped root canals were protected using sterile teflon tape packed at the orifice. A cut and coagulate mode in an electrosurgery unit was used to remove the tissues and at the same time control bleeding without any damage to the bone of the roots.
Visual access to the metal fragments was achieved using high magnification and coaxial illumination. A microsurgical tip was used to suck out the fragments. The inter-inter-radicular region was then flushed with 20cc sterile normal saline to prepare the area for repair.
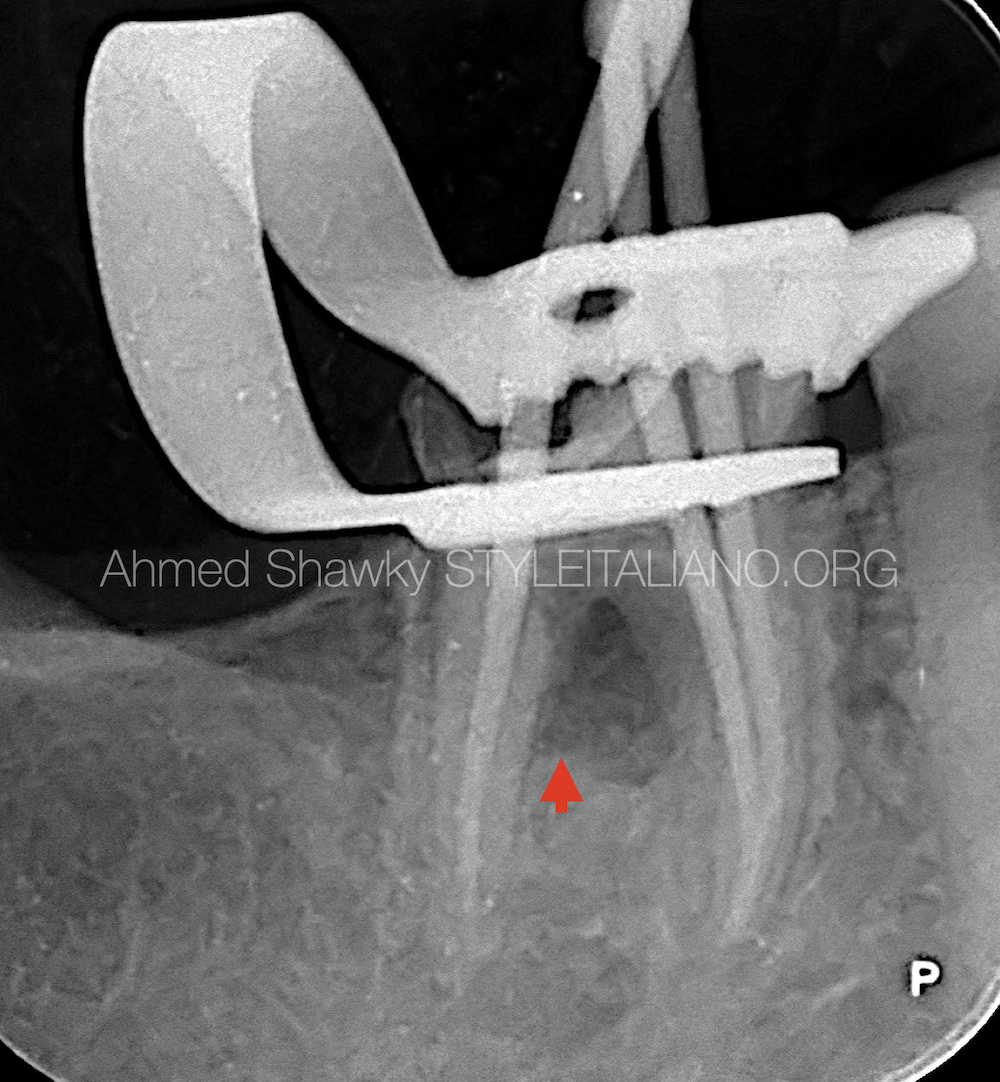
Fig. 4
Radiographic confirmation and cone fitting.
Radiographic confirmation of metal fragments retrieval (Red arrow) was done at the same time with the cones check
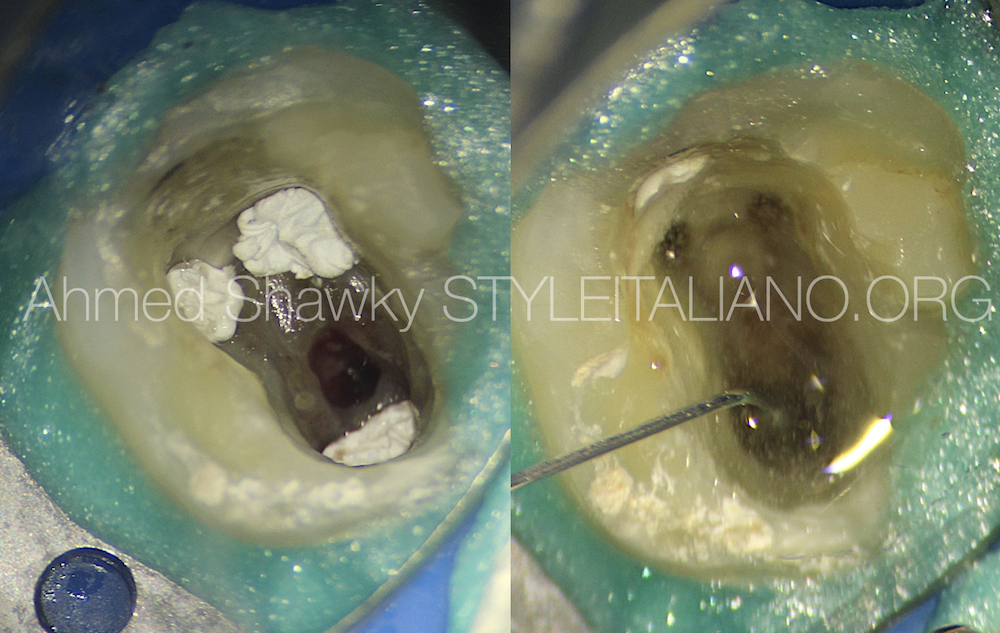
Fig. 5
Preparation of the perforation site
Final decontamination of the pulp chamber and the perforation margins was done using 2.5% NaOCl aided by passive ultrasonic agitation, without any intention to intrude the irrigant into the perforation site to avoid the caustic effect of the irrigant on the peri-radicular tissues.
New sterile teflon pellets were used to seal the canal orifices, preventing accidental lodging of the bioceramic repair material into the root canal space
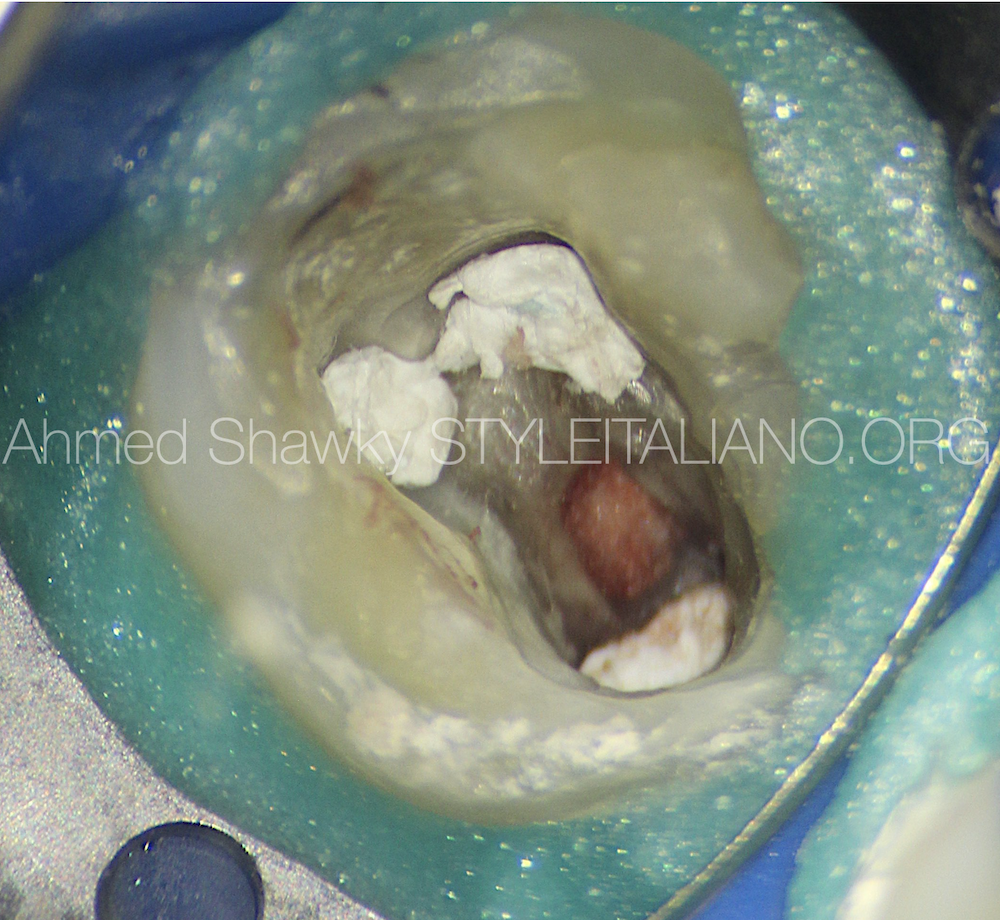
Fig. 6
Placement of a resorbable barrier.
A resorbable collagen matrix was packed into the furcation region through the perforation to act as a barrier against extrusion of the repair material and to limit the repair material to the perforation site.
Another advantage of using the resorbable matrix, is to control bleeding by activation of the clotting cascade.

Fig. 7
Placement of Bioceramic repair material
A fast setting Bioceramic putty material (Avalon Biomed, USA) was delivered to the perforation site using MAP one carrier (Produits Dentaires SA, Vevey, Switzerland) followed by brush packing.
The interface between the chamber floor and the repair material was cleaned from excess material using a Microbrush
A sterile, slightly moist, cotton pellet was placed against the repair material to enhance hydration, accelerate setting and improves the mechanical properties of the set material.
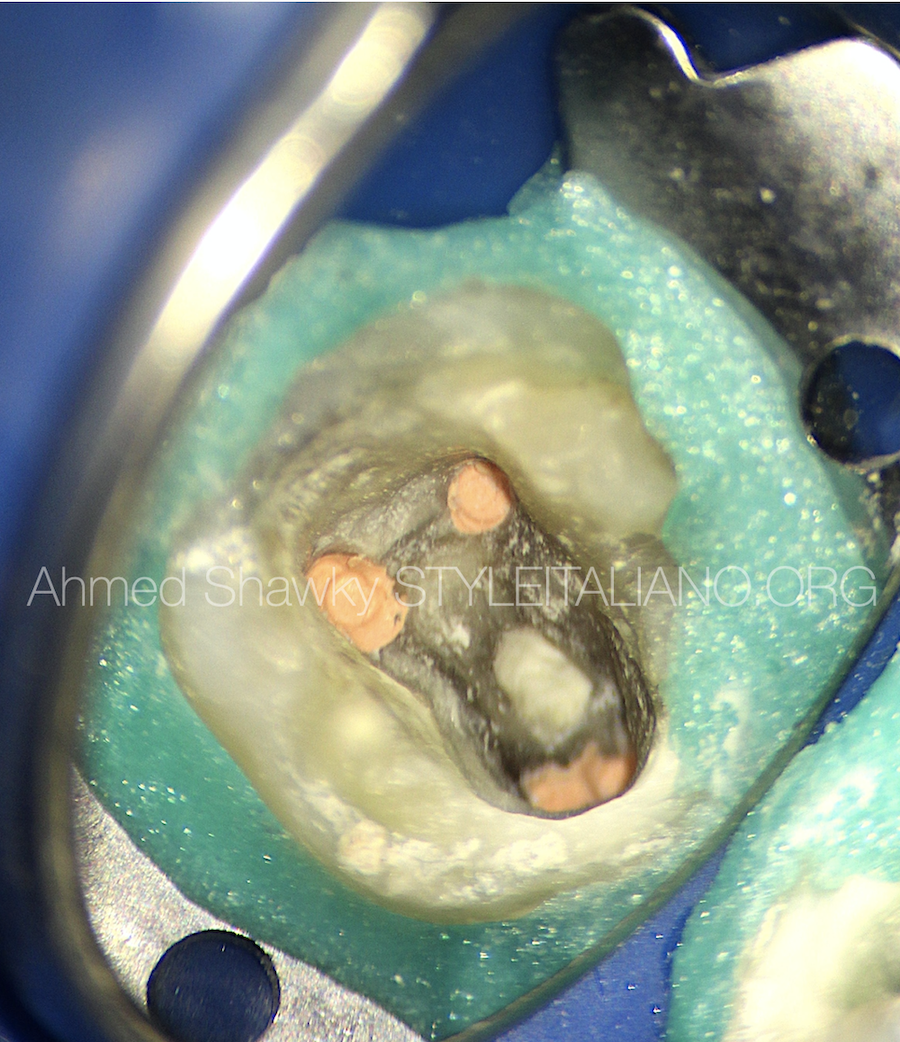
Fig. 8
Obturation of the root canal system
Complete setting of the repair material was confirmed by scratching a DG16 probe against the repaired area.
The root canals were obturated using warm vertical compaction. A coronal seal was placed at the obturation visit
1 week later, the patient attended for coronal coverage. The tooth was restored into normal function and contours using a zirconia crown.

Fig. 9
8 months post-restorative recall:
After 8 months, the patient returned for routine examination. Radiographic evaluation of the treated molar revealed complete healing of the furcal lesion and apical periodontitis.
Clinical examination revealed no tenderness to vertical or lateral percussion. There was no probing defect in the furcation region and the gingival tissues regained their normal texture, color and contour
Conclusions
- The recently optimized formulations of calcium silicates improved the predictability and outcomes of perforation repair in terms of bioactivity, antibacterial activity, sealing ability, mechanical properties as well as optical characteristics (staining potential).
- Using a dedicated carrier for delivery of the repair material to the perforation site will minimize the waste and facilitate accurate placement of the material.
- The obturation phase of the treatment can be done before or after perforation repair, depending on the size of the perforation and the proximity of the perforation to the root canals
- Perfect coronal seal is mandatory to create an environment favorable for healing and a disease-free tooth survival
Bibliography
1-Giovarruscio M, Tonini R, Zavattini A, Foschi F. Reparative procedures for endodontic perforations: towards a standardised approach ENDO EPT 2020;14(3):217–228
2- Gorni FG, Andreano A, Ambrogi F, Brambilla E, Gagliani M. Patient and clinical characteristics associated with primary healing of iatrogenic perforations after root canal treatment: results of a long-term Italian study. J Endod 2016;42:211–215.
3- Hashem AA, Wanees Amin SA. The effect of acidity on dislodgment resistance of mineral trioxide aggregate and bioaggregate in furcation perforations: an in vitro com- parative study. J Endod 2012;38:245–249.
4- Torabinejad M, Parirokh M, Dummer PMH. Mineral triox- ide aggregate and other bioactive endodontic cements: an updated overview – part II: other clinical applications and complications. Int Endod J 2018;51:284–317.