
A diagnostic conundrum
01/02/2024
Federico Foschi
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Multi-rooted teeth in the upper arch can present diagnostic difficulties. Vitality testing can result in erratic response due to necrobiosis status of the pulp. The aid of CBCT scan to rule out the presence of vertical root fractures is highly recommended. In general cracks are not visible on CBCT scans (Brady et al, 2014), however bone loss patterns can be detected. Cleaning and shaping with martensitic rotary files followed by activation of the irrigants and the bioceramic sealer allowed infill of a lateral portal of exit.
The patient presented with an unremarkable swelling on the palatal vault in proximity of the upper right second molar. The patient did not complain of any specific symptom or discomfort except some occasional bad taste as the boil would occasionally burst. On clinical examination the upper right first and second molars both presented with composite restoration. Special tests revealed a normal response to Endofrost on all teeth in the upper right quadrant, with a slight delay on the upper right second molar. Fistulography revealed that the sinus tract did not originate from the apical third of any root.
Due to unclear diagnostic features and the anatomical noise present in the area (maxillary antrum and overlapping roots) a small field CBCT scan was obtained. In these situations CBCT represents an appropriate imaging option to opt for the most appropriate treatment plan (Gliga et al., 2023). A visible hairline on the palatal root of the UR7, associated with a palatal cortical bone dehiscence was detected on the axial plane which led to suspicion of vertical root fracture, however observing the coronal plane of the scan the hairline appeared as isolated and linear consistent with the presence of a lateral canal with a palatal portal of exit. The axial plane also confirmed the presence of a single MB canal.
Interestingly limited periapical lesion was detected on the three roots, with minimal widening on the long DB root.

Fig. 1
Long cone periapical x-ray showing the guttapercha point inserted in the palatal sinus tract (Fistulography), with inconclusive findings, due to unclear origin.
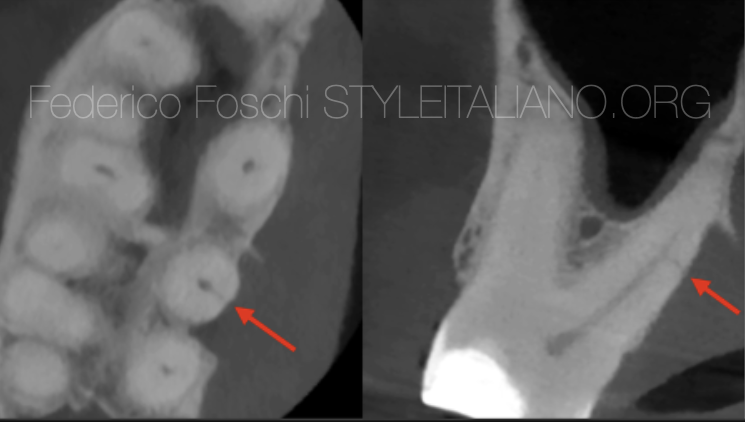
Fig. 2
Axial plane on the left showing cortical bone loss and a thin hairline consistent with potential VRF, however the coronal plane showed a limited corona-apical extension consistent with a lateral canal.
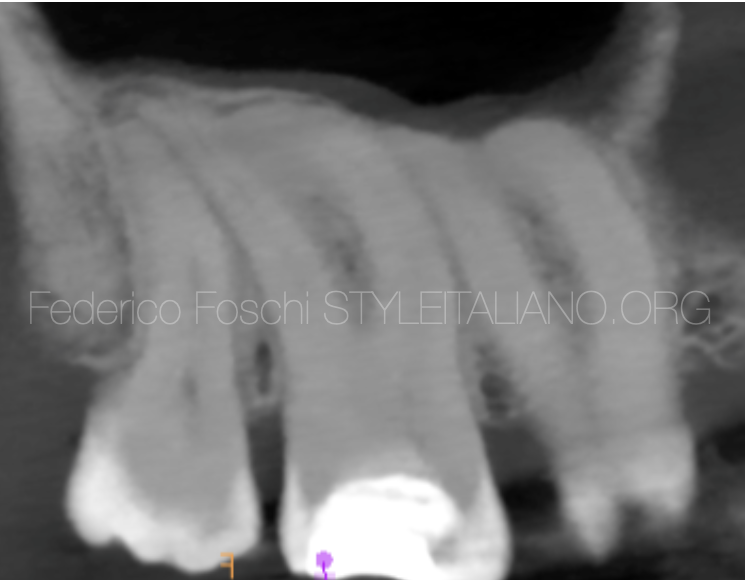
Fig. 3
Limited apical widening present on the DB root of the UR7. The DB canal was pre-measured on the CBCT as 25.5mm long.

Fig. 4
Master apical cones long cone periapical x-ray showing a good fit of the GP points.

Fig. 5
Final post-operative x-ray showing infill of the palatal lateral canal on the UR7.
Conclusions
Following local infiltration with articaine and single tooth rubber dam isolation the existing composite restoration, which appeared to be defective, was removed. Necrobiosis was detected with coexisting buccal canals partially vital and pus discharge on the palatal root.
The pre-measured working length determined on the CBCT scan was utilised due to its high reliability (Paterson et al. 2020). No hand file instrumentation was opted to minimise the chances of ledging and iatrogenic errors: mechanical scouting files have been used linked to the electronic apex locator to confirm full canal patency. A orifice widener has been used in reversed sequence order after the scouting mechanical files with brushing action to minimally countersink the canal orifices. Subsequently the rotary shaping files have been brought to full working length in all canals. A continuous irrigation protocol has been followed (2% NaOCl alternated to 17% EDTA) with activation for 30 seconds for each canal. The MAC LCPA confirmed appropriate taper and WL fit of the guttapercha points. Following sterile paper point drying bioceramic sealer have been deployed in all canals. A further 10 second activation has been carried out in the palatal canal. A hybrid single cone/coronal third backfill obturation technique was opted for. Final LCPA revealed a satisfactory result with infill of the palatal canal. The patient has been reviewed at one month confirming healing of the palatal fistulous tract. Twelve months review will be arranged.
Bibliography
Brady E, Mannocci F, Brown J, Wilson R, Patel S. A comparison of cone beam computed tomography and periapical radiography for the detection of vertical root fractures in nonendodontically treated teeth. Int Endod J. 2014 Aug;47(8):735-46.
Gliga A, Imre M, Grandini S, Marruganti C, Gaeta C, Bodnar D, Dimitriu BA, Foschi F. The Limitations of Periapical X-ray Assessment in Endodontic Diagnosis-A Systematic Review. J Clin Med. 2023 Jul 12;12(14):4647. doi: 10.3390/jcm12144647.
Paterson A, Franco V, Patel S, Foschi F. Use of preoperative cone-beam computed tomography to aid in establishment of endodontic working length: A systematic review and meta-analysis. Imaging Sci Dent. 2020 Sep;50(3):183-192.




