Management of double iatrogenic perforation step by step
24/09/2023
José Conde Pais
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The American Association of Endodontists (AAE) Glossary of Endodontic Terms defines perforations as mechanical or pathological communications between the root canal system and the external tooth surface (2003). Root perforations are severe complications and are associated with compromised endodontic treatment outcomes, especially when bacterial infection is allowed to establish. Perforations may occur due to pathological processes or treatment consequences. The subsequent injury to the periodontium results in the development of inflammation, destruction of periodontal fibres, bone resorption, formation of granulomatous tissue, proliferation of epithelium, and the development of a periodontal defect (Arens & Torabinejad, 1996; Beavers et al., 1986; Seltzer et al., 1970; Tsesis & Fuss, 2006) .The incidence of perforations is quoted in the literature as being between 0.7% and 10% (Eleftheriadis & Lambrianidis, 2005; Fuss & Trope, 1996; Ingle, 1961; Olcay et al., 2018).
In relation to the prognostic factors of a perforation we can state, according to the existing literature, the following:
- Time The immediate sealing is mandatory to prevent the infection
- Location Middle third and Apical third better prognosis but difficult management
- Size > 3 mm less favourable long-term prognosis
- Probing + Probing less favorable long-term prognosis
The use of bioactive materials, such as mineral trioxide aggregate (MTA) and other calcium-silicate cements, promotes a favourable environment for regeneration and has been used successfully for perforation repair.
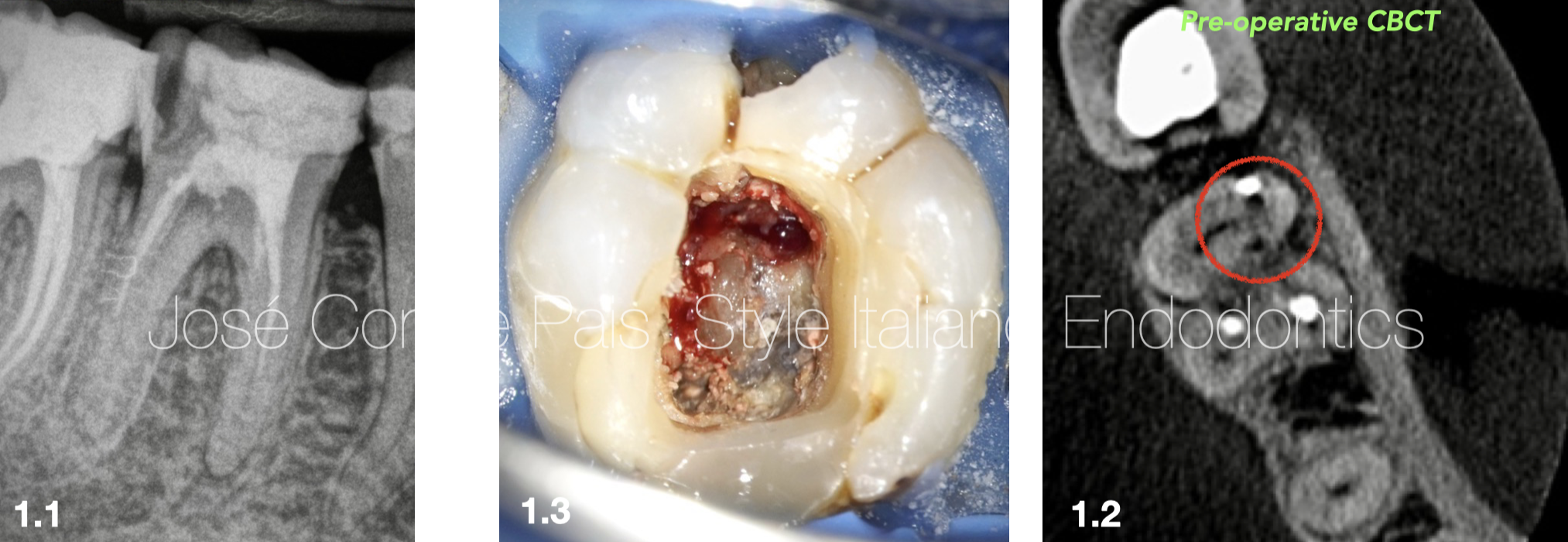
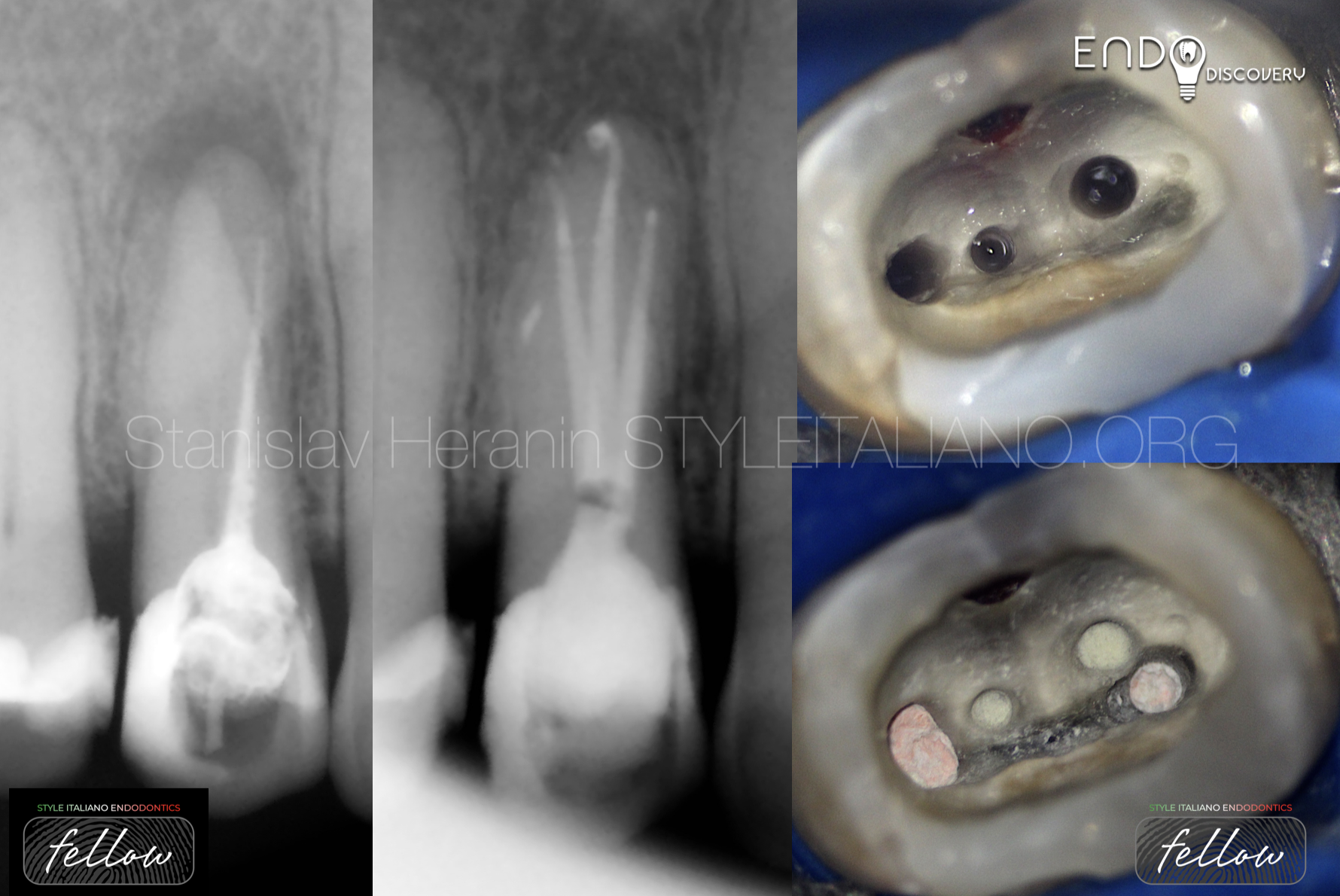
Fig. 1
A 30 years old male patient was referred from a general Practitioner to my clinic for management of furcal perforation and root canal retreatment.
After a clinical and radiographic examination, we observe the following :
Tooth 46 presents double iatrogenic furcal perforation , poor endodontic treatment, asymptomatic apical periodontitis and physiological probing.
We decide to perform a non-surgical approach under surgical microscope. The patient was informed of the pros and cons of the treatment and signed the informed consent.
1.1. Pre-operative X-ray
1.2. Pre-operative CBCT
1.3. Pre-operative Image
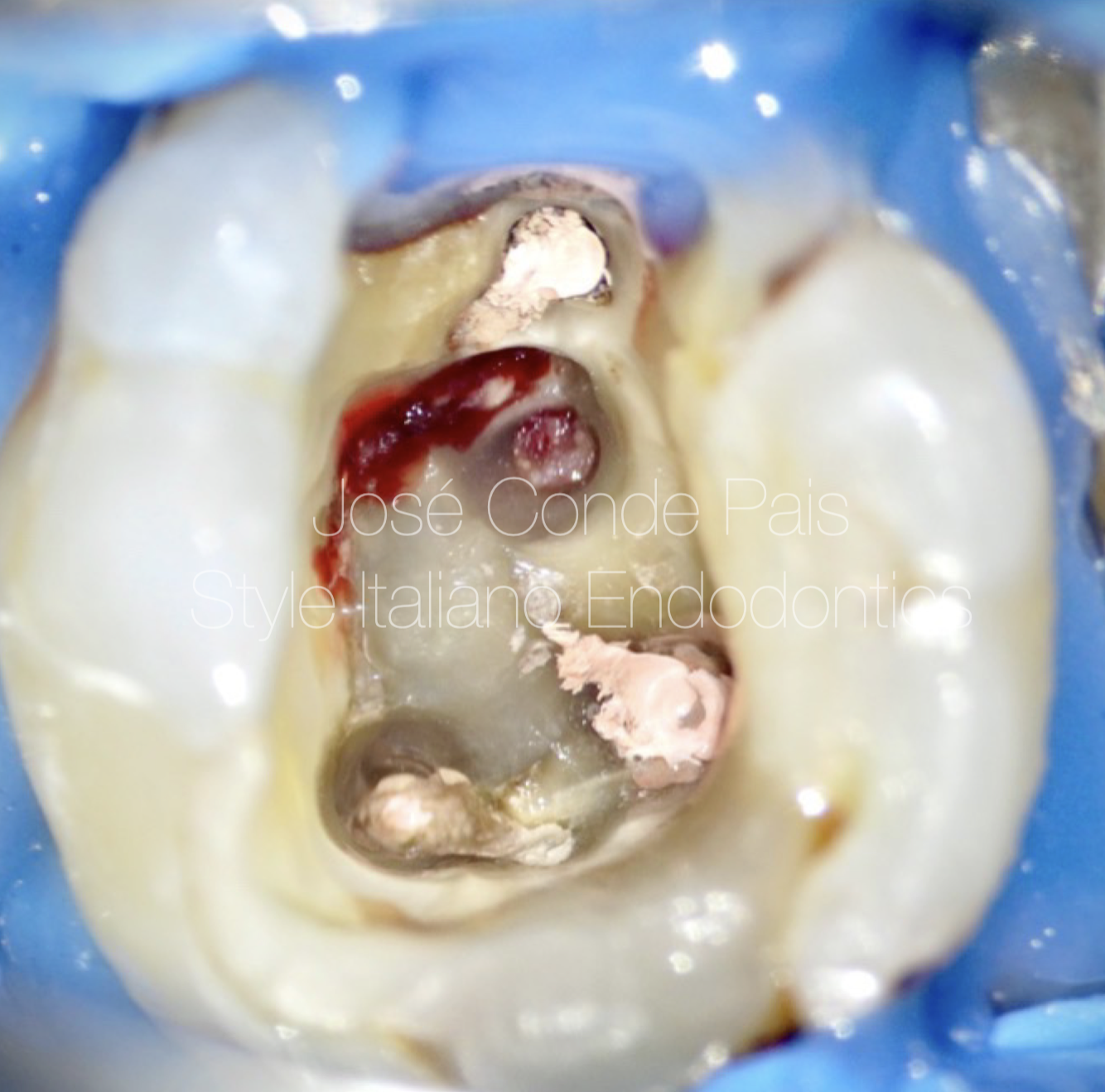
Fig. 2
Acces Cavity was redefine and the chamber floor cleaned using ultrasonic tips.
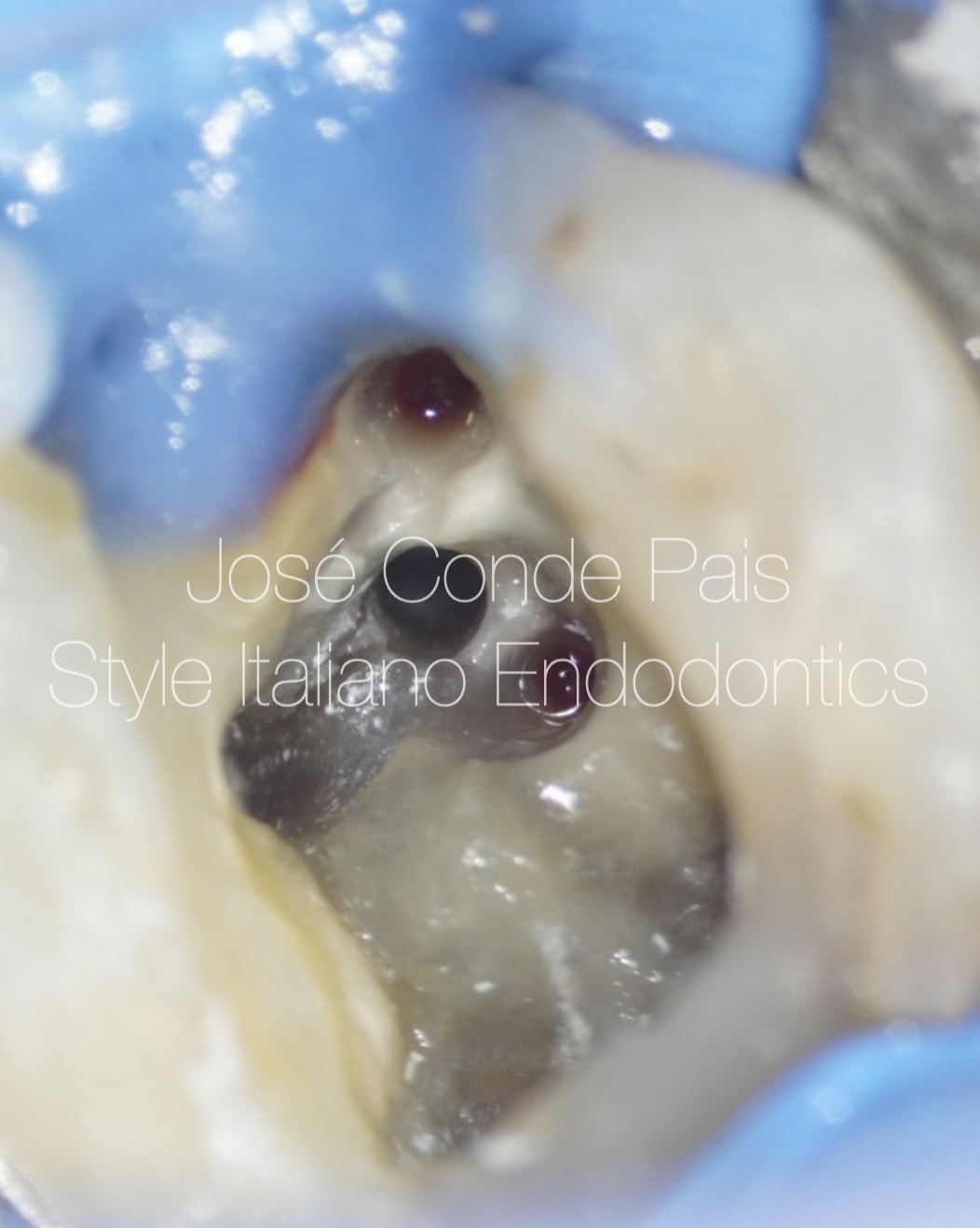
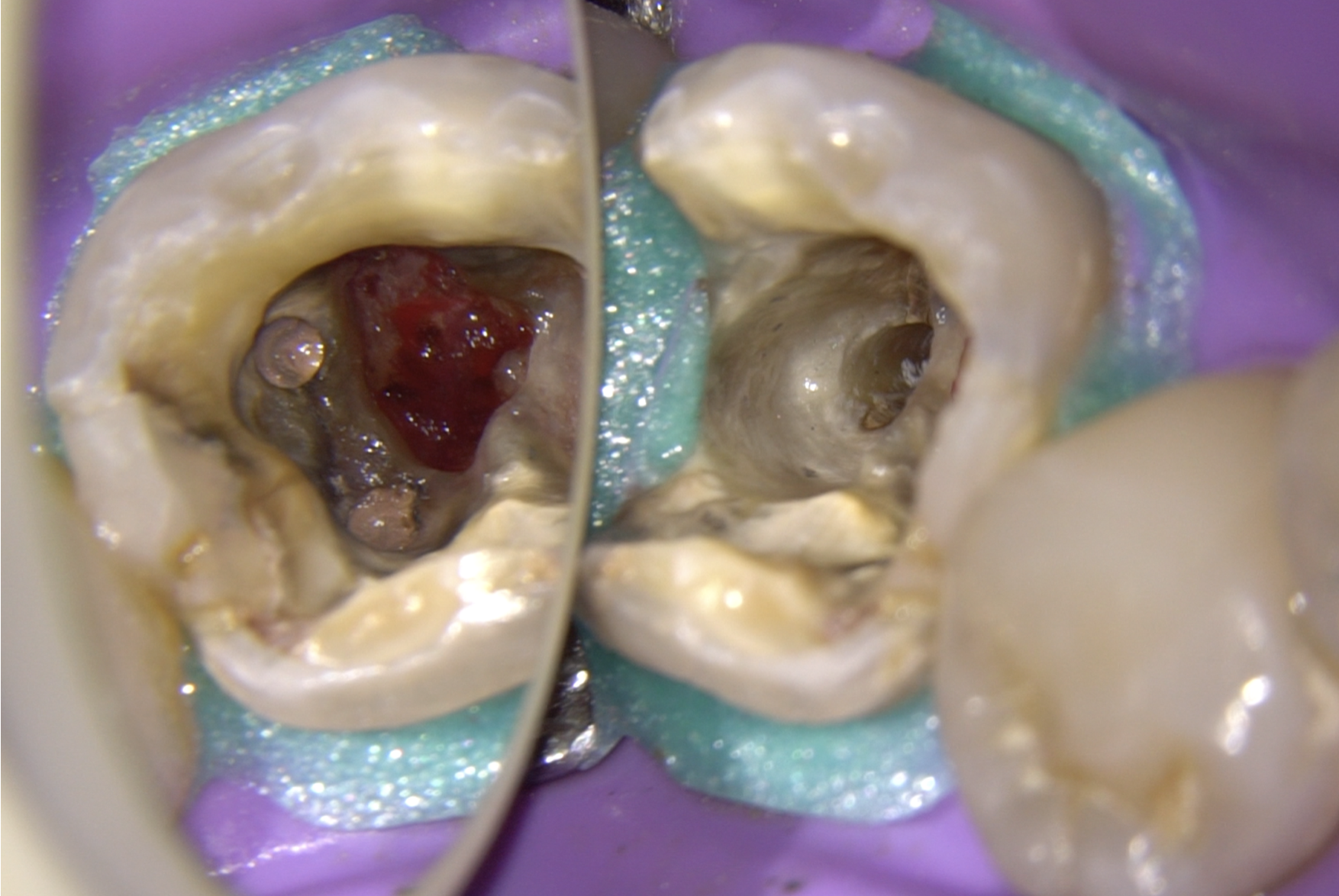
Fig. 3
The Root Canal System was prepared and disinfected with rotary files and iatrogenic perforations were located and disinfected.

Fig. 4
Intracanal medication (calcium hydroxide) was placed for 15 days to improve the bacterial environment.
4.1. Pre-operative X-ray
4.2. Intracanal X-ray
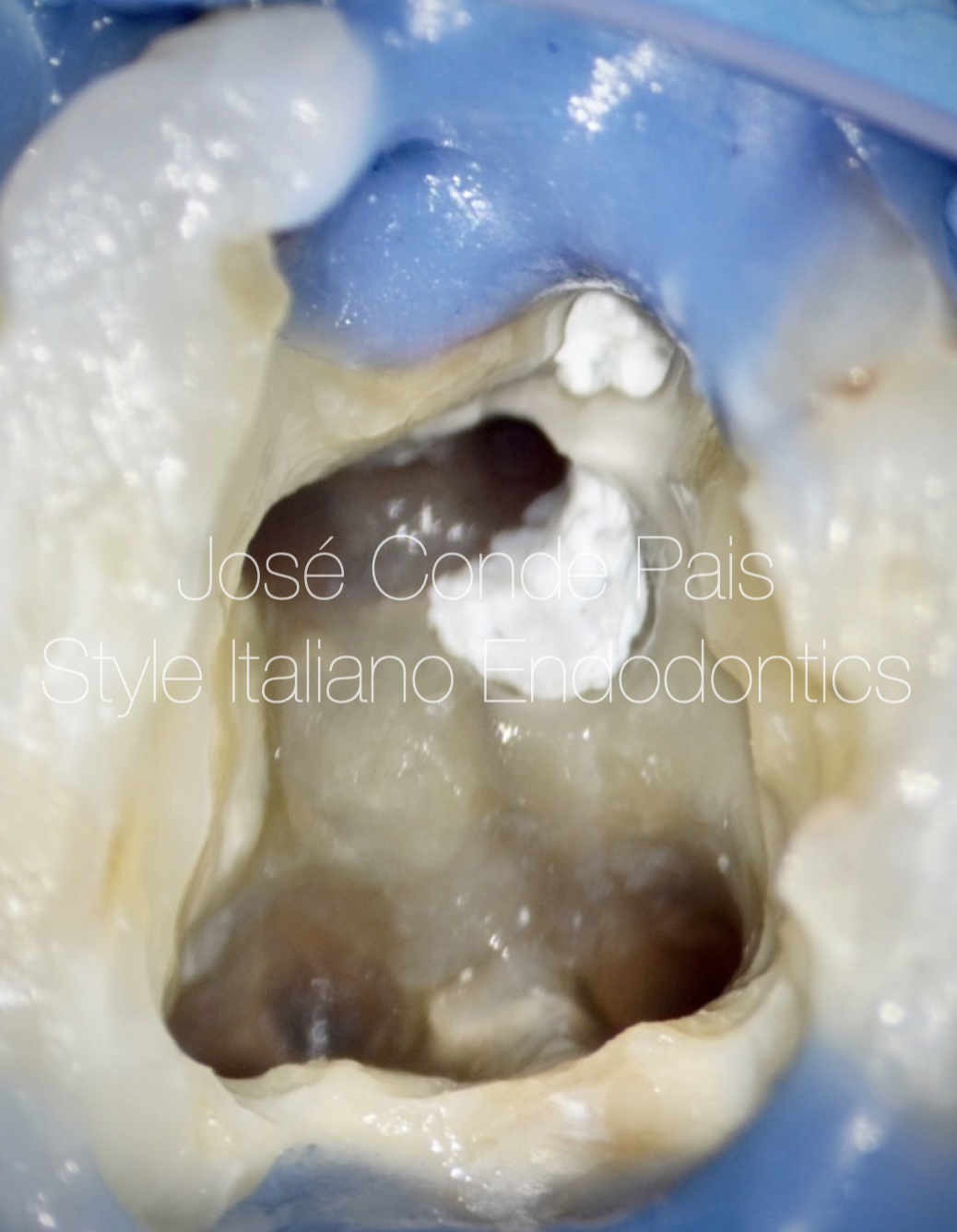
Fig. 5
Iatrogenic perforations were temporarily sealed with sterile Teflon (to avoid contamination by sealer and gutta-percha) and root canal retreatment was performed.
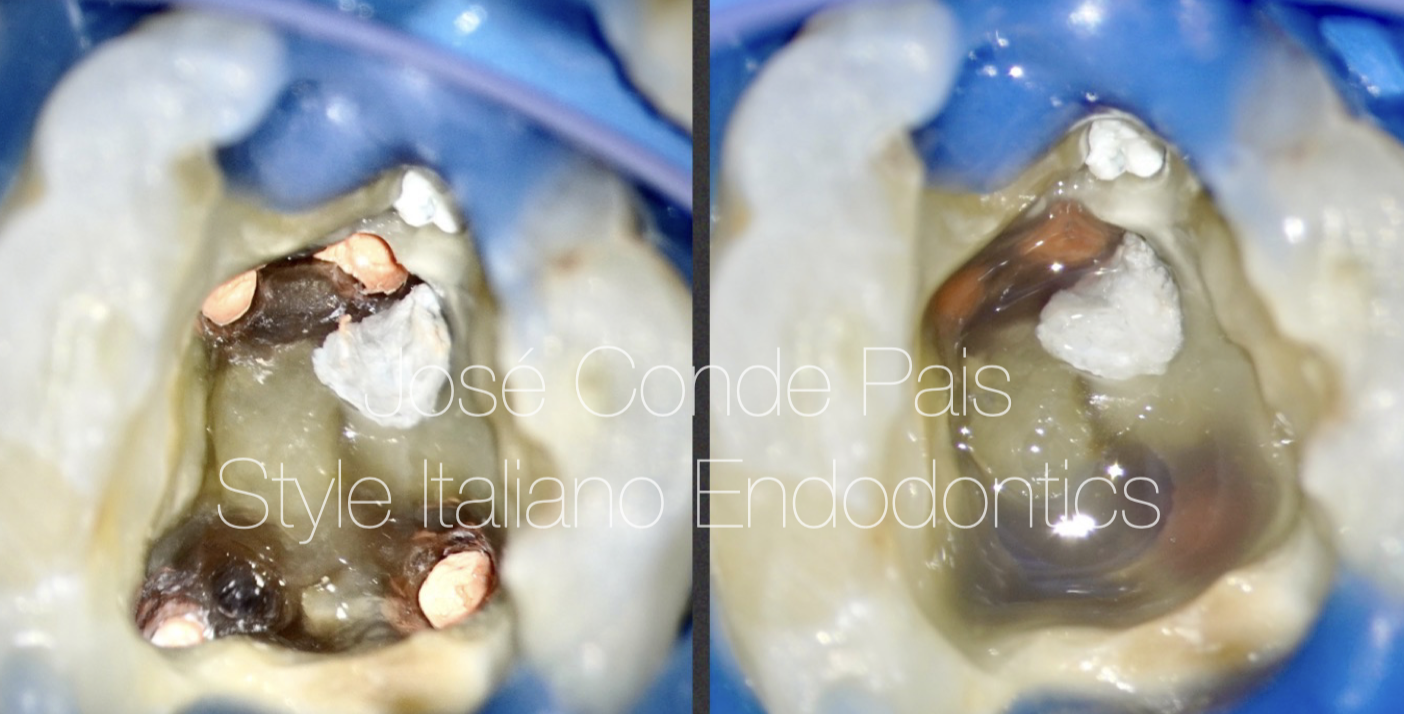
Fig. 6
The entrance of the canals was sealed with composite before to perforation management.
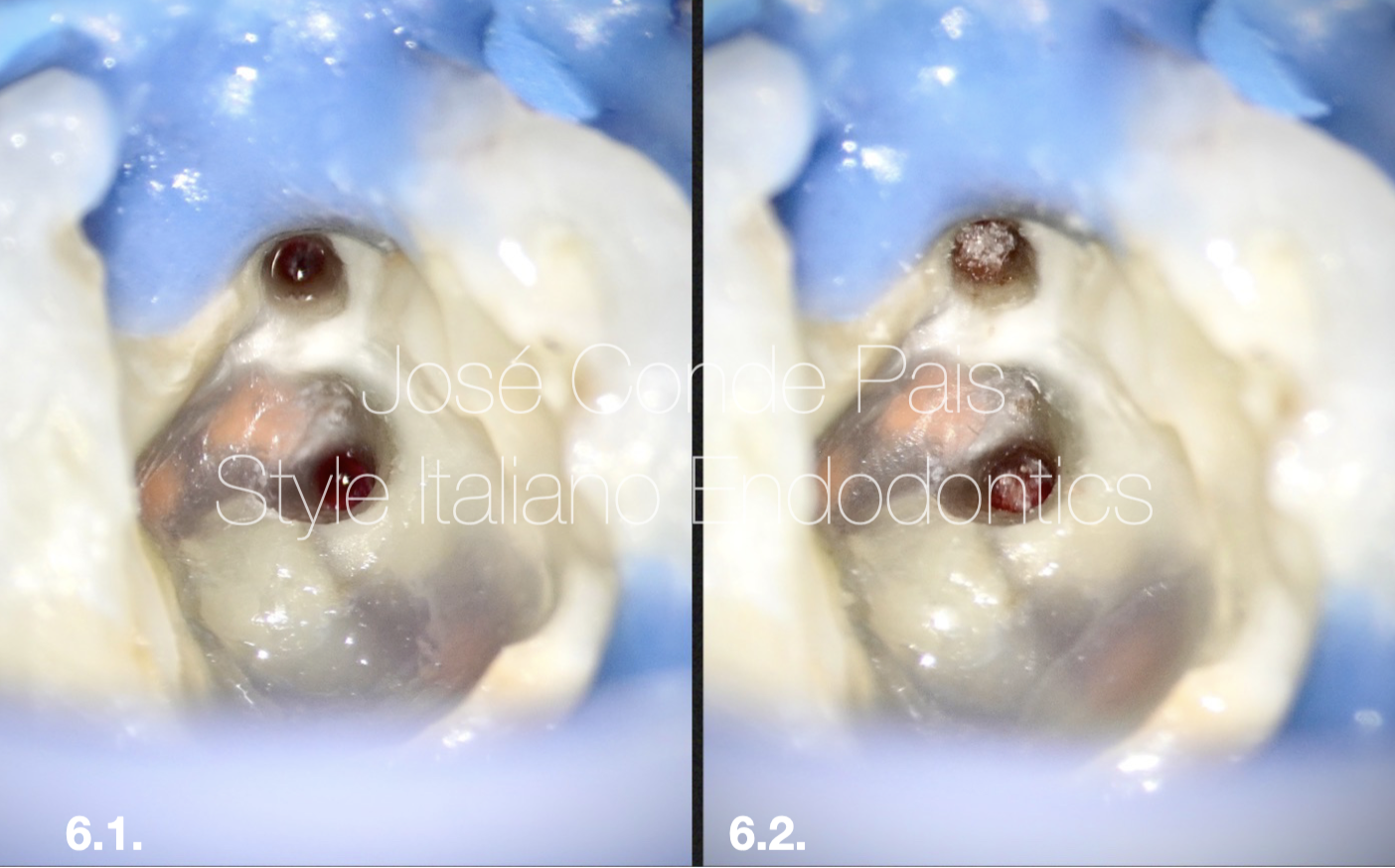
Fig. 7
6.1. The margins of the perforations were enlarged and cleaned with ultrasonic tips to remove contaminated tissue.
6.2. Collagen matrix was placed into the perforation to avoid extrusion of the bioceramic material.
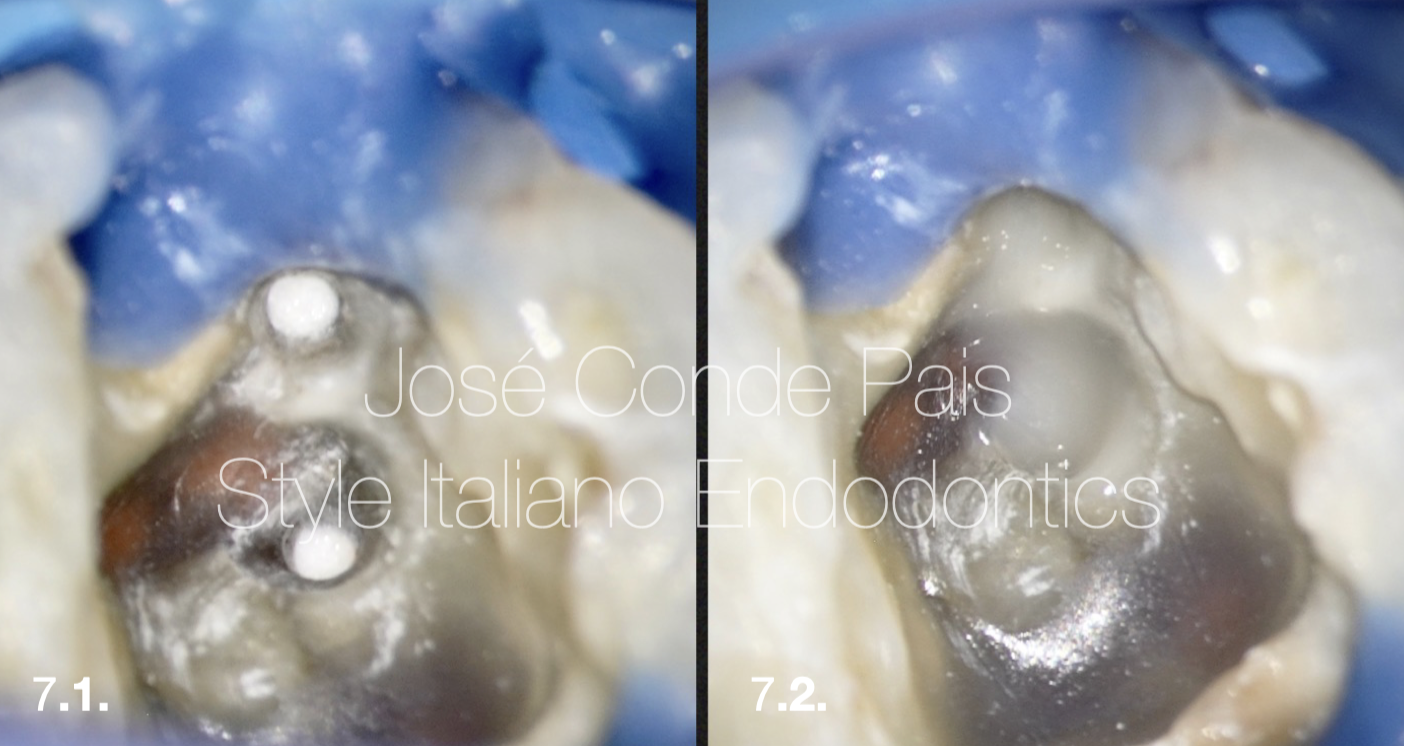
Fig. 8
7.1. Iatrogenic perforations were sealed using Neo-Mta and the Maps system as carrier.
7.2. Glass ionomer was used to protect the bioceramic material.

Fig. 9
Final X-Ray

Fig. 10
1 Year recall showing good healing.
Conclusions
In conclusion, root perforations are serious complications that reduce the prognosis of endodontic procedures and can cause tooth loss. The operating microscope facilitates endodontic procedures and reduces the risk of unnecessarily weakening or perforating a tooth in complicated clinical situations. MTA is an excellent material for perforation repair.
Bibliography
1. Gorni FG, Andreano A, Ambrogi F, et al. Patient and clinical characteristics associated with primary healing of iatrogenic perforation after root canal treatment: results of a long-term Italian study. J Endod. 2016;42 (2):211-215.
2. Clauder T. Present status and future directions - Managing perforations. Int Endod J. 2022 Oct;55 Suppl 4:872-891.
3. American Association of Endodontists. Treatment Options for the Compromised Tooth: A Decision Guide .
4. Tsesis I, Fuss Z. Diagnosis and treatment of accidental root perforations. Endod Top 2006;13:95–107.