
Internal Bleaching as a Conservative Alternative to Veneers in Root Canal-Treated Tooth
12/02/2026
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Nowadays, the field of aesthetics is becoming more and more important, especially when it comes to having a beautiful smile since it affects a person's psychological well-being and how they perceive their own beauty. When an isolated chromatic change happens, the impact of pigmented teeth is stronger since the difference with the remaining teeth is more noticeable.Numerous factors, such as dental trauma, necrotic debris on the pulp horns and dentinal tubules, inadequate irrigation, or sealing materials in the pulp chamber or chamber walls, can cause non-vital tooth discolouration . Intracoronal blood breakdown is the most frequently mentioned cause. Iron is released when erythrocytes hemolyze in the dentin tubules. This and hydrogen sulphate combine to generate ferric sulphide, a dark chemical that causes tooth discolouration. Internal tooth bleaching is a minimally invasive, conservative, relatively simple, effective, and low-cost method in the treatment of discolored endodontically treated teeth

Fig. 1
Clinically the patient chief complain suffering from grayish discoloration of the upper right central incisor with no signs and symptoms of any pain and tenderness, Vitality test was done to the tooth with ethyl chloride and the result showed negative response (the tooth is non vital).

Fig. 2
Pre-op X-Ray showed upper right central incisor with normal periapical status
The patient’s dental history revealed a previous traumatic incident involving the affected tooth approximately seven years earlier, which likely contributed to the subsequent discoloration.
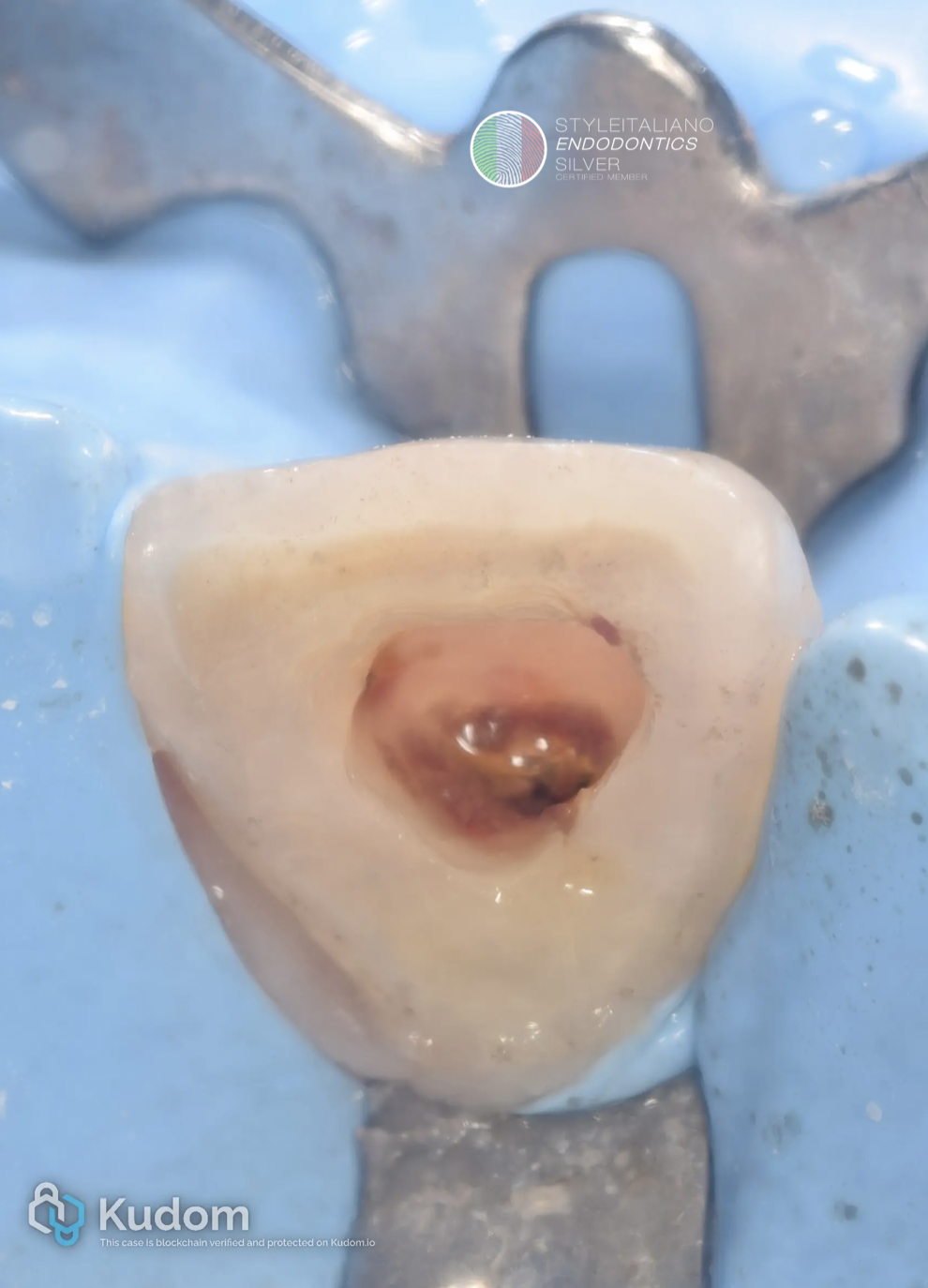
Fig. 3
Rubber dam isolation.
Access opening from the palatal surface
Removing of the necrotic tissue and dentin even from the pulp horn
copious amount of NaOCl 5.25% to decrease the amount of bacterial load from the pulp chamber to reduce the possibility of flare up

Fig. 4
Clean cavity
Straight line access to the canal chemomechanical shaping and cleaning
- Rotary file 17/04
- Rotary file 25//04
- Rotary file 30/04
- Rotary file 35/04
with copious amount of NaOCl 5.25% with ultrasonic activation for 1 minutes, then EDTA to remove the smear layer and followed again with NaOCl to disinfect again.

Fig. 5
Apical gauge to the master apical cone confirmed.
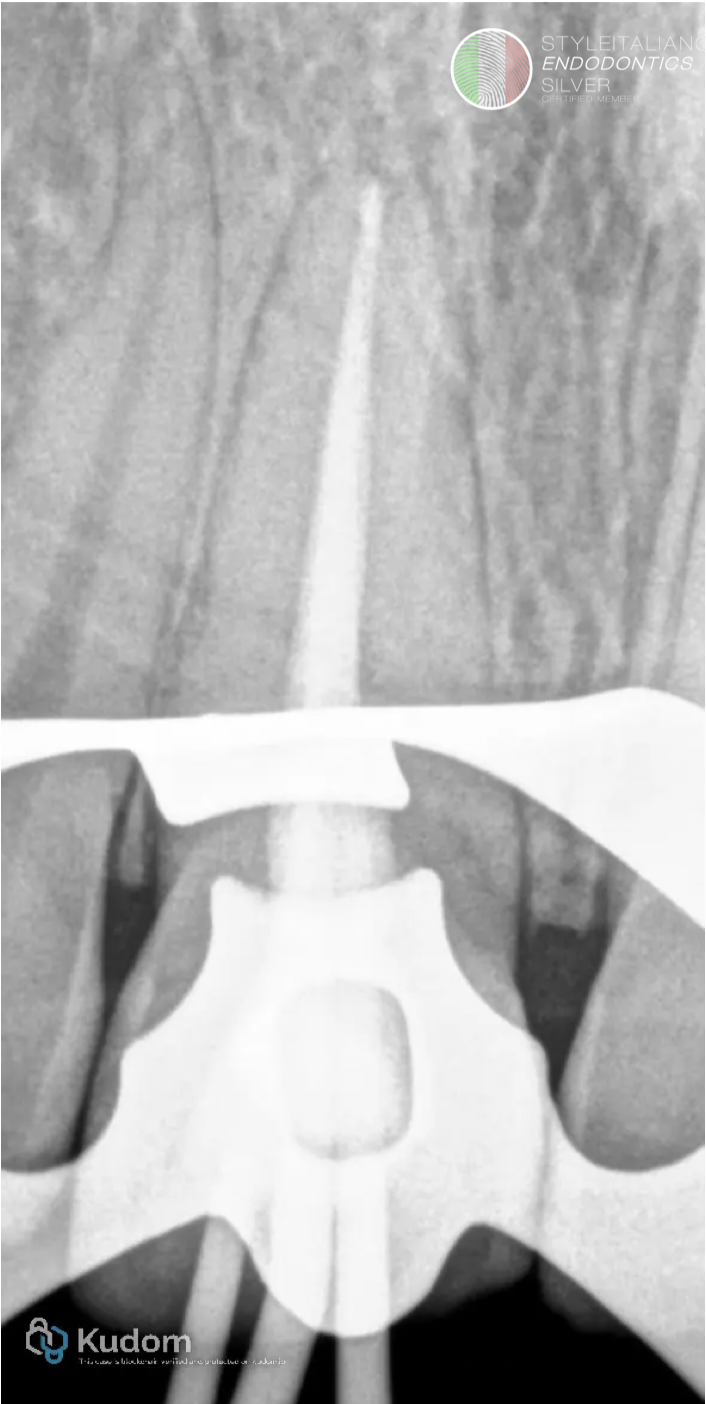
Fig. 6
Obturation of the canals by single cone with bioceramic sealer and down back of the cones with obturation pen.

Fig. 7
Final obturation and the gutta-percha condensed 1mm below the orifice.

Fig. 8
Resin modified glass ionomer was applied above the gutta-percha to provide sealing to prevent the leakage of the internal bleaching material thus avoiding the possibility of external cervical resorption of the tooth.

Fig. 9
Internal bleaching (35% hydrogen peroxide) gel was introduced into the pulp chamber cavity for 5 days and the cavity sealed with glass ionomer filling material
After 5 days the bleaching material was washed with normal saline and the cavity sealed again with glass ionomer for two weeks to prevent any effect from the residual bleaching material on the bonding of the final composite restoration.
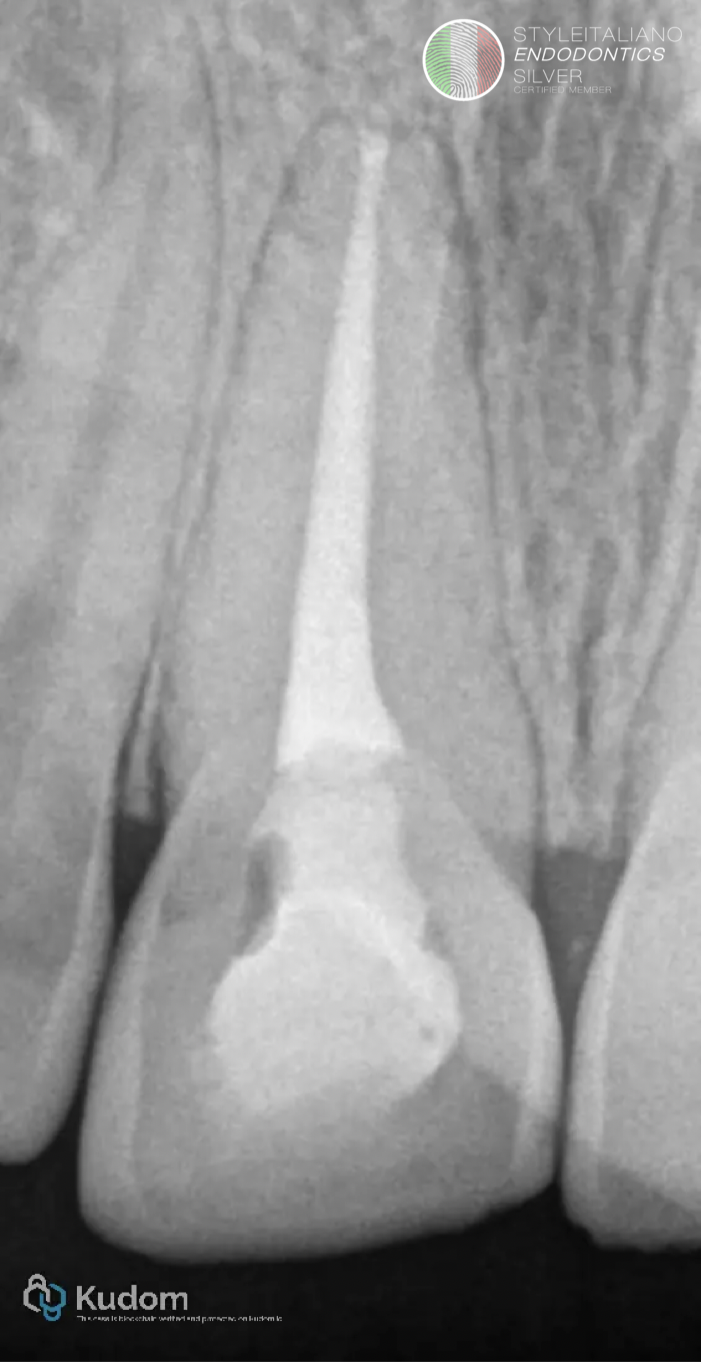
Fig. 10
Post-op X-Ray with final restoration.

Fig. 11
Follow up after one month showing excellent transformation from gray to natural shade.

Fig. 12
Before and after treatment.
Conclusions
Regardless of the technique used, internal bleaching is a conservative, simple, effective, and low-cost procedure, with good esthetic results, in the treatment of non-vital tooth discolorations. The cervical barrier is a standard of care in internal bleaching techniques and should be used.
Bibliography
- Joiner, A.; Luo, W. Tooth colour and whiteness: A review. J. Dent. 2017, 67S, S3–S10.
- Montero, J.; Gomez-Polo, C.; Santos, J.A.; Portillo, M.; Lorenzo, M.C.; Albaladejo, A. Contributions of dental colour to the physical attractiveness stereotype. J. Oral Rehabil. 2014, 41, 768–782.
- Al-Zarea, B.K. Satisfaction with appearance and the desired treatment to improve aesthetics. Int. J. Dent. 2013, 2013, 912368.
- Zimmerli, B.; Jeger, F.; Lussi, A. Bleaching of nonvital teeth. A clinically relevant literature review. Schweiz. Mon. Zahnmed. 2010, 120, 306–320.
- Plotino, G.; Buono, L.; Grande, N.M.; Pameijer, C.H.; Somma, F. Nonvital tooth bleaching: A review of the literature and clinical procedures. J. Endod. 2008, 34, 394–407.



