
Endo-resto management of two molars with failed old large amalgam restoration
27/01/2026
Fellow
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Failed amalgam restorations in posterior teeth remain a common clinical challenge in restorative dentistry, particularly in lower molars that are subjected to high occlusal forces. Over time, amalgam restorations may fail due to factors such as marginal breakdown, secondary caries, corrosion, or fracture of the remaining tooth structure, leading to pulpal complications. Sometimes bacterial leakage beneath defective restorations may result in pulpal necrosis and periapical involvement. The management of two lower molars with failed amalgam restorations therefore requires a comprehensive clinical approach that includes accurate diagnosis, evaluation of pulpal status, and appropriate treatment planning. This article presents the management of two lower molars with failed amalgam restorations, one of which required root canal treatment due to pulp necrosis, followed by definitive restorative rehabilitation to restore function and long-term tooth survival.

Fig. 1
The pre-operative intraoral photograph shows two adjacent mandibular molars restored with extensive amalgam restorations. Both restorations appear old and defective, with evident marginal breakdown and loss of anatomical contour. The proximal margins between the two molars are compromised, with food and plaque accumulation and recurrent caries. Discoloration around the restoration margins and areas of exposed tooth structure indicate microleakage and deterioration of the remaining enamel and dentin. The surrounding gingival tissues appear mildly inflamed, likely due to plaque retention associated with the defective restorations. These clinical findings, in conjunction with the radiographic assessment, confirm the failure of the existing amalgam restorations and the need for comprehensive restorative management, including endodontic treatment for the affected tooth followed by definitive coronal restoration.

Fig. 2
The pre-operative radiograph show two adjacent lower molars restored with large amalgam restorations. Both restorations show signs of failure, particularly at the proximal area between the two teeth. In the first molar, there is loss of normal pulpal architecture with a periapical radiolucency, indicative of pulp necrosis and associated periapical pathology. The second molar appear radiographicaly normal with no periapical changes , and it’s gives possitive response to the vitality testes .
These clinical and radiographic findings support the need for endodontic treatment for the necrotic tooth, followed by appropriate definitive restorative management for both molars.
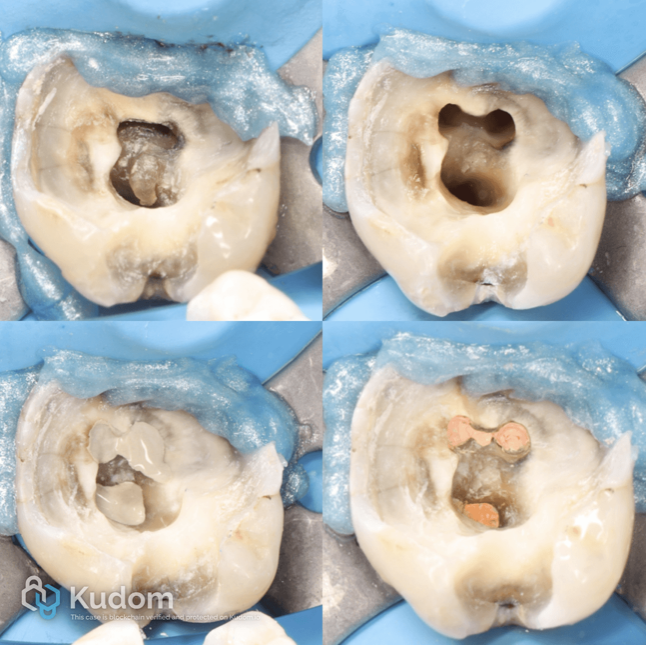
Fig. 3
After removing old amalgam restoration , recurrent caries from the lower six , the tooth was isolated using a rubber dam, the canals orifices were located, the root canals were enlarged, shaped cleanend , and then Obturated with a single cone with bioceramic sealer

Fig. 4
Periapical radiographs Illustrated the endodontic treatment of lower 6 adequate shaping , cleaning, and three-dimensional obturation of the root canal system, suggesting a favorable prognosis.

Fig. 5
After complete removal of old amalgam restoration , the two molars restored and prepared following the principles of biomimetic dentistry under rubber dam isolation. The cavity design appears conservative, with maximal preservation of sound tooth structure , which is fundamental to maintaining the tooth’s biomechanical integrity.
The restoration exhibit a build-up with a smooth, well-adapted adhesive interface, suggesting the use of stress-reducing bonding protocols. The rounded internal line angles and absence of sharp edges help to minimize stress concentration within the dentin, closely mimicking the natural stress distribution of an intact tooth.
The dentin replacement layer restores lost dentin volume and stiffness, allowing the composite to function as a biomimetic substitute for natural dentin. The peripheral enamel margins are preserved and appear continuous, providing an ideal substrate for durable enamel bonding and long-term marginal seal.
Overall, this image reflects a biomimetic approach aimed at re-establishing the tooth’s original structural resilience, enhancing fracture resistance, and promoting long-term clinical success by replicating the mechanical behavior of natural tooth tissues rather than relying on aggressive preparation or full-coverage restorations.

Fig. 6
The post-operative clinical photograph demonstrates overlay restorations with precise marginal adaptation, appropriate occlusal morphology, and satisfactory shade integration. The restorations exhibit a smooth surface finish and harmonious contours with adjacent teeth. Peri-restorative soft tissues appear healthy, indicating favorable biological response. Overall, the restorations achieved optimal functional performance and acceptable esthetic outcomes.

Fig. 7
One-and-a-half–year clinical follow-up demonstrating stable restorations with satisfactory marginal adaptation, preserved occlusal anatomy, and healthy surrounding soft tissues, indicating favorable long-term clinical performance.

Fig. 8
One-and-a-half–year radiographic follow-up demonstrating maintained obturation integrity, healing of periapical lesion, and absence of pathological changes, indicating favorable long-term endodontic outcome

Fig. 9
About the author:
Ali Abd
Iraq , Babil , 1995
Graduated from babylon university (2019)
Participant in many endodontic internal and national conferences and courses
Endodontic Lecturer and trainer
Microscopic endodontist
Advisory member at maruchi company
Pro user at orodeka company
Owner of Perfect care dental clinics
Conclusions
The successful outcome of this case highlights the importance of accurate endodontic procedures combined with appropriate restorative rehabilitation. High-quality canal obturation and well-executed final restorations played a critical role in preserving tooth structure and achieving predictable clinical and radiographic results.
Bibliography
Sabeti, Mehrdad, et al. “Clinical Factors Influencing the Prognosis of Endodontically Treated Teeth: A Contemporary Review.” International Endodontic Journal, vol. 57, no. 3, 2024, pp. 215–228.
Zavattini, Andrea, et al. “Clinical and Radiographic Outcomes of Root Canal Obturation Using a Tricalcium Silicate-Based Bioceramic Sealer.” Biomimetics, vol. 10, no. 11, 2025, article 412.
Magne, Pascal. “Immediate Dentin Sealing: A Fundamental Procedure for Indirect Bonded Restorations.” Journal of Esthetic and Restorative Dentistry, vol. 17, no. 3, 2005, pp
Magne, Pascal, et al. “Influence of Dentin Sealing on Bond Strength of Indirect Restorations.” Journal of Prosthetic Dentistry, vol. 91, no. 6, 2004, pp. 534–542,




