
Clinical Insights into the Middle Distal Canal of Mandibular Molars: A Case Report.
16/04/2025
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The middle distal canal in mandibular molars is a rare but clinically significant anatomical variation. Its prevalence varies from 0.26% to 9.6%, influenced by population differences and detection methods like CBCT or micro-CT. Challenges in detection arise due to its location in the isthmus, small diameter, and potential calcification. Effective treatment involves careful canal negotiation, enhanced irrigation techniques, and precise obturation methods. Accurate diagnosis and management are essential for successful outcomes, emphasizing the need for advanced diagnostic tools and clinician expertise in endodontic practice

Fig. 1
A female patient, 18 years old with no concomitant diseases, was referred for endodontic treatment of tooth 46. The referring doctor included an CBCT scan. CBCT examination 5cmx5cmx5cm front section showed the presence of massive apical lesion tooth 46. On extra-oral examination, no abnormalities, lymph nodes not palpable and not painful, skin coat without changes. On intra-oral examination, tooth 46 with deep caries. Percussion,,+,, palpation,,-,, no pockets, no mobility, The application of cold stimulus elicited a strong and prolonged reaction, indicating heightened sensitivity. diagnosis: irreversible symptomatic pulpitis and symptomatic apical periodontitis (SIP/SAP) tooth 46 The patient was informed of the clinical situation, possible complications, and prognosis.
Fig. 2
CBCT examination 5cmx5cmx5cm cross-section showed the presence of long isthmus in distal root canal. The periapical tissues were unchanged, and no perforation or transport of anatomical orifices was found.

Fig. 3
The appearance of the pulp chamber after pre-endodontic buildup and after the phases of shaping and cleaning.

Fig. 4
Through the dental microscope, this image reveals the middle distal canal. Nestled within the isthmus between the main distal canals, its small, subtle orifice demonstrates the intricate nature of root canal anatomy.

Fig. 5
After a previous thorough CBCT analysis, minimally invasive instrumentation of MB and ML canals by crown down to ISO 40.04 and DB,DM,DL ISO40.04 was implemented. Performed disinfection of the endodontic space with 5.25% sodium hypochlorite solution and 40% citric acid solution. The liquids were activated with PUI. An intra-oral radiograph was taken in an oblique projection with gutta-percha points. The radiograph confirmed proper canal preparation.

Fig. 6
Obturation was performed using the vertical compaction method using AH+ epoxy sealer and calibrated gutta-percha cones; calibration was performed with a calibration ruler. After obturation, an intra-oral radiograph was taken in oblique projection - the canals were filled correctly.
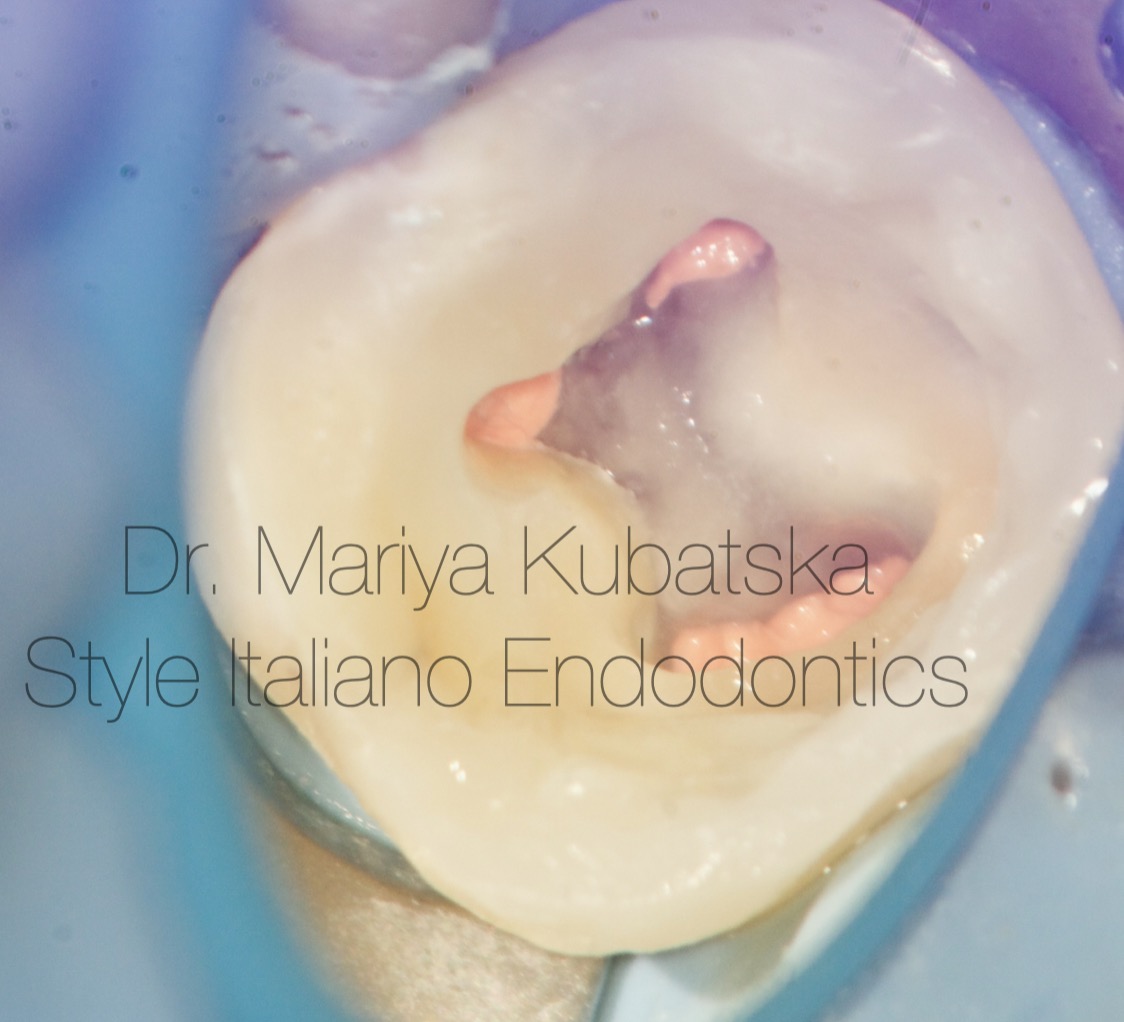
Fig. 7
The view of the pulp chamber after obturation of root canals and after air-abrasion treatment.

Fig. 8
Mariya Kubatska graduated medical university of Gdansk in 2014. Since graduation, I have been highly interested in Endodontics. Member of the European Society of Endodontology, the American Association of Endodontists, the Polish Endodontic Association, and the Department of Endodontology of the Polish Dental Society. Since 2023, Style Italiano Endodontics fellow. International speaker. Lecturer in Esdent and MCS Karas Dental Training centers. Author of case reports in Polish dental magazines. Since 2018, Mariya has worked in Oslo, Norway, focusing on endodontics, in private life piano lover.
Conclusions
The middle distal canal, often overlooked in routine endodontic assessments, plays a critical role in the success of mandibular molar treatments. Systematic reviews and clinical studies have underscored its variable prevalence and the challenges it presents in both detection and treatment. The small size, complex anatomy, and location of this canal often make it difficult to identify without advanced diagnostic techniques. By incorporating tools such as cone-beam computed tomography (CBCT), dental microscopes, and modern instruments, clinicians can more effectively detect and treat these canals. This approach not only prevents missed canals but also enhances treatment outcomes, ensuring long-term tooth preservation and reducing the risk of post-treatment complications. Ultimately, a comprehensive understanding of canal morphology, paired with meticulous techniques, improves the predictability and success of endodontic procedures, benefiting patient care and satisfaction.
Bibliography
1.Ahmad, M., et al. (2020). "The Prevalence of Middle Mesial Canals in Mandibular Molars: A Systematic Review and Meta-analysis." Journal of Endodontics
2.Martins, J. N. R., et al. (2022). "Root and Canal Anatomy of Mandibular First Molars Using Micro-CT: A Systematic Review." BMC Oral Health.
3.Nascimento, E., et al. (2021). "Prevalence and Treatment Strategies for Middle Distal Canals: A Retrospective Study." International Endodontic Journal.
4.Assessment of the prevalence and configuration of middle distal canals in the mandibular molars in a Saudi subpopulation using Cone-Beam computed tomography . Faisal Alnassar a, Yousef Aldahman b, Ahmed Altuwalah a, Abdullah Aldafaas c, Ra’ed A-Sadhan d, Waleed Alnassar e, Riyadh Alroomy a,*, Basim Almulhim f, Badar Alshammari g, Saad Alnazhan h




