Pulpal Floor Perforation repair with the use of MTA cement
02/06/2024
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Perforations are among the major complications of endodontic treatments and considered to be the second greatest cause of endodontic failure. Being iatrogenic in the most cases, root perforations result in a chronic inflammatory reaction characterized by formation of granulation tissue, bone and tooth loss.
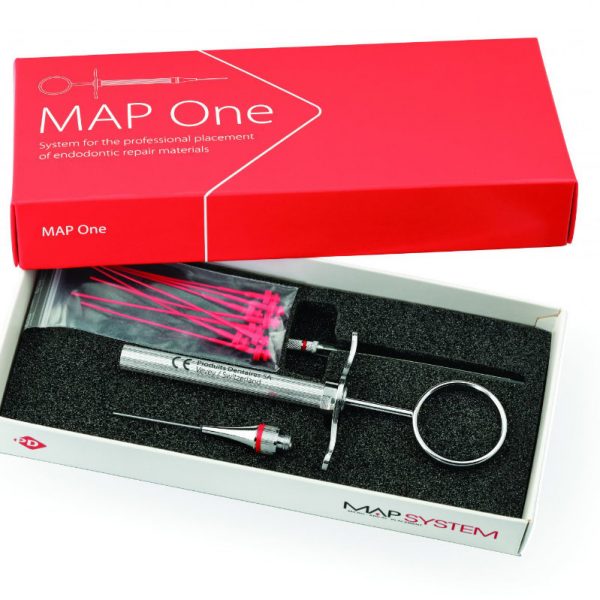
These defects should be repaired both surgically and non-surgically using biocompatible materials such as hydraulic calcium-silicate cements (MTA / Bioceramics). Present case report shows the use of MTA and periradicular matrix for the repair of a pulpal floor endodontic perforation defect and regeneration of the lost periodontium.
Challenging cases with the accidents of unpredictable endodontic root/pulp chamber floor perforations result in a high rate of clinical failure. The prognosis of a perforation defect is mostly depends on risk factors such as size, time, level of perforation and the sealing ability and biocompatibility of the of material being used. Nowadays, new technologies and biocompatible materials are used for perforation repair, MTA has been applied with good treatment outcomes owing to its properties of biocompatibility, great tissue response, good sealing in presence of moisture/blood and a high pH (12.5) which promotes growth of cementum and regeneration of periodontal ligament. MTA main content are calcium and phosphate ions, which are also the main constituents of the dental hard tissues, resembling the chemical composition of the tooth structure. The ability of MTA and Bioceramics to release Ca+ ions and their capacity to form hydroxyapatite are stated to be the factors responsible for its sealing ability, biocompatibility and dentinogenic activity. Biocompatible origin of MTA/Bioceramics, tendency to induce osteogenesis and cementogenesis make these materials suitable for root perforation repair resulting in a regeneration of periodontal attachment.

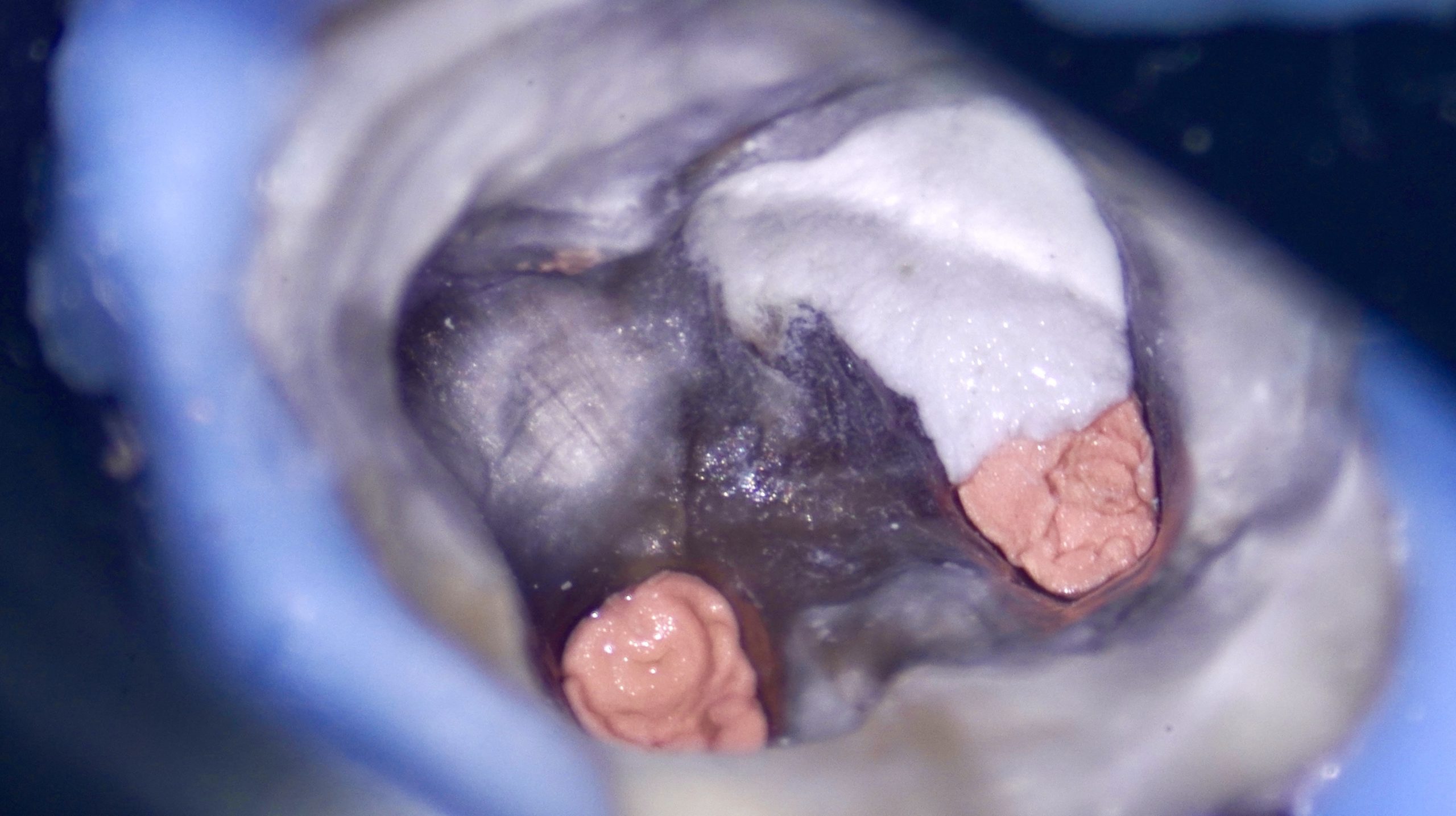
Fig. 1
A 32-year-old patient was referred to our dental office for endodontic re-treatment. Previously initiated treatment. History of a few endodontic interventions. 4.6 with old chipped MOD composite filling. Presence of the sinus tract on the buccal aspect. Diagnostic radiograph showed radiolucent lesion in periapical and furcal area (perforation suspected) of 4.6. Percussion painless, periodontal probing within normal limits. The Endodontic plan was to perform non-surgical root canal re-treatment with repair of the perforation with the use of MTA cement.
Initial appearance: Panoramic radiograph
Referred patient, V., 32 yo, female
4.6 Chronic Apical Abscess
Furcal Perforation
Sinus Tract
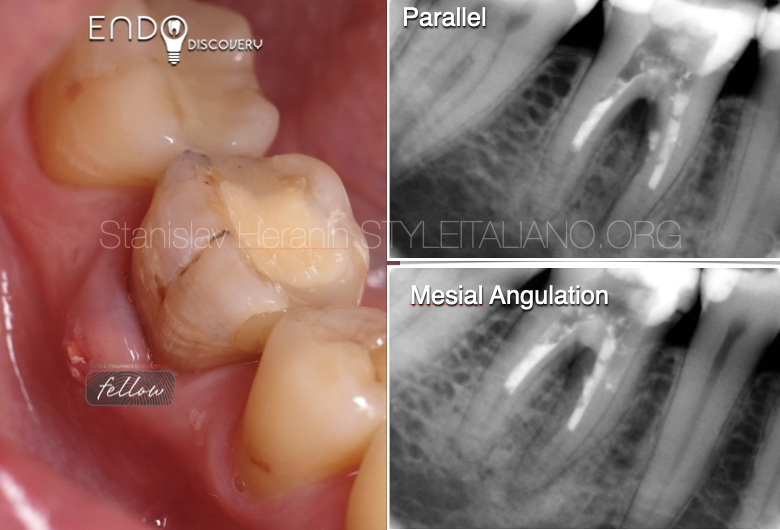
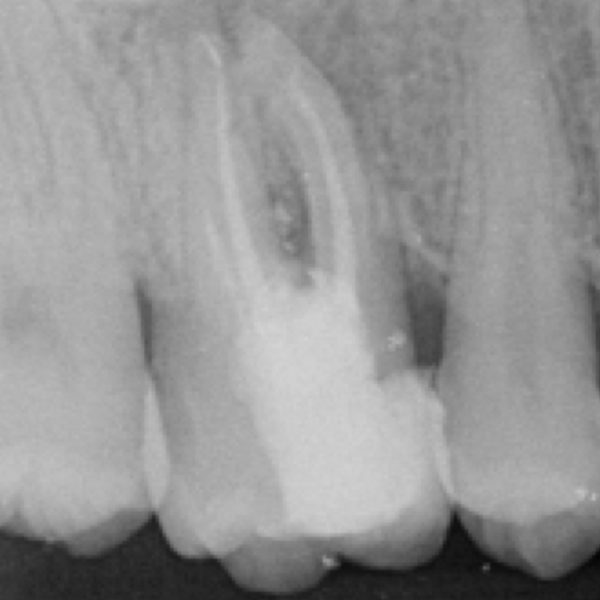
Fig. 2
Objective appearance
Diagnostic Periodical Radiographs
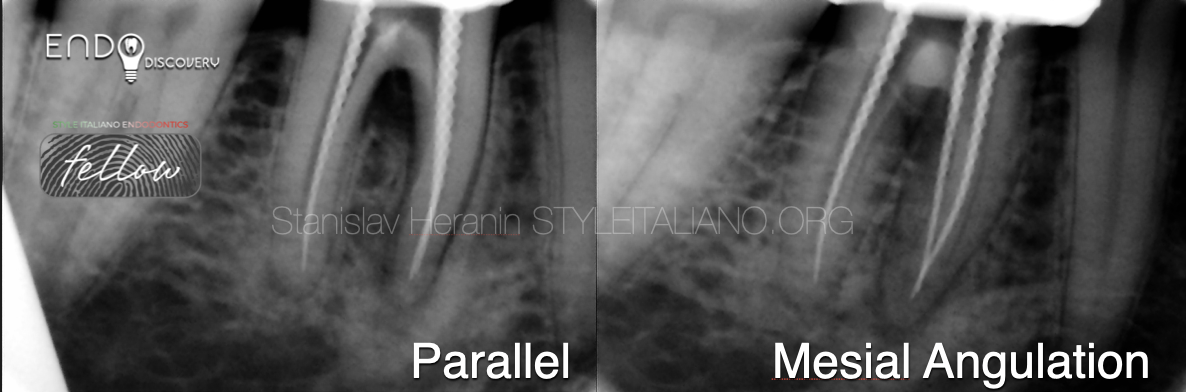
Fig. 3
1st appointment
Local Anesthesia, Isolation, Initial access, Desobturation, Gaining patency. Chemo-mechanical root canal preparation, MB/BL confluent, MAF 30.04, D - oval shape, MAF - 80.02. Pulpal floor perforation revealed next to MB orifice. Multiple irrigation with 5.25% sodium hypochlorite solution with ultrasonic agitation, finished with calcium hydroxide dressing for 10 days.

Fig. 4
2nd appointment
Asymptomatic. Sinus tract healing. Local Anesthesia, Isolation, Access, Copious Irrigation with 5.25% Sodium Hypochlorite, 17% EDTA + US agitation. Filling of root canals: MB/BL - continuous wave compaction, D - MTA plug. Perforation: periapical matrix (gelatin sponge), MTA plug.
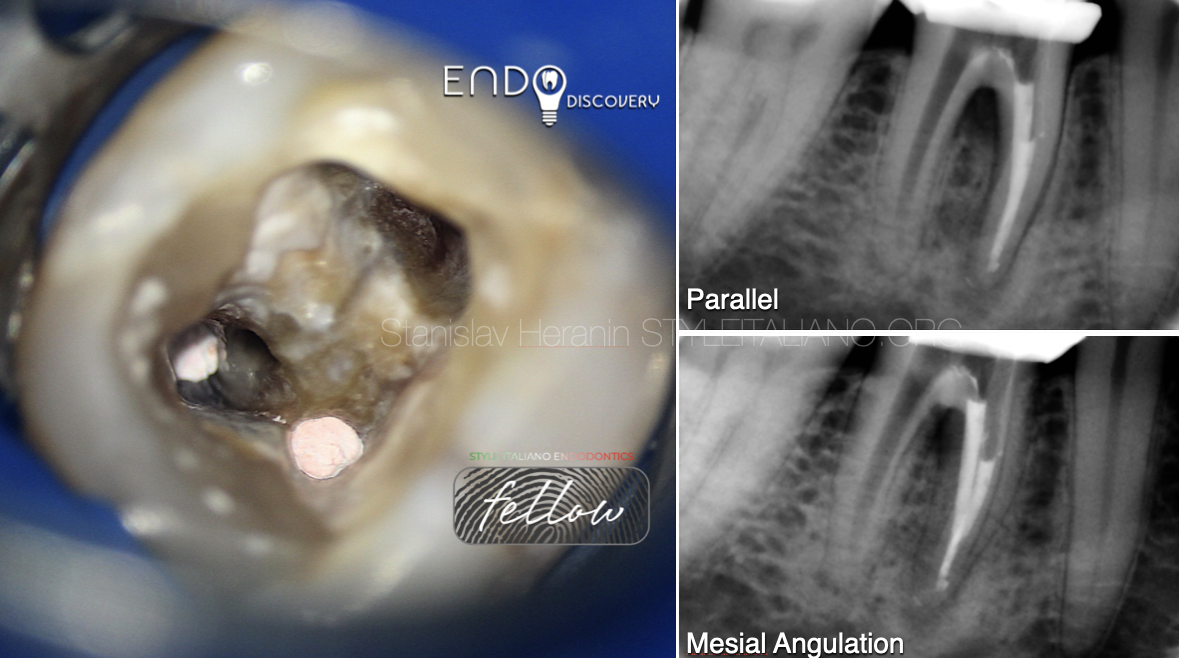
Fig. 5
2nd appointment
Root canal filling: MB/L - Continuous wave compaction
Radiographic control
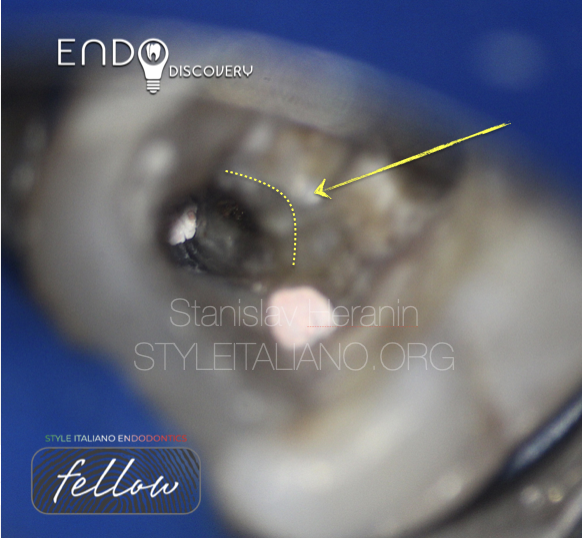
Fig. 6
2nd appointment
Perforation repair: Placement of periapical matrix (gelatin sponge)
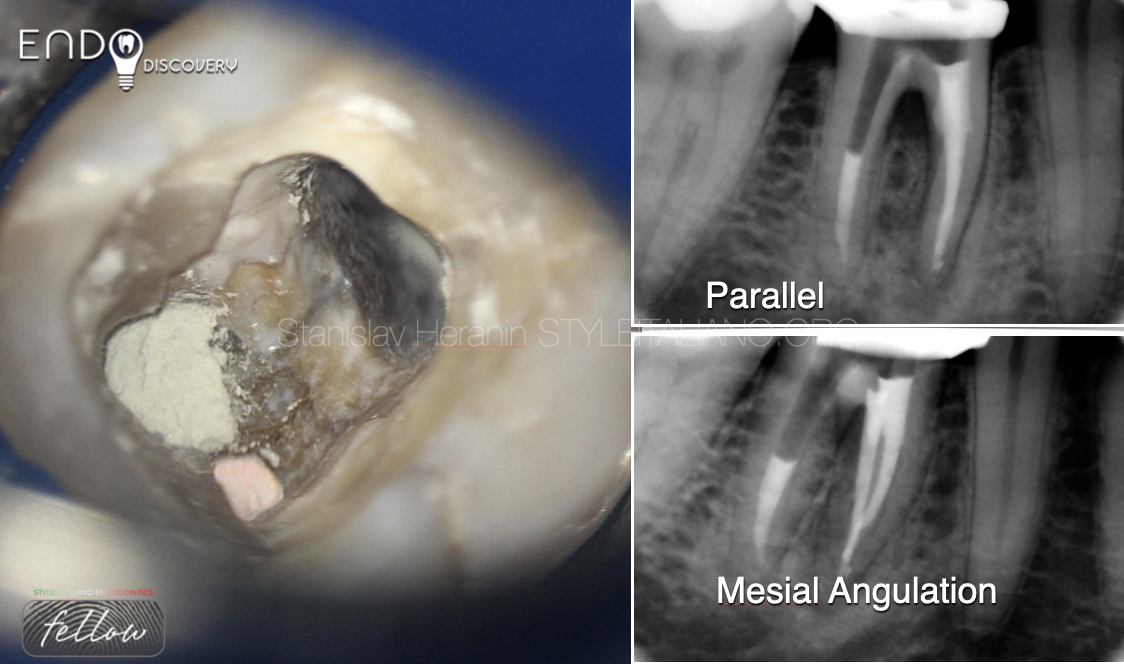
Fig. 7
2nd appointment
Perforation repair: Placement of MTA plug over perforation site
Distal canal: MTA plug
Radiographic control

Fig. 8
1,5 y recall: Complete healing of the periapical lesion and bone defect in perforation area

Fig. 9
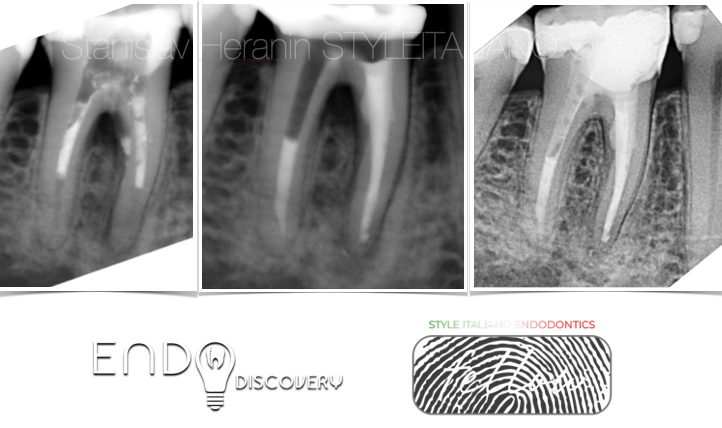
About the author:
Stanislav Heranin
1999: Graduated in Dentistry from the Ukrainian Medical Stomatological Academy - Faculty of Dentistry
1999-2001 - Postgraduate Education (UMSA)
2001-2012 - Professor Assistant - Department of Therapeutic Dentistry (UMSA)
2012-2019 - Professor Assistant - Department of Postgraduate Education of Dental Practitioners (UMSA)
2011: PhD in Dentistry (Ukrainian Medical Stomatological Academy)
2023 until now Associate Professor at The Department of Dentistry – School of Medicine - V.N.Karazin
Kharkiv National University
Private Dental Practice - Dental Centre “Machaon” (Poltava, Ukraine)
Founder of the Educational Centre EndoDiscovery
Past-President of the Ukrainian Academy of Esthetic Dentistry
Board Member of the Ukrainian Endodontic Association
Member of the Ukrainian Endodontic Society
Member of International Jury of Dental Restorative Contest ”Prisma-Championship”
Board member of the International Journal “Ukrainian Dental Journal”
Conclusions
Hydraulic Calcium Silicate Cements (MTA / Bioceramics) used as an apical barrier and perforation repair material are the primary materials of choice at present due to high biocompatibility and high sealing properties.
Bibliography
- Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod 2009;35:930–7
- Gorni FG, Gagliani MM. The outcome of endodontic retreatment: a 2-yr follow-up. J Endod. 2004 Jan;30(1):1-4. doi: 10.1097/00004770-200401000-00001. PMID: 14760899.
- Torabinejad M, Parirokh M, Dummer PMH. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part II: other clinical applications and complications. Int Endod J. 2018 Mar;51(3):284-317. doi: 10.1111/iej.12843. Epub 2017 Oct 11. PMID: 28846134.
- Castellucci A. The use of mineral trioxide aggregate in clinical and surgical endodontics. Dent Today. 2003 Mar;22(3):74-81. PMID: 12705015.
- Nazeer A, Nazir A, Manzoor SA, Khan MA, Shaukat Z, Saleem M, Sajid M, Kashif M. Efficacy of Mineral Trioxide Aggregate (MTA) as a Reparative Material in Iatrogenic Furcal Perforations in Mandibular Molars. Cureus. 2024 Jan 29;16(1):e53206. doi: 10.7759/cureus.53206. PMID: 38425600; PMCID: PMC10902626.Bains R, Bains VK, Loomba K, Verma K, Nasir A. Management of pulpal floor perforation and grade II Furcation involvement using mineral trioxide aggregate and platelet rich fibrin: A clinical report. Contemp Clin Dent. 2012 Sep;3(Suppl 2):S223-7. doi: 10.4103/0976-237X.101100. PMID: 23230369; PMCID: PMC3514927.
- Nagmode P, Janbandhu P, Jagtap A, Basatwar H, Godge S, Shinde S. A scanning electron microscopic study evaluating the sealing ability of MTA, BiodentineTM, and new light-cure MTA used for furcal perforation repair. J Clin Exp Dent. 2023 Jan 1;15(1):e32-e37. doi: 10.4317/jced.59755. PMID: 36755683; PMCID: PMC9899359.