Management of a perforating internal inflammatory root resorption in a maxillary central incisor
18/02/2021
Xavier-Fructuós Ruiz
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Internal root resorption is an inflammatory condition that produces the destruction of hard dental tissues. For the resorptive process to take place, two conditions have to occur simultaneously. First of all, predentine layer has to be damaged and expose the mineralized structures of the tooth to the osteoclastic cells and secondly, there is a need of partial vital and inflamed pulp to perpetuate the process. Osteoclasts are the responsible cells that start the resorption which progress until the whole pulp becomes necrotic.
Traumatic injuries, pulp inflammatory conditions, restorative procedures and orthodontic treatment are some of the predisposing factors related to internal inflammatory root resorption (IIRR). Its prevalence is reported in the literature as a very rare condition and they are often diagnosed during routine radiographic examinations due to their symptom-free characteristics. Therefore, IIRR sometimes can advance weakening the tooth structure and perforating the root canal space, when sometimes a sinus tract can be developed. Three-dimensional imaging modalities such as Cone-Beam Computed Tomography (CBCT) are required for a proper diagnosis and treatment decision making.
Root canal treatment is the indicated approach for teeth with IIRR. A good disinfection with sodium hypochlorite is essential to remove the granulomatous tissue present in the resorptive process. Calcium hydroxide has also been recommended in cases where bleeding can’ t be controlled. One of the main complications when facing those IIRR cases is root canal obturation due to the oval shape of the resorptive cavity. Warm gutta-percha obturation techniques have been suggested to achieve a good success. In cases where a perforation occurs, the use of bioceramic materials such as mineral trioxide aggregate (MTA) is indicated to seal the communication with the periodontal tissues due to their high biocompatibility.
The present case shows the management of a tooth with an IIRR that where a perforation was detected and where root canal treatment was performed sealing the root canal system and the resorptive process with MTA.

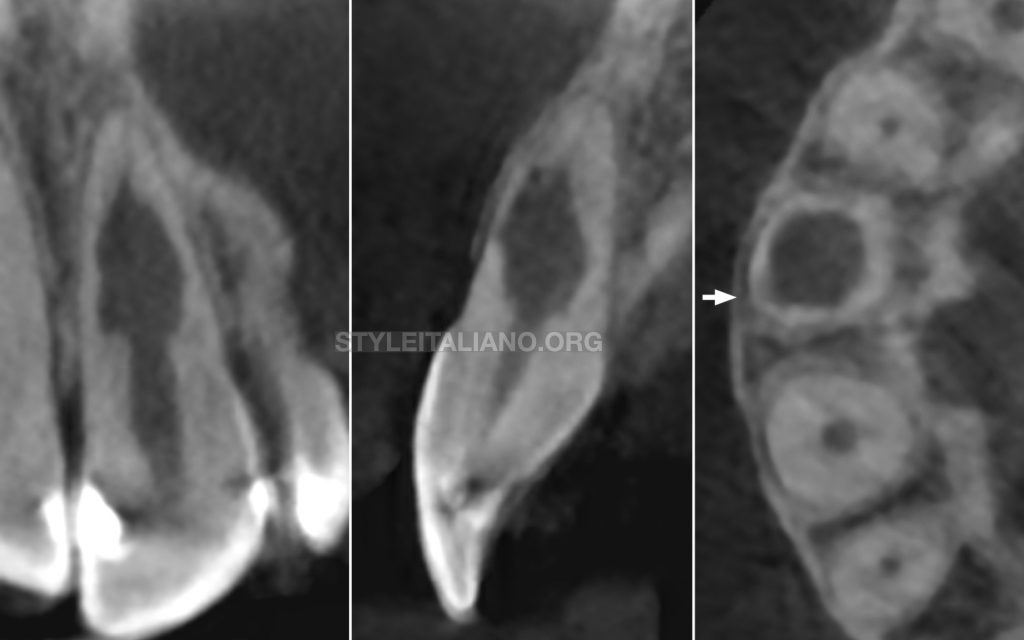
Fig. 1
Description of the case
A 42-year-old male patient came into the clinic because he noticed the presence of a bump at the gingival tissues above the left maxillary central incisor (Fig.A). Clinically, tooth 21 was asymptomatic to percussion and responded normally to pulp sensibility testing.
A digital periapical radiograph was performed (Fig.B) which showed the presence of a radiolucent oval widening of the root canal space in the middle third of the root. Taking into account the clinical and radiographic signs and symptoms the diagnosis was an internal inflammatory root resorption of tooth 21.
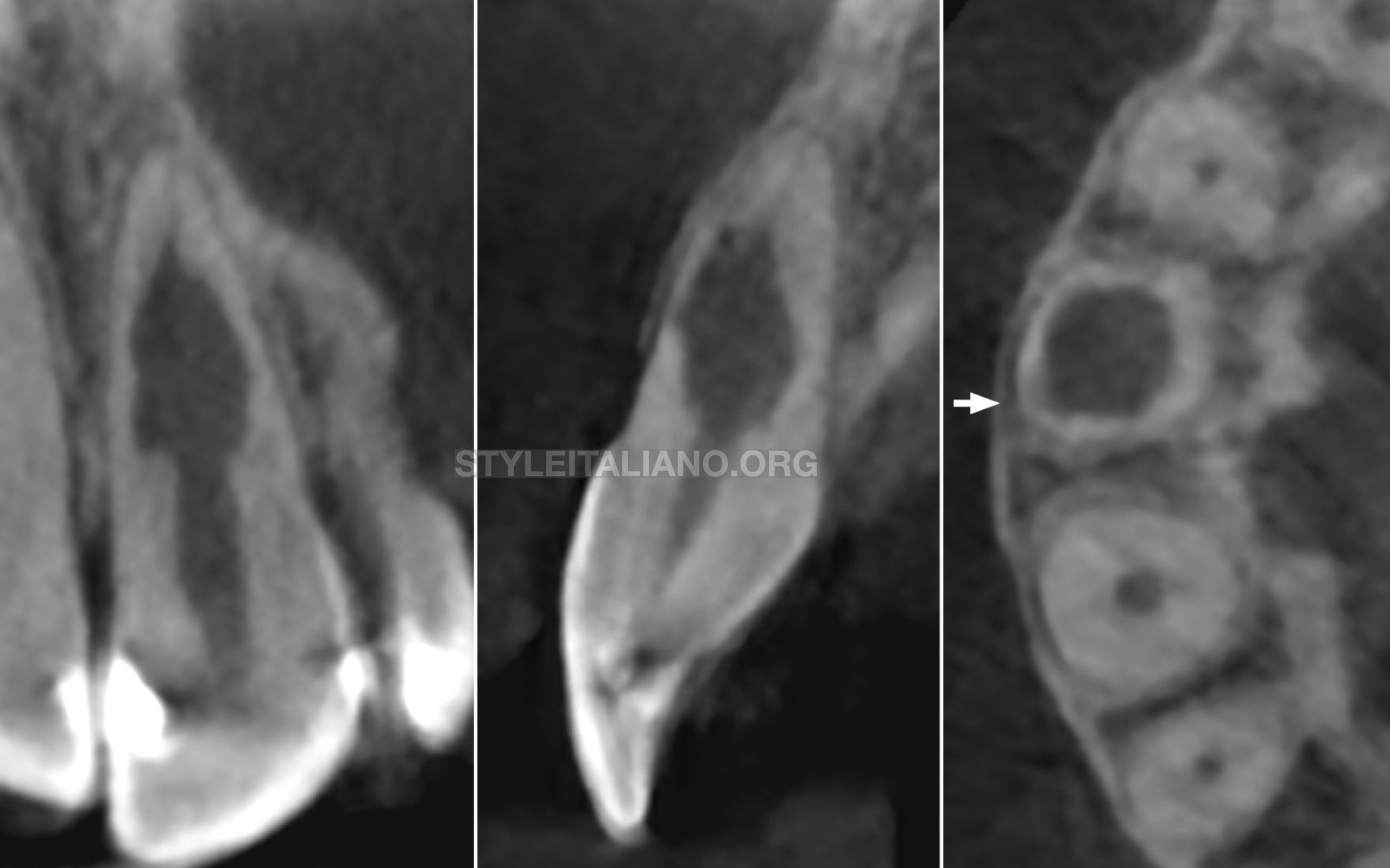
Fig. 2
A limited 5x5cm field of view CBCT scan was then performed. The CBCT slices confirmed the presence of an infracrestal communication (arrow) between the root canal space and the periodontal tissues. The final diagnosis was a perforating IIRR and patient was scheduled for root canal treatment.
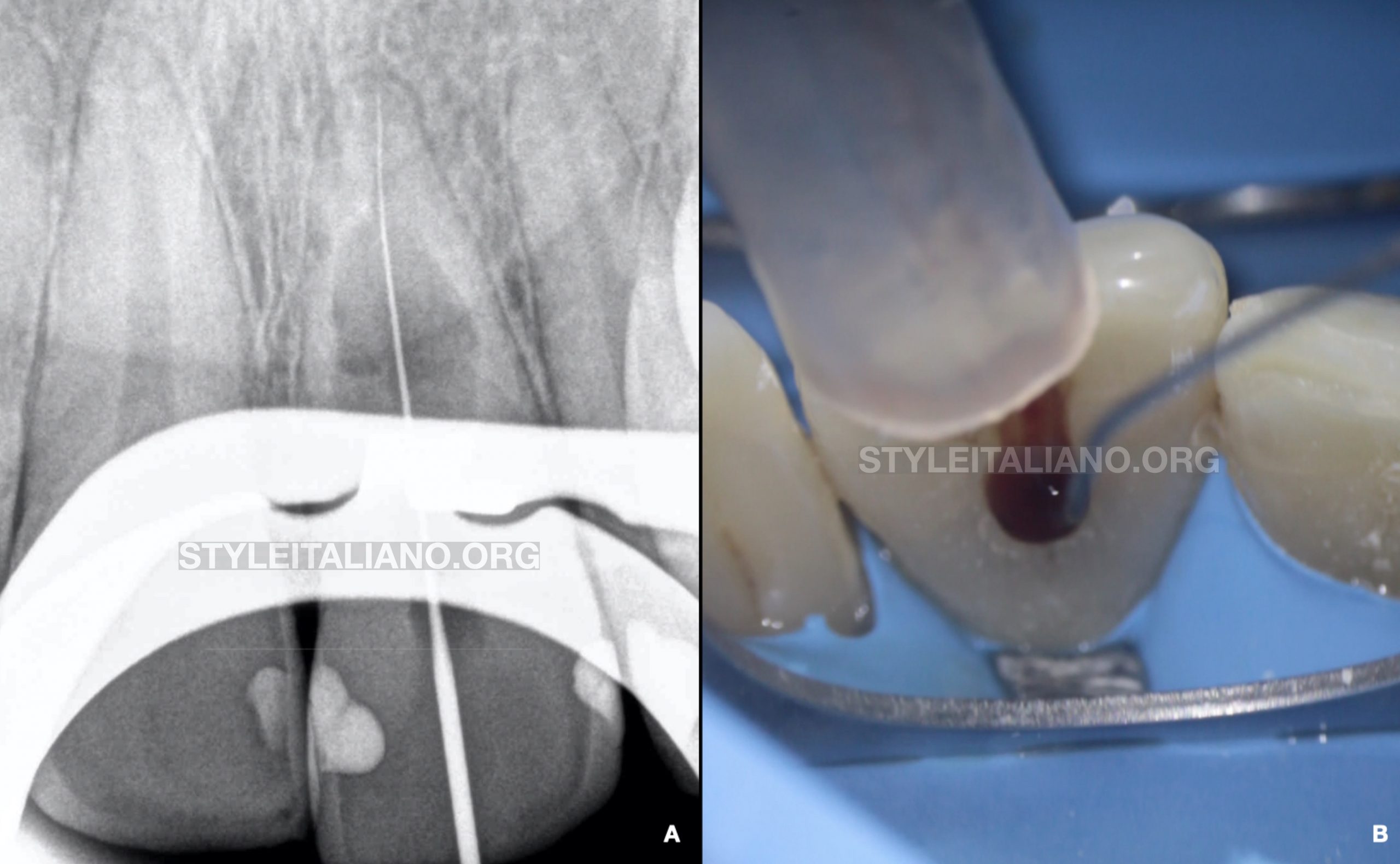
Fig. 3
Root canal treatment procedure: 1st appointment
After performing local anesthesia and under rubber dam isolation an access cavity was performed. Apical patency was achieved and working length was determined with a 10-K manual file (Fig.A). Profuse bleeding was observed due to high-vascular granulomatous tissue (Fig.B). Continuous irrigation was performed with sodium hypochlorite 4.25%. Mechanical instrumentation was performed with WaveOne Gold 25.07 (Dentsply Sirona, Ballaigues, Switzerland) and a calcium hydroxide-based paste was used due to the impossibility to control bleeding from the root canal space. A provisional obturation was then placed and the patient was given second appointment to finish the procedure.
Root canal treatment procedure: 2nd appointment
The next appointment was performed 2 weeks later. The sinus tract had disappeared. Provisional obturation was removed and profuse irrigation with sodium hypochlorite was performed.
Due to both the apical widening of the root canal space and the presence of the infracrestal perforation caused by the resorption, it was decided to perform the obturation with MTA. A Profile 60.04 was used to prepare the apical part. Final irrigation with sodium hypochlorite was performed and activated sonically with Endoactivator® (Dentsply Sirona, Ballaigues, Switzerland), which also helped to clean the remnants of granulomatous tissue from the resorptive process. Root canal was dried with paper points and an MTA plug was performed using a plugger and indirect ultrasonic vibration until 3mm under the cement-enamel junction. A bulk-fill composite was then used in the coronal third of the root canal space, and a flowable resin and a composite to seal the access cavity and perform the coronal restoration.
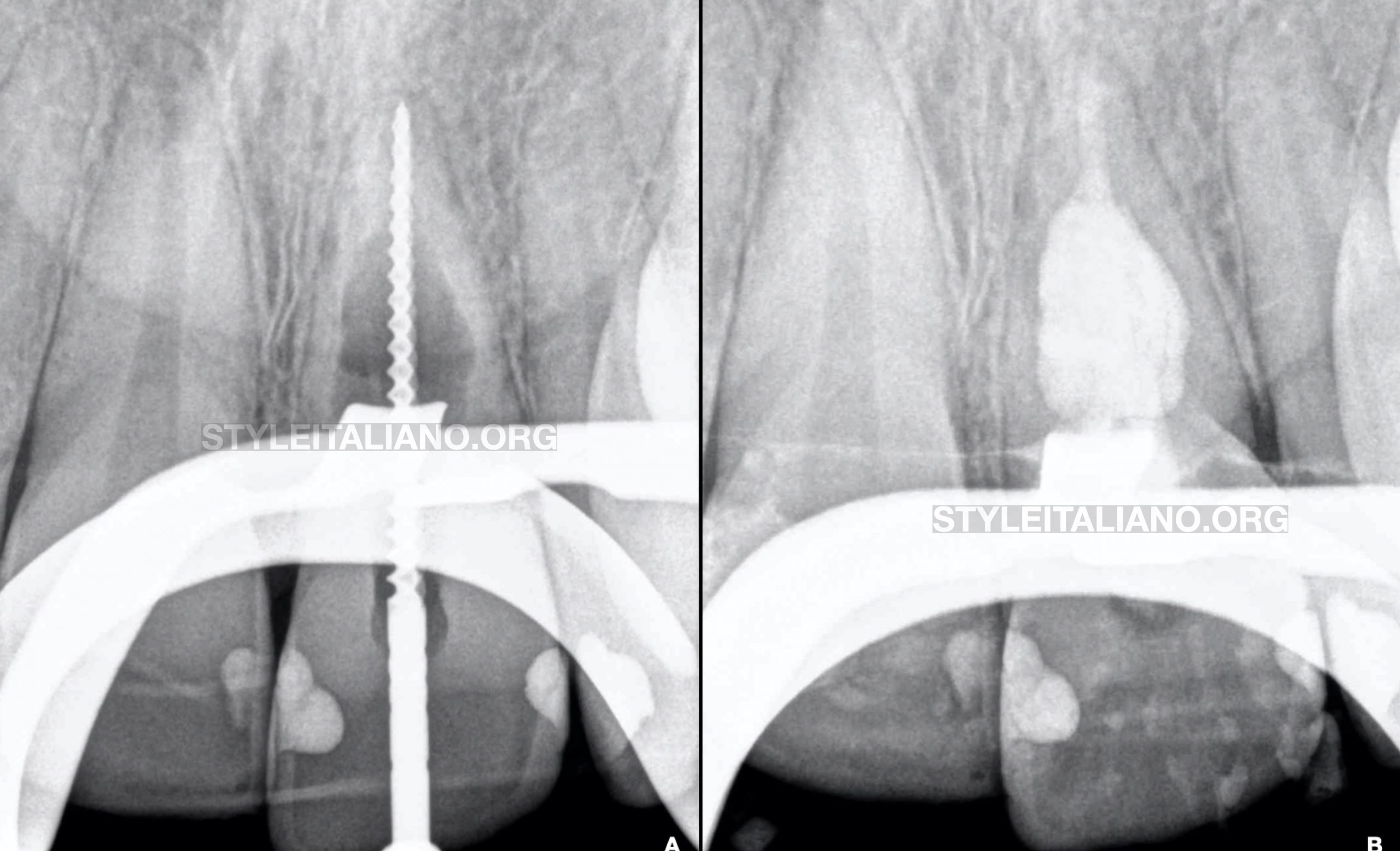
Fig. 4
Working length determination radiograph (Fig.A) after root canal preparation. Radiograph showing root canal and resorptive process obturation (Fig.B) with MTA.
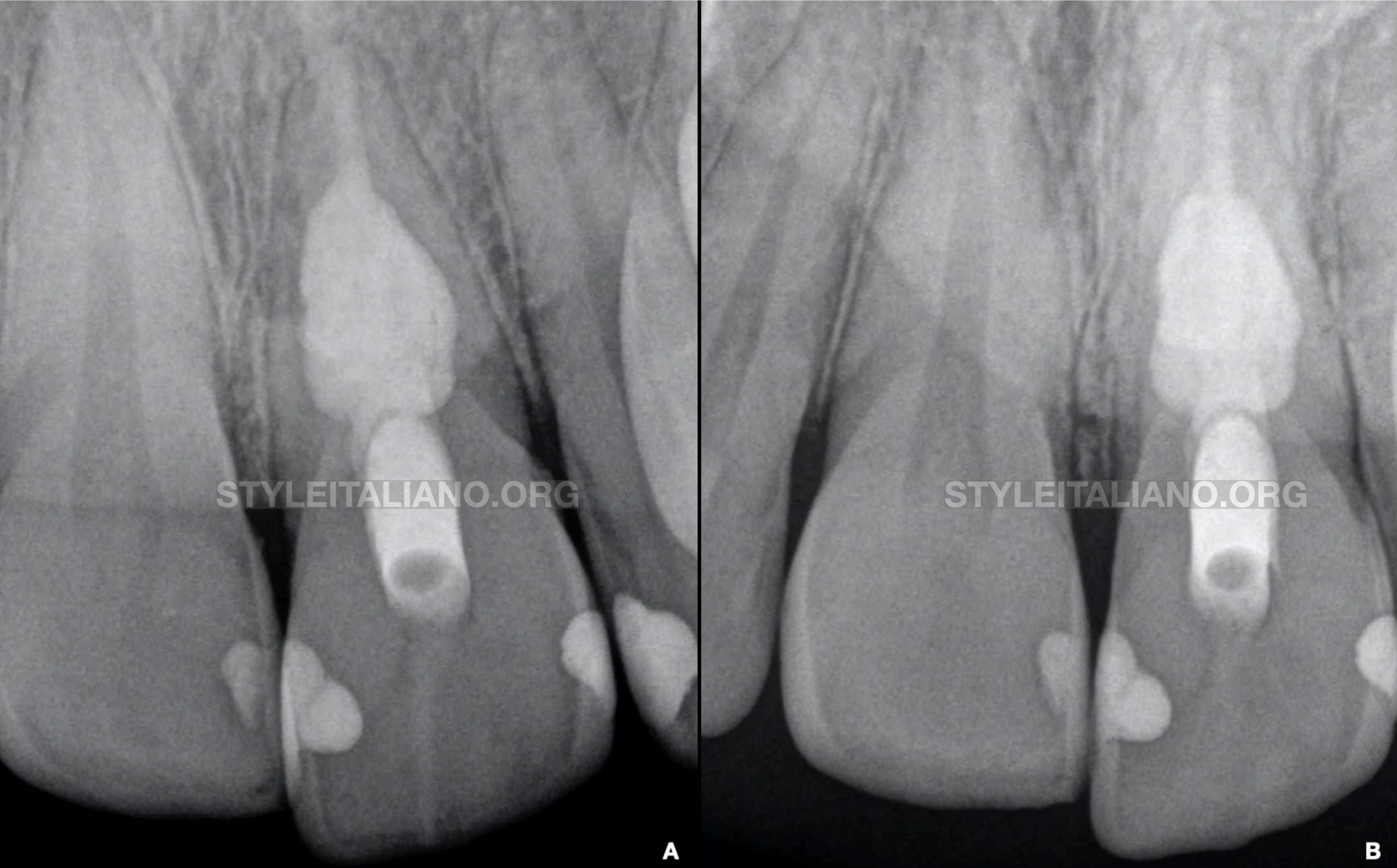
Fig. 5
Post-operative (Fig.A) and 1-year recall radiograph (Fig.B) showing healthy periapical tissues. The patient was asymptomatic and no discoloration was observed at follow-up.
Conclusions
Management of teeth with IIRR represent a great challenge for the clinicians, especially if those resorptions perforate the root canal system producing a communication with the periodontal tissues. A good diagnosis is mandatory and the use of CBCT is recommended to identify if those root resorptions are perforating or not.
Root canal treatment with a proper disinfection and thermoplastic gutta-percha obturation techniques to fill all the resorptive process is required to achieve success. In cases where a communication occurs, bioceramic materials and specifically MTA has been recommended for its repair. The main problem of MTA is that it produces tooth discoloration. Thus, it is recommended to place the material at least 3mm under the cement-enamel junction of the tooth or use a similar biocompatible material to avoid or minimize this drawback.
In conclusion the prognosis of teeth with internal root resorptions is good when a good diagnosis and management is performed, as it is showed in the present case.
Bibliography
1. Haapasalo M, Endal U. Internal inflammatory root resorption: the unknown resorp-tion of the tooth. Endod Topics 2006;14:60–79.
2. Patel S, Ricucci D, Durak C, Tay F. Internal root resorption: a review. J Endod. 2010;36:1107–21.
3. Patel S, Brown J, Semper M, Abella F, Mannocci F. European Society of Endodontology position statement: Use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by. Int Endod J. 2019;52:1675-1678
4. Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25:197–205.
5. Valles M, Mercade M, Duran-Sindreu F, Bourdelande JL, Roig M. Influence of light and oxygen on the color stability of five calcium silicate-based materials. J Endod. 2013;39:525–528.

