Invasive Cervical Resorption Part 2: Combined Non-surgical and surgical management
07/09/2020
Ahmed Shawky
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
For invasive cervical resorption to occur and propagate, there must be a damage in the periodontal ligament and cementum in addition to a contributing factor(s) which is assumed to sustain the osteoclastic activity. Although the etiology of ICR is poorly understood in literature and there might be some etiological factors which have not yet been identified, it seems that Traumatic dental injuries and orthodontic movements are the most common factors associated with ICR.
According the ESE position statement, the treatment plan for a tooth with ICR can be; Conservative non-surgical repair (see part1), Surgical repair +/- endodontic treatment, Intentional Replantation or extraction in non-restorable teeth.
This is the second part of three articles aiming to present a case with trauma-induced invasive cervical resorption in which management was performed using a combined approach of Non-surgical and surgical treatments.

Fig. 1
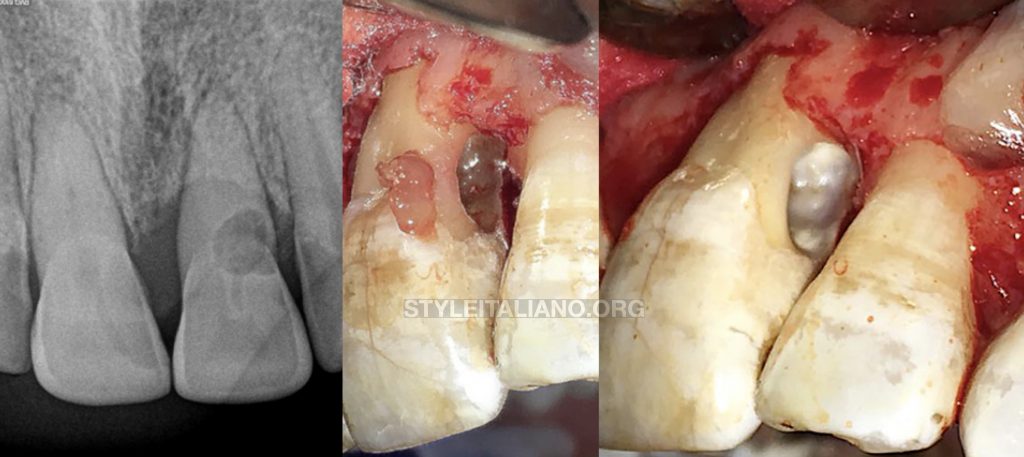
Figure 1: Pre-operative Assessment:
[A] Preoperative clinical image showing discolored maxillary central incisors and inflammation of the interdental papilla distal to the left central incisor (red arrow).
[B] Preoperative radiographic image showing PCO [Pulp Canal Obliteration] of both maxillary central incisors. The left incisor showing large invasive cervical resorptive defect. Both teeth showing apical periodontitis.
Periodontal examination revealed deep probing defects on the mesial and dial aspects of the resorbed left central incisor

Fig. 2
Figure 2: [A] Non-surgical treatment of the involved tooth:
Intra-operative radiographic image showing pre-surgical management of calcification in the maxillary left central incisor using D-finders and flare files. [B] Intra-operative radiographic image showing shaping confirmation during pre-surgical management of calcification in the maxillary left central incisor in which the instrumentation procedures have been completed using wave one gold [Large] files. [C] Intra-surgical radiographic image showing cone fit in the maxillary right central incisor in which the instrumentation procedures have been completed using wave one gold [Large] files. Cone fit and obturation were delayed to the surgical phase of the treatment plan [D] Intra-surgical clinical image showing cone fit in the maxillary right central incisor in which the instrumentation procedures have been completed using wave one gold [Large] files.
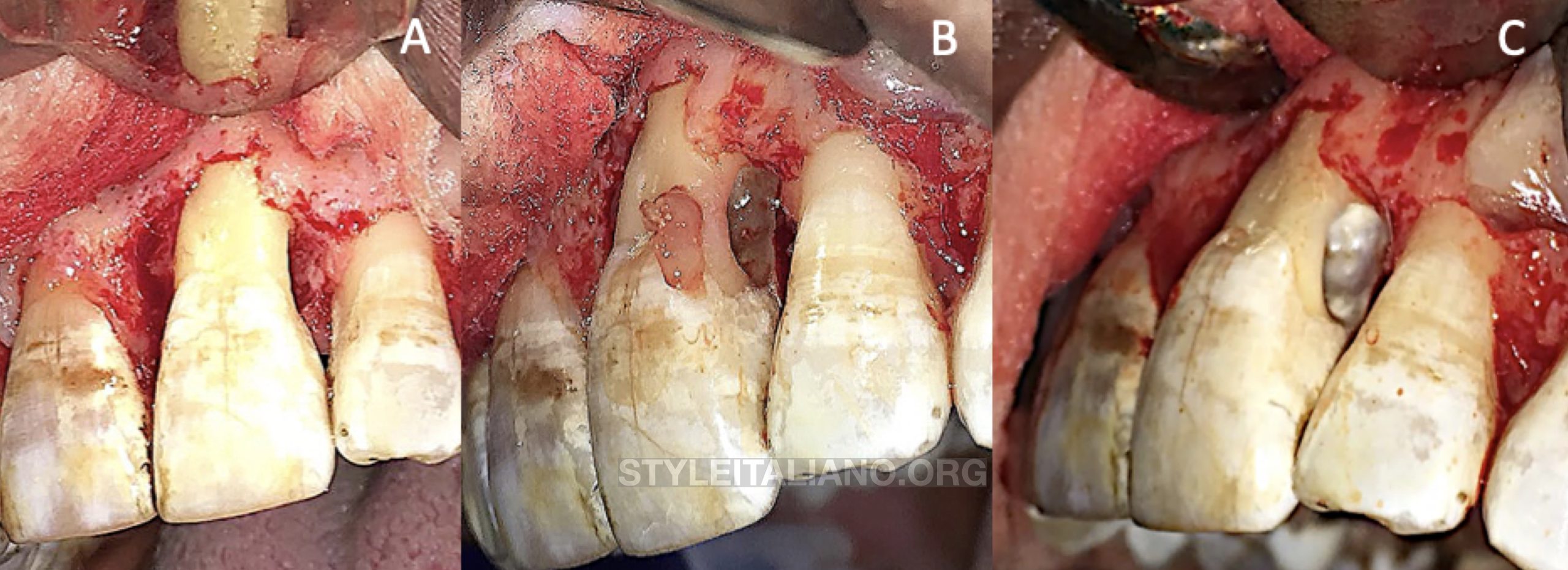
Fig. 3
Figure 3: Surgical Management of External Cervical Invasive Resorption.
[A] Intra-surgical clinical image showing surgical exposure of the defect using an intra-sulcular incision. [B] Intra-surgical clinical image showing excavation of the resorptive tissues within the defect. [C] Intra-surgical clinical image showing debridement of the resorptive defect after using ultrasonics.
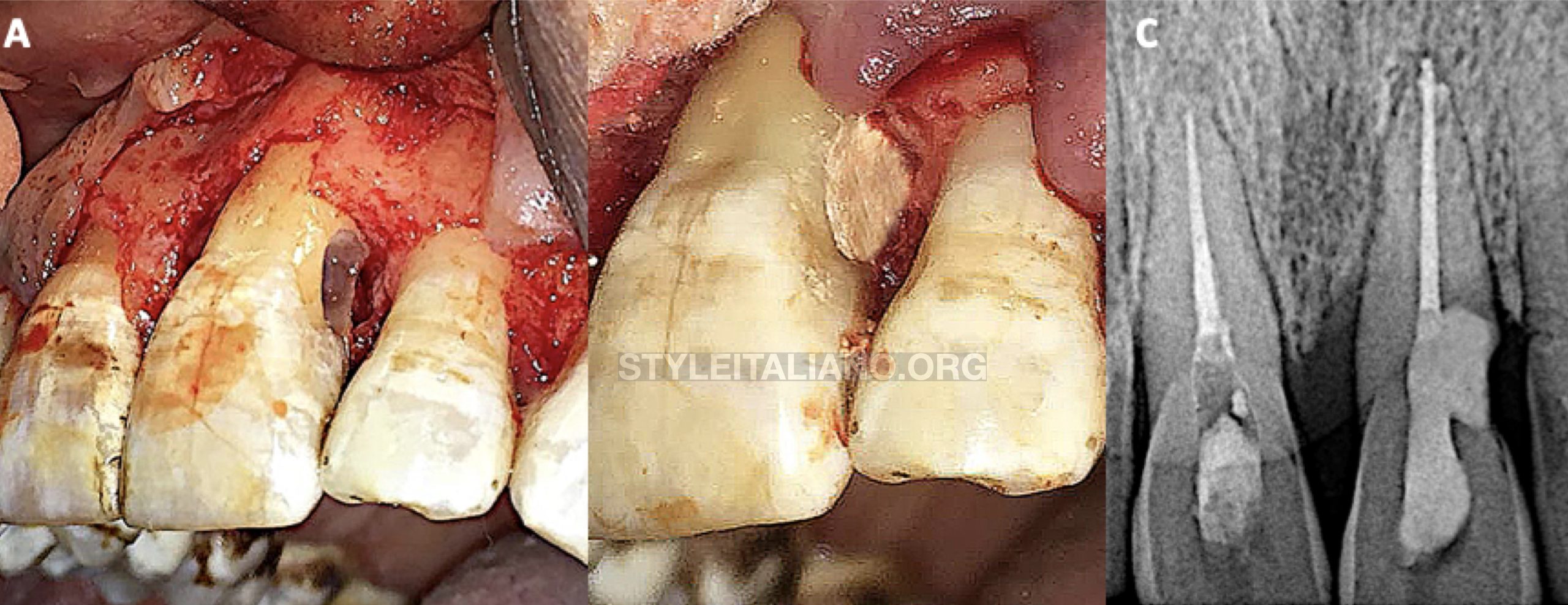
Fig. 4
Figure 4: Repair of Invasive cervical resorption using Calcium silicate material.
[A] Intra-surgical clinical image showing the cleaned defect after chemical debridement of the resorptive defect using 90% trichloroacetic acid [tissues have been isolated and protected using glycerol gel]. [B] Intra-surgical clinical image showing filling the resorptive defect using Biodentine [Septodont, France]. [C] Post-operative radiographic image showing obturation of both incisors and repair of the resorptive defect using Biodentine (Note the perfect adaptation of biodentine to the margins of the resorptive cavity). The patient was instructed and trained to maintain adequate hygiene measures with special concern given to the repaired incisor.

Fig. 5
Figure 5: One Year follow up:
One year later the patient attended for clinical and radiographic assessment. The patient reported adequate function without excessive stresses on the previously resorbed incisor as well as absence of signs and symptoms completely.
Upon radiographic evaluation, both teeth showed radiographic signs of healing (uniform thickness of periodontal membrane space, healing of apical periodontitis). It was a rewarding outcome to see the alveolar crest distal to the pre piously resorbed incisor growing and kissing the repair material.
Also, there was an improvement in the probing depth mesial to the previously resorbed incisor
Conclusions
- Traumatic Dental Injuries, especially major luxations, bears the risk of causing multiple complications especially pulp canal obliteration (due to alteration of the blood supply) or invasive cervical resorption (as a result of intense periodontal damage)
- Invasive cervical resorption involving the pulp requires combined approach in treatment involving both non-surgical and surgical managements.
- The use of calcium silicate based materials in repair of resorptive lesions enhances sealing of these defects as well as promoting fast restoration of the periodontal structures
Bibliography
1- Patel S, Foschi F, Condon R, Pimentel T, Bhuva B. External cervical resorption: part 2 – management. Int Endod J. 2018;51(11):1224-1238.
2-Heithersay GS. Invasive cervical resorption. Endod Top. 2004;7(1):73-92.
3- Patel, S, Lambrechts, P, Shemesh, H, Mavridou, A. European Society of Endodontology position statement: External Cervical Resorption. International Endodontic Journal, 51, 1323– 1326, 2018.



