Treatment of obliterated root canals using Guided Endodontic technique. A case report
09/02/2023
Massimo Giovarruscio
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
This article reports on an Endodontic treatment of obliterated teeth using a static guided endodontic (GE) technique. The aim is to demonstrate the benefits and limits of static guided endodontics.
The process of canal obliteration (CO) is characterized by the apposition of secondary or tertiary dentin, resulting in loss of volume in the pulpal space.
Canal Obliteration can result from various causes:
Pathological: trauma, decays, iatrogenic factors (bulky restorations or orthodontic movements) or occlusal overload.
Physiological: age-related. 4% of the population is affected by CO. In the event of trauma, the incidence reaches 22%
Root canal obliteration is considered to be a defence mechanism of the pulp, the vitality of which is often preserved. Esthetically, this usually leads to yellowish discolouration, which can be treated by external whitening and/or by placing a veneer. Endodontic treatment is only indicated when the canal obliteration is associated with radiological signs revealing a periapical lesion or clinical signs of irreversible pulpitis. This clinical situation poses a challenge for the practitioner. Even using a microscope, the risk of intra-operative error is very high.

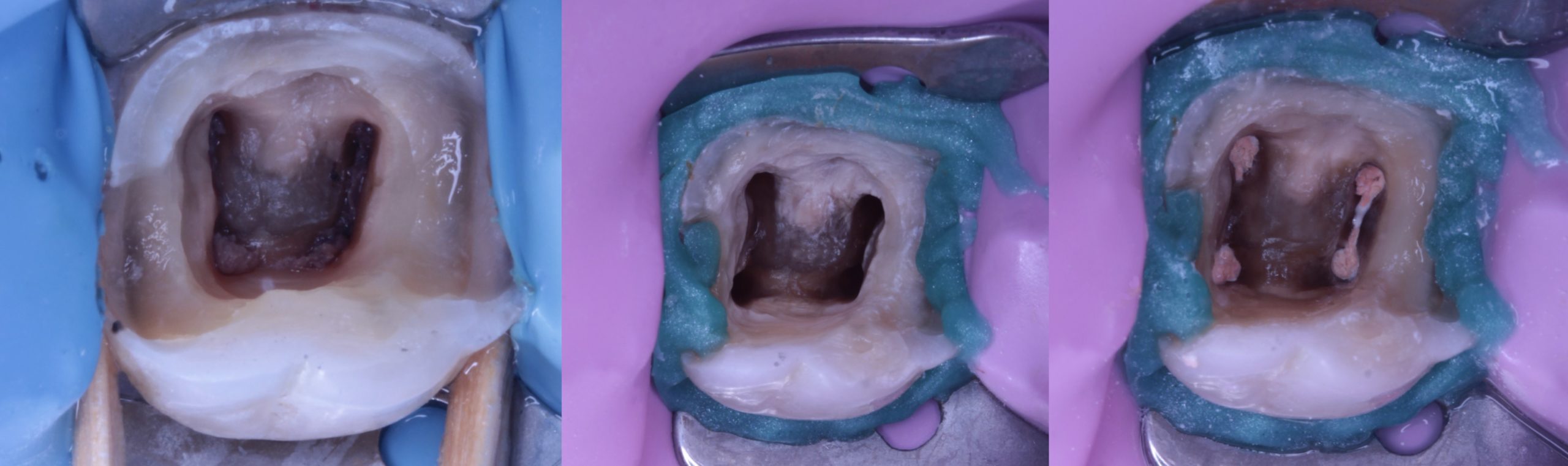
Fig. 1
A new approach to access cavity preparation was described for the first time in 2013 by Kfir et al. for the treatment of a type 3 dens invaginatus using an endodontic guide. For this purpose, they segmented the dental structure by means of CBCT to achieve a resin 3D model of the tooth. The model served to plan and manufacture a resin guide. As a result, a drill could be guided towards the invagination to be treated while preserving pulpal vitality of the tooth.
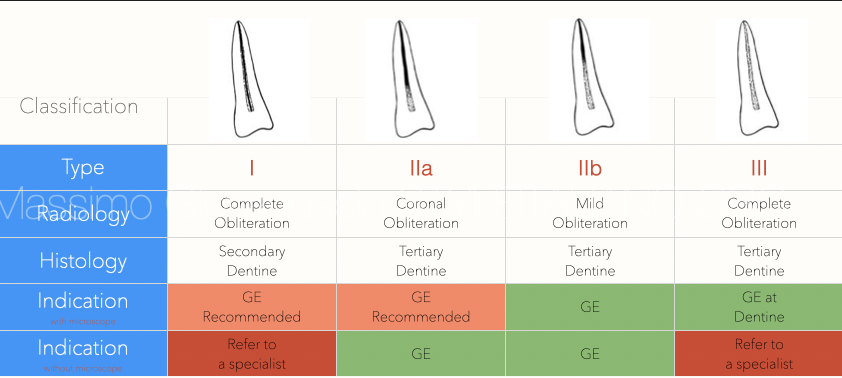
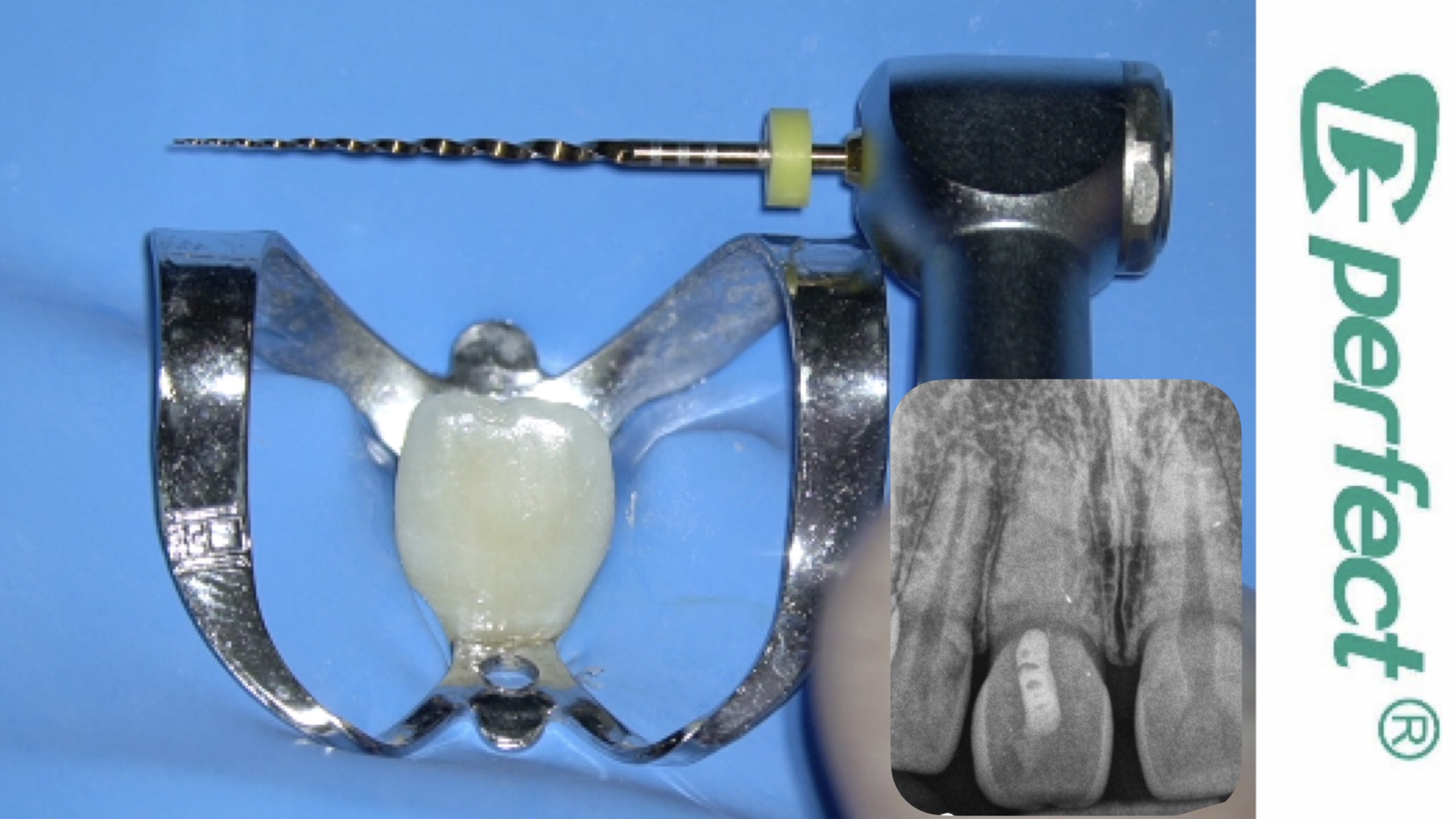
Fig. 2
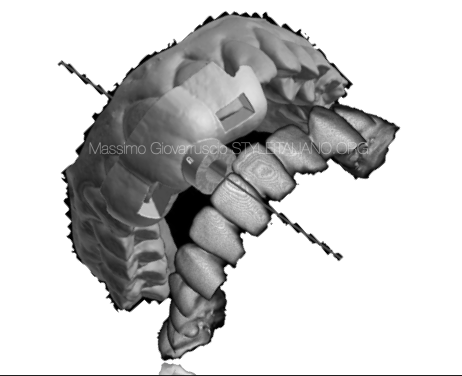
Van der Meer et al. suggested a digital planning protocol for endodontic use inspired by implantology protocols. They merged a DICOM file obtained by CBCT with a Standard Tessellation Language (STL) file obtained from an intraoral optical impression. They calculated the drilling axis with the aid of an implant planning software and created a virtual guide. The virtual guide was then downloaded as an STL file to print a resin guide by means of a 3D printer. The guide enabled the drill to be centred towards the canal of an obliterated tooth. Such planning of the access cavity made it possible to preserve the dental structure and avoid deviations that may jeopardize tooth prognosis. Static Guided Endodontics (GE) was then made simpler by using a single software program combining all the stages of the planning process, from visualization of the STL and DICOM files, to design the static guide and then printing the guide in resin materials. Some authors have applied this technique in cases involving maxillary and mandibular incisor and molar root canal obliteration, as well as for removal of fiber-reinforced posts. In this article, a clinical case was described involving the use of an endodontic static guide to perform endodontic treatment in an upper calcified root canal incisor.

Fig. 3
A 35-year-old female patient was referred following sclerosed canal on the upper right incisor (tooth 11). She reported a trauma which had occurred 15 years before. The tooth presented with yellowish discoloration, was painful to percussion and reported a negative response to electric and thermal sensitivity tests.
This finding was confirmed by CBCT taken (VGI, Evo NewTom) with a 55 mm scan field of view and 100-micron resolution. The patient’s informed consent was obtained to perform orthograde treatment by Guided Endodontics.

Fig. 4
The STL file of the arch was obtained by optical impression and uploaded to the BlueSky Plan software (BlueSkyBio; LLC; Grayslake; IL; USA) The aim was to superimpose the digital image of the arch on the CBCT views. Merging of the two files was achieved by means of fixed reference points on the crown surface of all the teeth of the full arch.
In this way, the inner surface of the guide can be modeled depending on the digital impression. The sleeve slot was realised according to the position of the drill simulated on the DICOM images.

Fig. 5
Planning the guide.
The guide was designed using BlueSkyPlan freeware. The bur was designed and planned on the DICOM file and oriented to ensure correct endodontic access to the calcified canal.
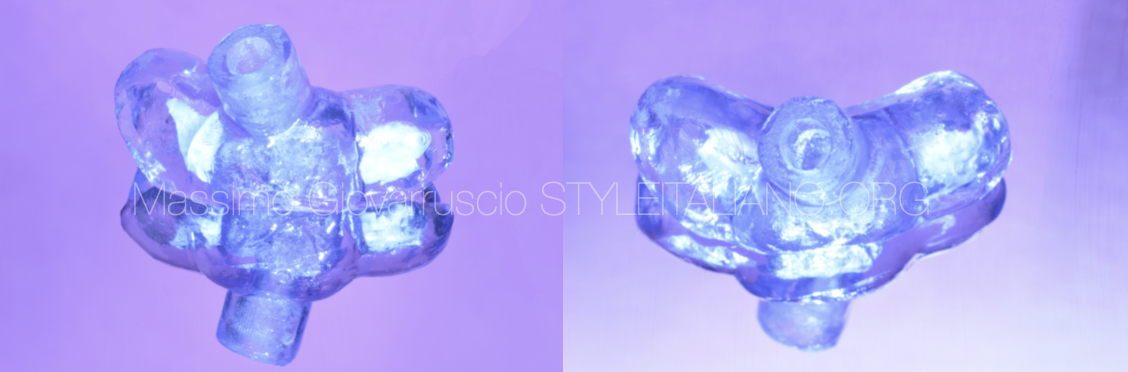
Fig. 6
The STL file for the guide was then downloaded and dispatched for 3D printing. The guide was printed in resin using a Formlabs 2 printer (Formlabs Inc; Sommerville; MA; USA).

Fig. 7
These planning specifications correspond to the drill (0.75 mm diameter) and its guide sleeve (0.75 mm inner diameter and 3.50 mm outer diameter; 5 mm length).
In fact, the metal sleeve was then inserted under friction into the resin guide to orient a drill 0.75 mm in diameter and 23 mm in length (FFDM Pneumat Tivoly; Bourges; France)
A 0.75 mm diameter drill was utilised to minimise tooth removal during the drilling procedure.

Fig. 8
Recapitulation of the different steps of the 3D planning procedure of the directional guide

Fig. 9
During the clinical appointment the operative field was isolated using a rubber dam placed on several teeth to avoid interference between the guide and the clamp. The drill, mounted on a low-speed contra-angle, was inserted into the sleeve, then rotated at 20,000 RPM. The guide was kept very stable by the clinician during drilling. At every millimeter of progress along the canal, the guide was withdrawn to allow the access cavity to be irrigated. The irrigation avoids overheating of the dentine and accumulation of dentine debris.

Fig. 10
A staggered drilling pattern was performed. At every millimeter progress along the canal, the guide was withdraw to allow irrigation to the access cavity and avoid overtaking of the dentin and accumulation of dentin debris.
The guide and the handpiece must be firmly held with the fingers, otherwise the guide and the handpiece could be moved and displaced.
The straight-line penetration of the drill was checked with a stiff pencil lead of a similar diameter (0.70 mm).
We perform a stagger drilling pattern, stopping and removing the guide after 2-3 mm of progress to verify the patency and rinse the canal to avoid clogging it with debris and overheating of the dentin

Fig. 11
An intraoperative radiograph was taken to confirm the correct trajectory during the treatment. Once the drill was fully inserted into the sleeve, patency and working length
was checked by use of a C-Pilot 10 file and Electronic Apex Locator.

Fig. 12
The endodontic treatment was normally completed. An intraoperative X-Ray has been taken with the C-Pilot 10 file to confirm a working length. Shaping was performed using Primary WaveOne Gold System.
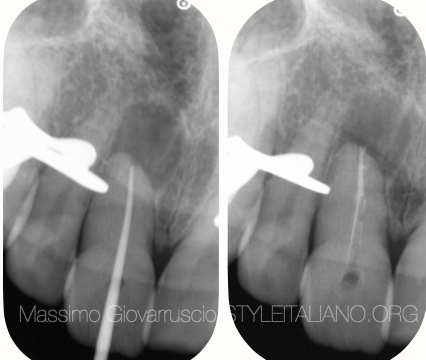
Fig. 13
The Endodontics treatment is performed following the standard procedure.
In this case the canal has been shaped using WaveOne Gold Primary reciprocation file.
The irrigation consisted of a sodium hypochlorite 5,75% solution and EDTA 17% solution.
The canal has been obturated with GP and Warm Vertical Compaction.

Fig. 14
The small access cavity has been restored permanently using a direct composite material.

Fig. 15
Pre, intra and post operative situation
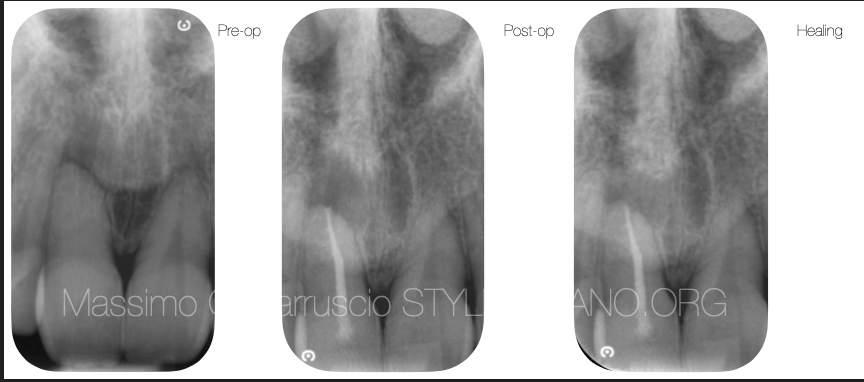
Fig. 16
Pre operative, post operative and follow up X-rays
Conclusions
The treatment of obliterated root canals using Guided Endodontic technique, examined in this article, is a safe and efficient method to access a calcified root canal and preserving tooth structure. This is a straight-forward technique which can be employed by most dentists. Validation studies on patients are needed to evaluate clinical benefits of this use of guided technique.
Bibliography
Bordone, A., & Cauvrechel , C. (2020). Treatment of obliterated root canals using various guided endodontic techniques: a case series. Giornale Italiano Di Endodonzia, 34(1). https://doi.org/10.32067/GIE.2020.34.01.06
Perez C, Finelle G, Couvrechel C. Optimisation of a guided endodontics protocol for removal of fibre-reinforced posts. Aust Endod J. 2020 Apr;46(1):107-114. doi: 10.1111/aej.12379. Epub 2019 Oct 11. PMID: 31603599.
Ishak G, Habib M, Tohme H, Patel S, Bordone A, Perez C, Zogheib C. Guided Endodontic Treatment of Calcified Lower Incisors: A Case Report. Dent J (Basel). 2020 Jul 8;8(3):74. doi: 10.3390/dj8030074. PMID: 32650552; PMCID: PMC7558261.
Moreno-Rabié C, Torres A, Lambrechts P, Jacobs R. Clinical applications, accuracy and limitations of guided endodontics: a systematic review. Int Endod J. 2020 Feb;53(2):214-231. doi: 10.1111/iej.13216. Epub 2019 Oct 23. PMID: 31520416.
Torres A, Shaheen E, Lambrechts P, Politis C, Jacobs R. Microguided Endodontics: a case report of a maxillary lateral incisor with pulp canal obliteration and apical periodontitis. Int Endod J. 2019 Apr;52(4):540-549. doi: 10.1111/iej.13031. Epub 2018 Nov 8. PMID: 30341776.
Zehnder MS, Connert T, Weiger R, Krastl G, Kühl S. Guided endodontics: accuracy of a novel method for guided access cavity preparation and root canal location. Int Endod J. 2016 Oct;49(10):966-72. doi: 10.1111/iej.12544. Epub 2015 Oct 3. PMID: 26353942.
Gambarini G, Galli M, Morese A, Abduljabbar F, Seracchiani M, Stefanelli LV, Giovarruscio M, Di Nardo D, Testarelli L. Digital Design of Minimally Invasive Endodontic Access Cavity Appl. Sci. 2020, 10, 3513; doi:10.3390/app10103513