Three Years Follow-up of Large Lesion Treated With MTA Apical Plug
15/11/2020
Ahmed Alwaidh
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
The goal of Endodontic treatment is to cure or prevent apical periodontitis (Ørstavik & Pitt Ford 2008). Endodontic treatment does not end when the root canal being filled, but when having favourable outcomes of the treatment upon reviewing (Reit 1986), which can be achieved by the infection control management through the root canal procedure (Basrani & Haapasalo 2012). Non-surgical root canal treatment is a procedure with a high long term prognosis if we have a proper diagnosis, treatment plan, and accurate execution of the procedure with a systematic approach.

Fig. 1
A 28 years old female presented complaining of a discolored maxillary left central incisor (UL1). History of trauma 12 years ago. The patient’s chief complain was the discolored UL1 with ugly restoration, as she reported no history of pain nor discomfort.

Fig. 2
On clinical examination, UL1 had negative response to cold test, no tenderness to percussion, no tenderness to palpation on buccal gingiva, and no mobility. While UR1 and UL2 responded normally to cold test.

Fig. 3
From palatal view, the gingiva around UL1 was little swollen with deep probing. There was clinical evidence of pin underneath the composite restoration

Fig. 4
Pre-operative IOPA (intra-oral peri-apical) radiograph revealed large peri-apical lesion around the apices of UL1 and UL2. But according to the clinical examination, UL2 was with clinically normal pulp as it responded normally to cold test.
Diagnosis: UL1 was diagnosed as necrotic tooth with asymptomatic apical periodontitis (AAP).
Treatment plan:
- 1. NSRCT (non-surgical root canal treatment).
- 2. Internal bleaching.
- 3. Restore the tooth aesthetic by direct composite restoration.
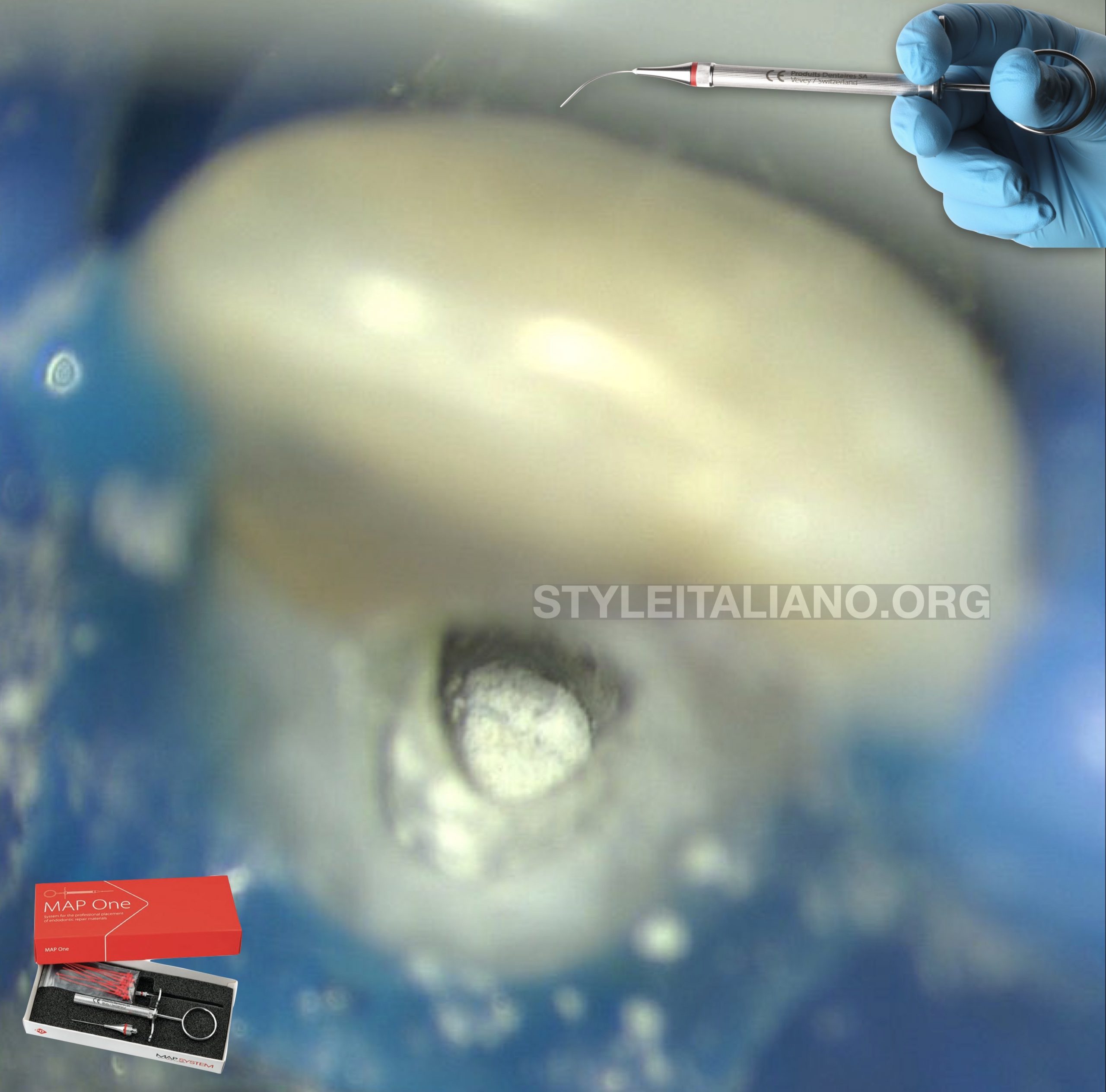
Fig. 5
Endodontics treatment was conducted on two visits.
After access opening, the canal was already wide so there was no instrumentation.
Chemical debridement was conducted with NaOCl 5.25%, EDTA 17%, activated by passive ultrasonic irrigation (PUI).
Apical gauge was measured size #70.
With the use of MAP System (Produits Dentaires SA), it was easy to deliver MTA apical plug.

Fig. 6
8 mm of MTA apical plug was delivered with the use of MAP System and condensed using the flexible Fanta Pluggers
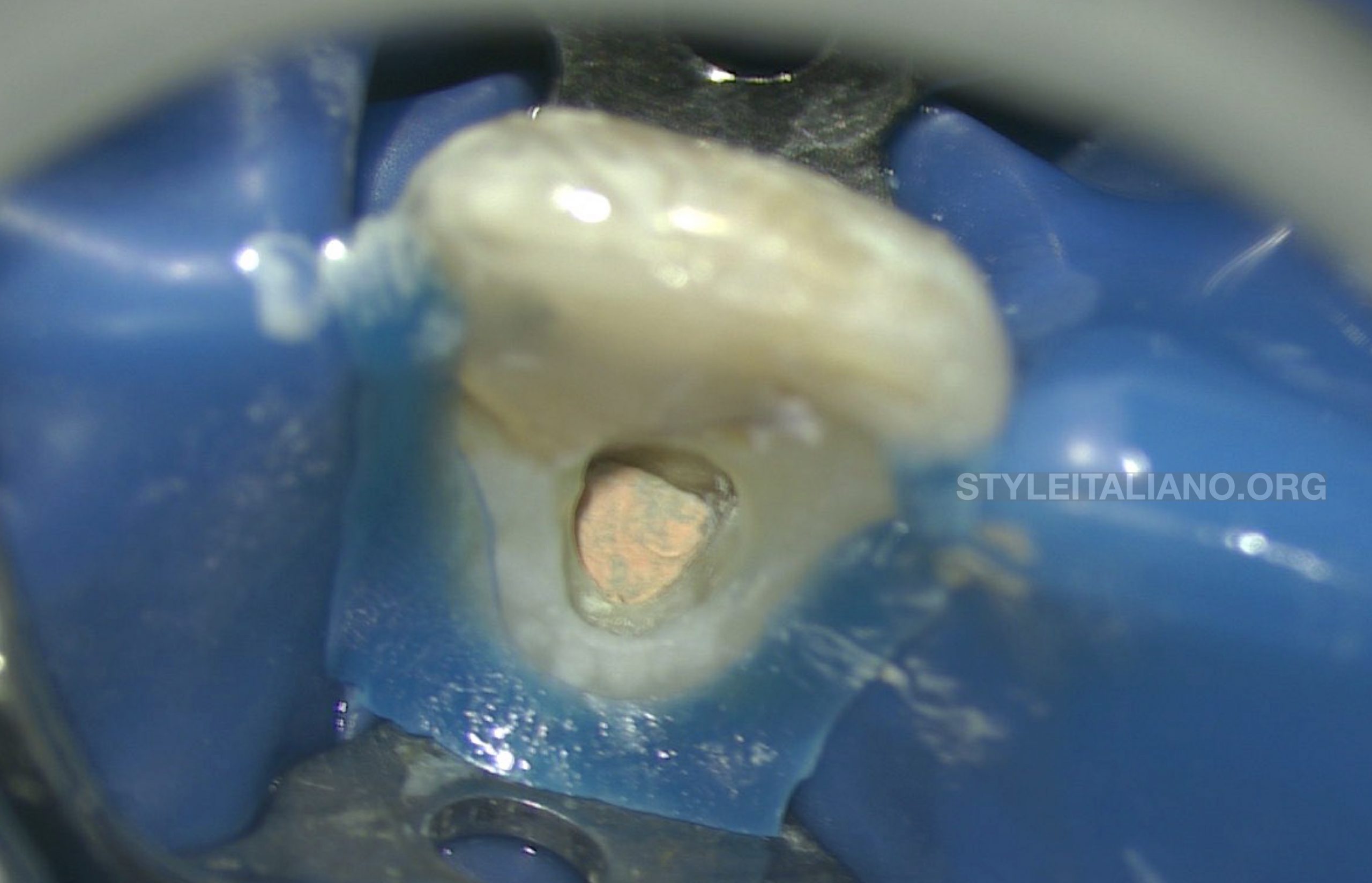
Fig. 7
The rest of the canal was then filled with thermo-placticized gutta percha to a level bellow the crystal bone level.
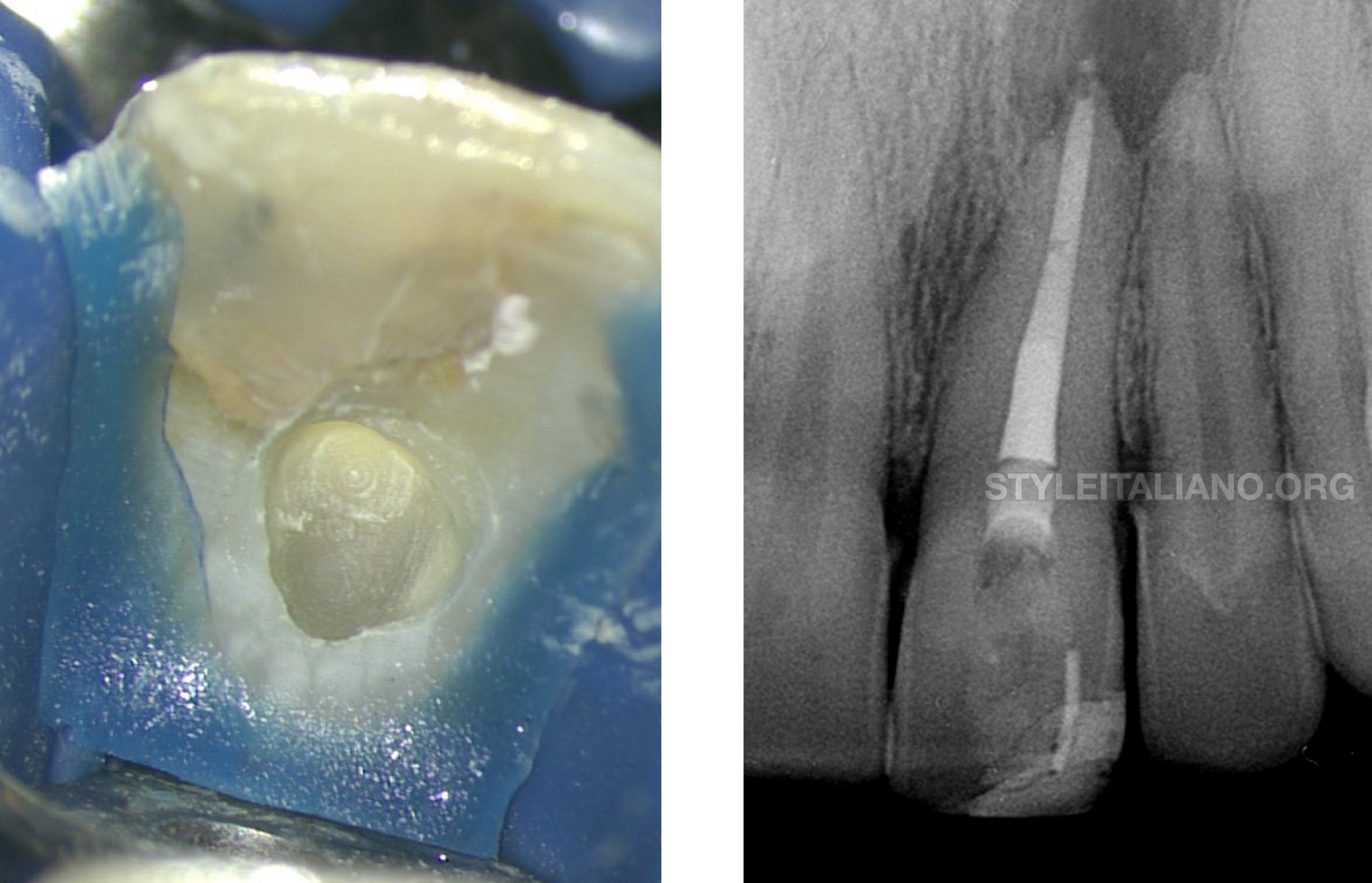
Fig. 8
Coronal seal was done with SDR. The pulp chamber then was filled with internal bleaching material (Ultradent) for 5 days

Fig. 9
Final situation of UL1 by restoring the function and aesthetic after internal bleaching and direct composite restoration.

Fig. 10
Three years review IOPA showing complete healing of the periapical lesion and new bone formation.

Fig. 11
Normal palatal gingival tissue around UL1 and the disappearance of the pocket after 3 years recall.

Fig. 12
Before and after 3 years, clinical and aesthetic situation of UL1.
Conclusions
Endodontically treated teeth always has to be restored to function and aesthetic. Root canal treatment has surprisingly high and long term prognosis if conducted properly (Ng et al. 2011, Salehrabi & Rotstein 2004, Salehrabi & Rotstein 2010).
On the other hand, since its introduction in the clinical Endodontic treatment Torabinejad et al. in 1993 at Loma Linda University and King’s College London, MTA showed a significant high success rate in different implications in Endodontics (Tang et al. 2010, Torabinejad et al. 1995, Giovarruscio et al. 2020), owing to it’s biocompatibility, bioactivity, high alkaline pH, and antibacterial activity (Parirokh & Torabinejad 2010).
In this case report, along with good chemo-mechanical debridement and good coronal seal, MTA has played a major role in the healing process of the peri-apical lesion,
Bibliography
- Basrani, B. and Haapasalo, M., 2012. Update on endodontic irrigating solutions. Endodontic topics 27(1), 74-102.
- Giovarruscio M, Tonini R, Zavattini A, Foschi F (2020) Reparative procedures for endodontic perforations: towards a standardised approach. ENDO EPT 14, 217-228.
- Ng YL, Mann V, Gulabivala K (2011) A prospective study of the factors affecting outcomes of non‐surgical root canal treatment: part 2: tooth survival. International endodontic journal 44(7), 610-625.
- Ørstavik D, Pitt Ford TR (2008) Apical Periodontitis: Microbial infection and host responses. In: Orsta Ørstavik vik D and Pitt Ford TR, Essential Endodontology 2nd edition. Oxford: Blackwell Science, 1-9.
- Parirokh M, Torabinejad M (2010) Mineral trioxide aggregate: a comprehensive literature review—part I: chemical, physical, and antibacterial properties. Journal of endodontics 36(1), 16-27.
- Reit C (1986) On decision making in endodontics. A study of diagnosis and management of periapical lesions in endodontically treated teeth. Swed Dent J 4. 1–30.
- Salehrabi R, Rotstein I (2004) Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. Journal of endodontics 30(12), 846-850.
- Salehrabi R, Rotstein I (2010) Epidemiologic evaluation of the outcomes of orthograde endodontic retreatment. Journal of endodontics 36(5), 790-792.
- Tang Y, Li X, Yin S (2010) Outcomes of MTA as root-end filling in endodontic surgery: A systematic review. Quintessence International 41(7).
- Torabinejad M, Hong CU, McDonald F, Pitt Ford TR (1995) Physical and chemical properties of a new root-end filling material. Journal of endodontics 21(7), 349-353.
- Torabinejad M, Watson TF, Pitt Ford TR (1993) Sealing ability of a mineral trioxide aggregate when used as a root end filling material. Journal of Endodontics 19(12), 591-595.