Third molars: extraction or endodontics?
09/12/2019
Paolo Generali
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Third molars, or, more popularly, wisdom teeth usually erupt in most patients after the age of 17. Abnormal eruption patterns make them more susceptible to dental decay, as well as gingival and periodontal diseases. If there is insufficient anatomic space to accommodate normal eruption, extraction of third molars is the preferred option, to prevent acute and chronic inflammation or infection, resorption phenomenon, carious lesions (including those of adjacent teeth), cysts, and displacement or destruction of adjacent hard tissue structures.
Despite third molar extraction being a common dental procedure, retaining every functional component of the dental arch should be among the principle goals of contemporary dental practice; when fully erupted, third molars may work as a natural component of occlusion. They can become abutments for partial fixed or removable prosthesis, or constitute the donor tooth for an autotransplantation procedure.
Further, contraindication for extraction may exist. A list may include, among others, probable excessive damage to adjacent structures, compromised medical status, advanced age, risk of osteoradionecrosis or, more commonly today, risk of bisphosphonate-related osteonecrosis of the jaw.
In these clinical situations, the retention of a third molar would be essential even if it requires endodontic treatment.

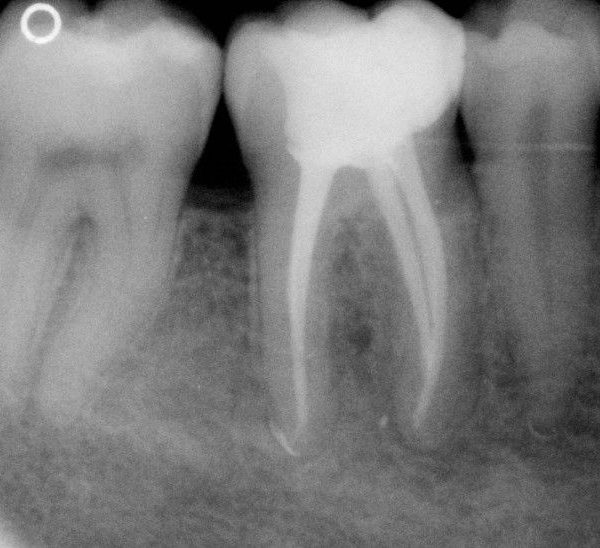
Fig. 1
A third mandibular molar was endodontically treated because of swelling and chronic pain upon chewing. After eight years, the tooth is healed and fully functional.
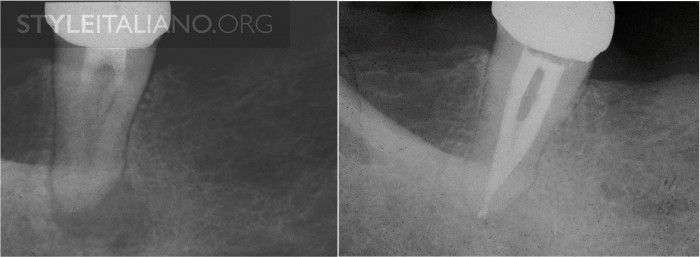
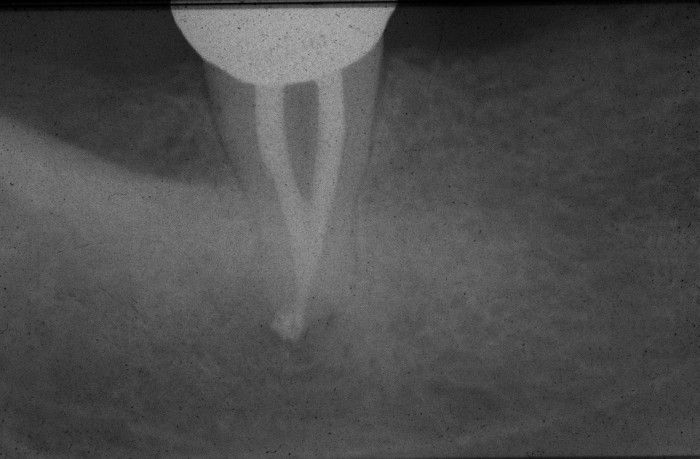
Fig. 2
A third mandibular molar, used as an abutment for a removable partial denture in a 80 y/o patient, was endodontically treated more than ten years ago. Morphology quite unusual, one root, reported frequency 17% (Sidow et al., JOE 2000) At a seven-year recall, the periapical radiolucency disappeared.

Fig. 3
Another third mandibular molar. Anatomical features are the most frequent for this tooth, two roots-three canals. Mesial canals were confluent, type II.
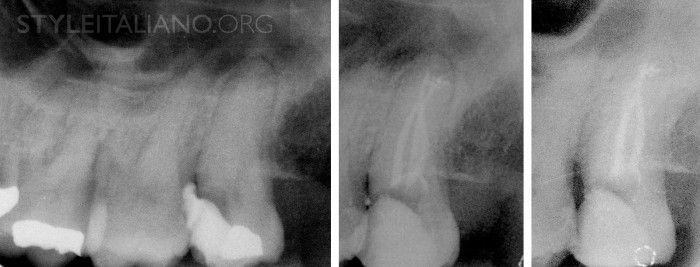
Fig. 4
Mandibular third molars are often mesioinclinated, making endodontic access less difficult. On the other hand, maxillary third molars are distally inclinated, making access even more difficult than usual. In this particular case, however, a deep mesial carious lesion helped in accessing root canal anatomy. Endodontics was preferred upon extraction because of the risk of biphosphonate-related osteonecrosis of the jaw.
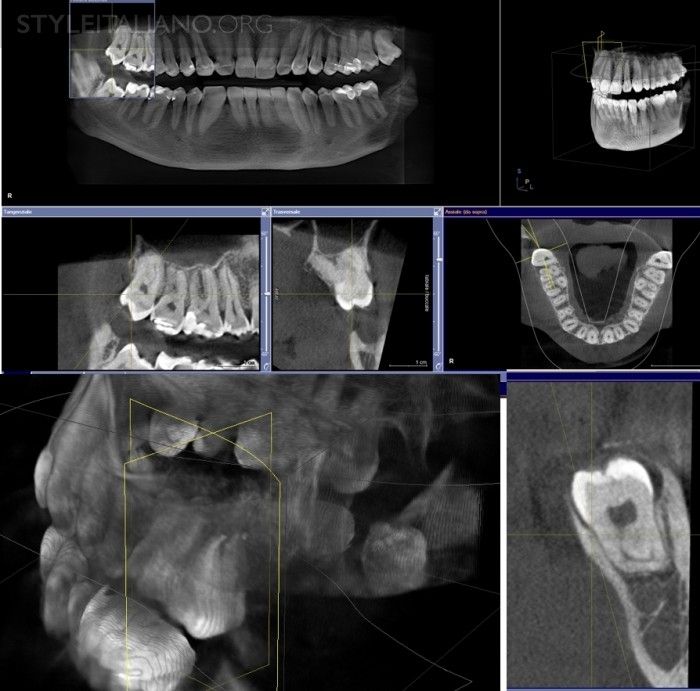
Fig. 5
A good periapical radiograph would provide adequate information on the anatomy of third molar teeth and the surrounding structures; however, root dilacerations parallel to the x-ray beam would not always be apparent on the radiograph. CBCT should only be done when the conventional periapical radiographs fail to provide adequate information. “Cognitive deduction of the clinical picture and intelligent interpretation of radiologic information”(Krithikadatta, JOE 2010) should be the best way to understand the morphological features of third molars. Anyway, sometimes there are other concurrent indications for a CBCT, and this can show some interesting features.
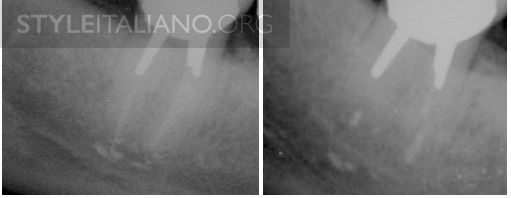
Fig. 6
Proximity of nerve structures: over-instrumentation and extrusion of irrigants and/or obturation materials can lead to local injury to the alveolar nerve. In this case, paresthesia of the lip occurred after endodontic and restorative treatment of a third mandibular molar. Patient was referred for periapical surgery and symptoms subsided.
Conclusions
Endodontic treatment of third molars with varying root-canal morphology and difficult access can be challenging. Nevertheless, modern techniques and devices make third molar endodontics predictable. A comprehensive review upon this topic has been published by Ahmed in 2012.
The root canal morphology of third molars shows an increased likelihood for aberrations, such as dilacerations, C-shaped canals and unpredictable morphological features, that should be identified accurately before commencing endodontic treatment. Intelligent evaluation of clinical and radiographic data makes possible to understand the unpredictable anatomy of these teeth. Magnification and coaxial illumination allow the identification of canal orifices, along with the "Laws" postulated by Krasner and Rankow. The proximity of alveolar nerve, with respect to the apexes of third mandibular molars, suggests, even more than in usual cases, a safe irrigation technique, such as the use of side vented needles or negative pressure irrigation systems. Following these principles, extraction of third molar teeth, usually considered as a common dental procedure, should became more and more uncommon.
Bibliography
Ahmed HM. Management of third molar teeth from an endodontic perspective. Eur J Gen Dent 2012;1:148-60
Sidow SJ, West LA, Liewehr FR, Loushine RJ. Root canal morphology of human maxillary and mandibular third molars. J Endod. 2000; 26(11):675-8.
Plotino G. A mandibular third molar with three mesial roots: A case report. J Endod 2008;34:224-6.
Grover AK, Grover SK . Mandibular third molar-endodontic perspective. Endodontology. 1992 Jun.; 4(1): 31-6
Krasner P, Rankow HJ. Anatomy of the Pulp-Chamber Floor. J Endod 2004; 30: 516.
Krithikadatta J, Kottoor J, Karumaran CS, Rajan G. Mandibular first molar having an unusual mesial root canal morphology with contradictory cone-beam computed tomography findings: a case report. J Endod. 2010;36(10):1712-6.