Saving the unsavable: Intentional replantation
14/07/2025
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
A 44 year old male presented in our referral clinic concerned about a huge defect on his upper left central incisor. He wished a second opinion on his problem as the only solution offered to him was an extraction. Patient mentioned a sport injury on his upper jaw 25 years ago. The clinical and radiographic examination revealed an enormous subgingivall defect due to external resorption of UL1.

Fig. 1
The initial preoperative periapical radiograph shows an extensive defect due to external resorption
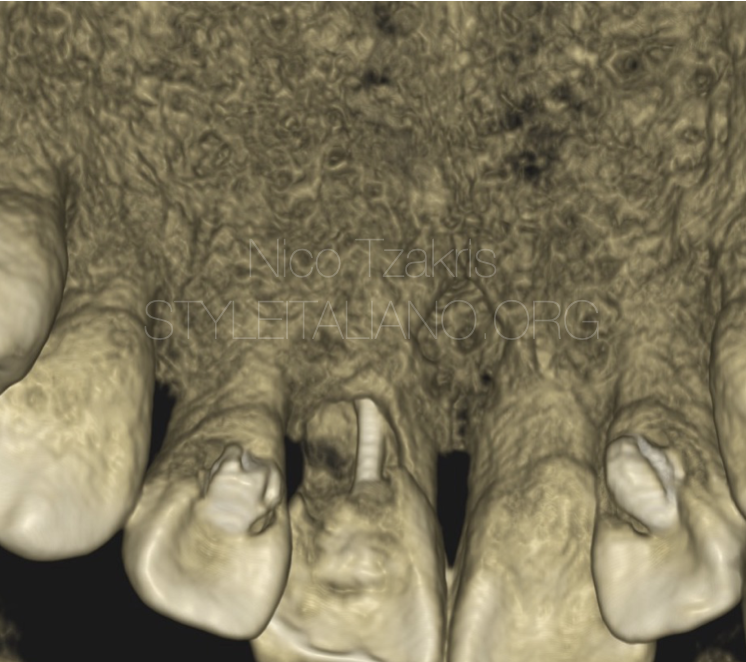
Fig. 2
3d view. A CBCT scan was taken in order to evaluate the borders and the dimensions of the defect.

Fig. 3
The defect was extending almost through all the tooth structure from palatal to buccal wall compromising the tooth integrity. In addittion, small periapical lesion was evident of the cbct scan. After discussing the different treatment options we decided to continue with the intentional replantation of the tooth. The procedure was performed as per ESE guidelines for intentional replantation. The total time of the manipulation after the extraction was less than 12 minutes

Fig. 4
The tooth was extracted very carefully and as much atraumatic as possible in order to prevent possible root fracture.
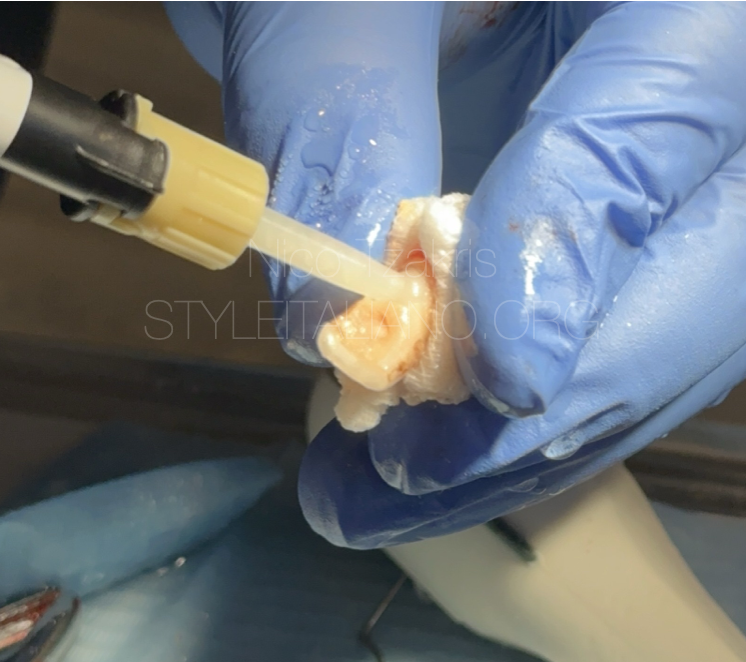
Fig. 5
The defect was prepared and filled with a self-adhesive, dual-cure, resin-modified glass ionomer material that promotes adhesion of the soft tissues to his surface.

Fig. 6
Polishing of the material. The last step before reinserting the tooth into the socket.

Fig. 7
Final postoperative radiograph. Retropreparation of the apical part was also performed with ultrasonics and bc putty in order to eliminate the apical pathology. A splint was used for 5 days to stabilise the tooth in the socket.

Fig. 8
A two year follow up shows no pathology. The tooth is functional and stable.

Fig. 9
About the author:
Niko Tzakris
2013 - Medical University of Plovdiv - Dental School
2022 - New York University college of dentistry. Cpde in implantology and oral rehabilitation
2023 - Aristotle medical university of Thessaloniki . Msc in research methodoly in Medicine and in Health Sciences
He is the owner of Waterfall Smiles in Edessa,c Macedonia Greece. A dental referral clinic treating complex endodontic and surgical cases.
He is an associate dentist at the square dental referral clinic Isle of Man, UK with special interest in endodontics. He is lecturing both nationally and internationally and in private courses.
Conclusions
The concept of intentional replantation (IR) dates back centuries, with descriptions of similar procedures appearing in ancient texts. IR may be considered in carefully selected cases as both a primary therapeutic option and a measure of last resort aimed at postponing the extraction of structurally or functionally compromised teeth. The temporary retention of the natural dentition may confer clinical advantages by reducing the need for prosthetic rehabilitation. While the current body of evidence remains limited, IR has shown potential as a viable, minimally invasive, and economically advantageous alternative to conventional endodontic retreatment or extraction, assuming the practitioner possesses the requisite training and expertise.
Bibliography
1. Lin Wang, Hua Jiang, Yang Bai, Qiang Luo, Hao Wu & Hongchen Liu
“Clinical outcomes after intentional replantation of permanent teeth: A systematic review” (2020, Biomolecules & Biomedicine)
2. Jin‑wei Huang, Ye‑na Gan, He Xu, Sheng Han, He Zhu, Lu Jia, Nan Li, Duo‑duo Li & Zhi‑gang Cai
“Tooth intentional replantation from 1964 to 2023: A bibliometric analysis” (2023, Dental Traumatology)
3. Beatriz Pereira, Mariana D. Pires, Abayomi O. Baruwa, Jorge N. R. Martins & António Ginjeira
“Intentional replantation of severely compromised teeth” (2022, Giornale Italiano di Endodonzia)
4. M. Pisano, F. Di Spirito, S. Martina, G. Sangiovanni, F. D’Ambrosio & A. Iandolo
“Intentional Replantation of Single‑Rooted and Multi‑Rooted Teeth: A Systematic Review” (2022, Healthcare/Basel)




