Restoring the unrestorable: Surgical extrusion
02/05/2024
Xavier-Fructuós Ruiz
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
One of the main objectives of dentistry is the preservation of the natural dentition.1 Carious lesions, dental trauma, root resorptions or iatrogenic procedures such as root perforations can cause the loss of healthy dental tissue. When the loss of dental tissue occurs at the subgingival level; the restorability of these teeth is seriously compromised.2
In these cases, the placement of a restoration below the gingival margin can cause inflammation of the gingival tissues, loss of periodontal clinical attachment and bone loss due to the invasion of the so-called 'biological space'.3 Clinically, this is observed with the presence of periodontal pockets, recessions and/or gingival bleeding.4 Furthermore, not having a minimum of 1.5 mm of healthy dental tissue circumferentially, also called ferrule, can cause the failure of the definitive restoration.5
There are different treatments with the aim of lengthening the clinical crown and therefore, having enough healthy dental tissue to accommodate a restoration in a more suitable condition. Surgical crown lengthening6, rapid or forced orthodontic extrusion7 and surgical extrusion8 are methods that allow us to avoid the invasion of biological space, and at the same time gain enough ferrule to increase the survival of our restorations.
Surgical extrusion was first described in 1978 as intraalveolar transplantation, with the aim of maintaining teeth with cervical root fractures in patients who had suffered dental trauma.9 The procedure consists of repositioning the tooth in a more coronal (supragingival) position from the same alveolus; thus lengthening the clinical crown. With the help of fine elevators and forceps, the syndesmotomy and luxation of the tooth is performed, trying to minimize damage to the periodontal ligament and subsequently, the tooth is splinted in the desired position using sutures or semi-rigid splinting.10–12
The main objective of this article is to present a case of a non-restorable tooth in which surgical extrusion was performed and describe the steps from endodontic treatment to cementation of the indirect restoration, ``from root to crown''.
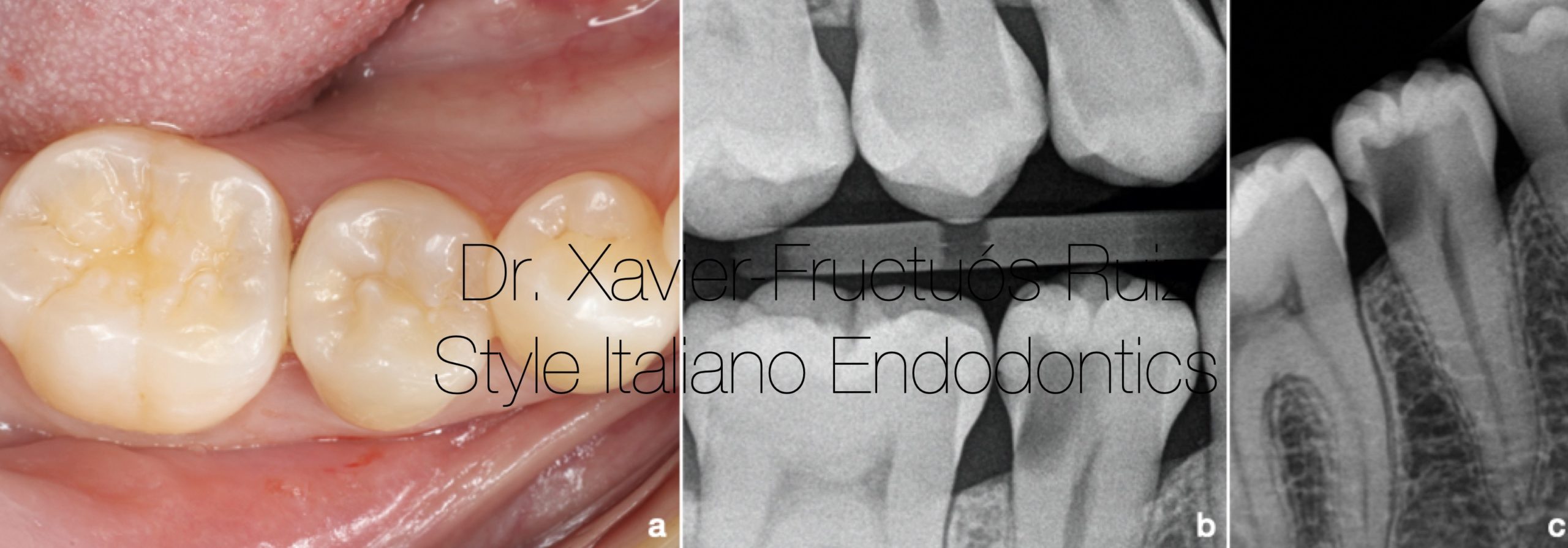
Fig. 1
Initial clinical and radiographic examination. (a) Intraoral photography. (b) Bitewing x-ray. (c) Periapical radiography.

Fig. 2
Clinical and radiographic examination after caries removal. (a) Intraoral photography. (b) Bitewing x-ray.
Surgical video.
2 weeks video.
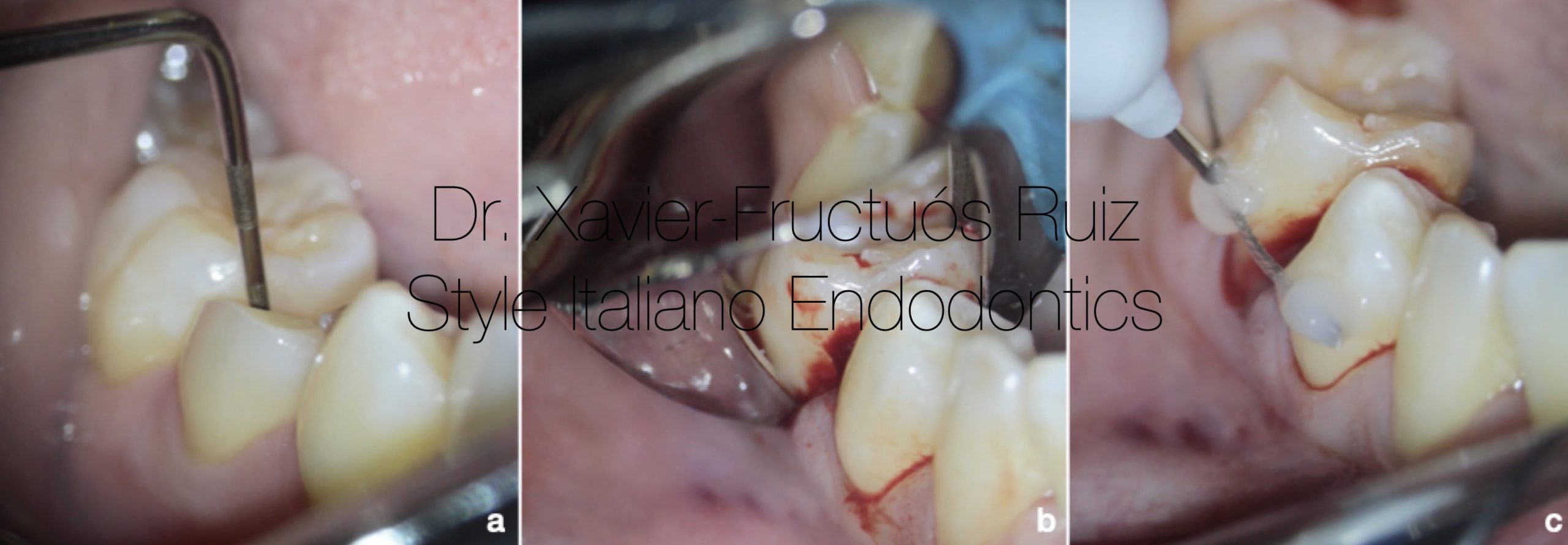
Fig. 3
Surgical extrusion procedure. (a) Periodontal probing (b) Tooth dislocation. (c) Semi-rigid splinting.

Fig. 4
Clinical and radiographic control 2 weeks after surgical extrusion. (a) Intraoral photography. (b) Bitewing x-ray. (c) Periapical radiography.
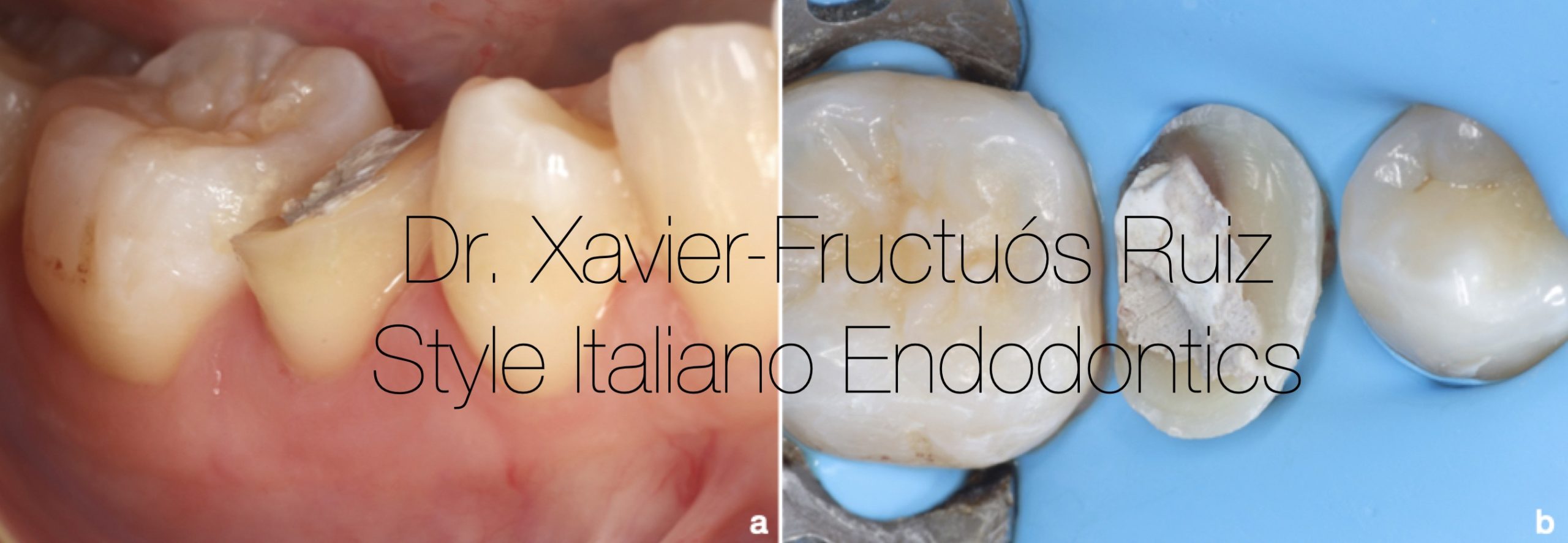
Fig. 5
(a) Intraoral photograph after removing the splint. (b) Absolute isolation with rubber dam.

Fig. 6
Pre-endodontic restoration with composite. (a) Placement of the Automatrix® metal matrix. (b). Restoration of the distal margin using SDR® composite and Ceram-X Universal®.
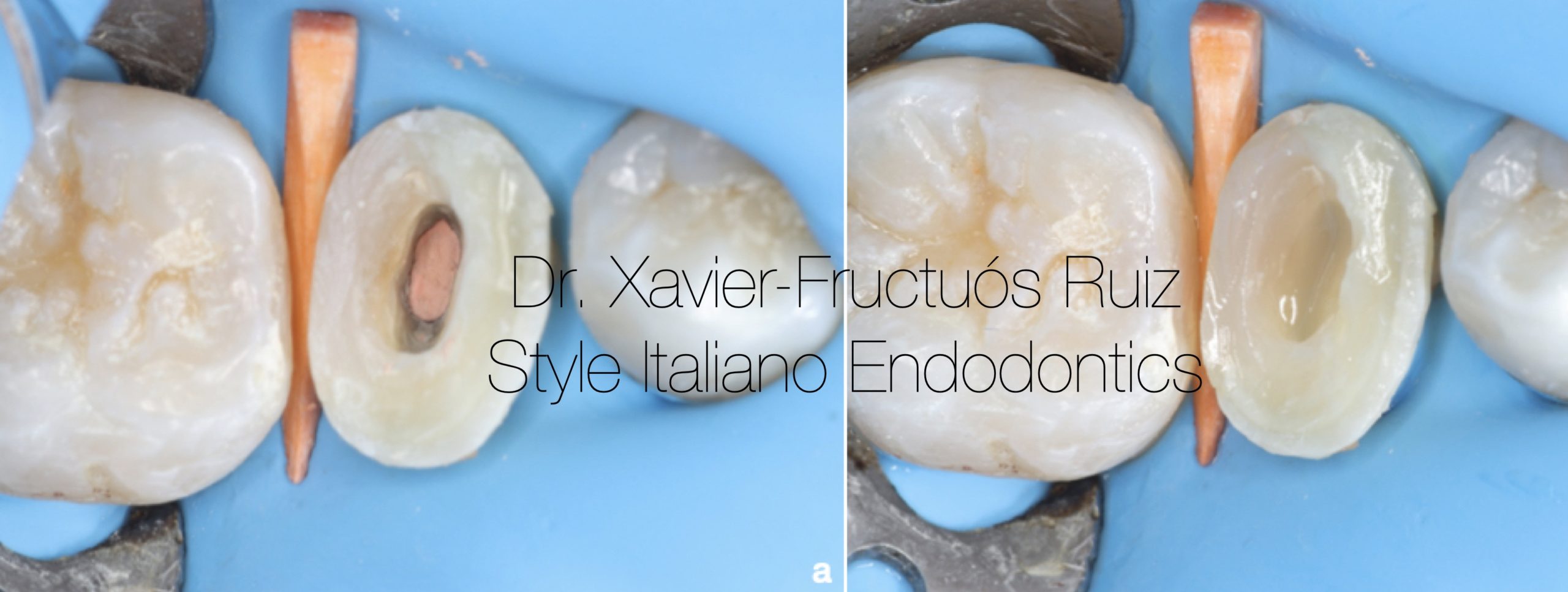
Fig. 7
Intraoral photography after endodontic filling. (b) Intraoral photograph after sealing the pulp chamber using SDR®.
Firstly, the access cavity was modified with the help of a StartX No. 3 ultrasonic tip (Dentsply Maillefer). A C+ #10 manual file (Dentsply Maillefer) was used to achieve apical patency and establish a correct working length. During the treatment, irrigation was carried out continuously with a 4.25% sodium hypochlorite solution. For the 'glide path' the Wave One Gold glider #15.02 reciprocating file (Dentsply Maillefer) was used and for the subsequent instrumentation the Wave One Gold Primary #25.06 reciprocating file was used. Finally, it was decided to instrument using a Profile #35.04 file (Dentsply Maillefer) to achieve correct apical calibration. The final irrigation consisted of 10% citric acid (1mL), followed by 4.25% sodium hypochlorite (5mL) and 96% alcohol (1mL).
Root filling was performed using a #50 caliber thermocompactor (Guttacondensor®, Dentsply Maillefer), after placing a master cone with taper (35.04) and an accessory gutta-percha cone impregnated in a resinous cement (AH- Plus, Dentsply Maillefer). (Fig.7a)
Subsequently, excess filling material was removed from the pulp chamber using an Endo Z bur (Dentsply Maillefer). The cavity was sealed with bulk fill SDR® composite (Dentsply DeTrey) (Fig.7b) and Ceram-X composite (Dentsply DeTrey) for the 'build-up'. Periapical radiographs were taken throughout the procedure. (Fig.8a,b,c,d)
After one month, it was decided to perform a postoperative clinical and radiographic control (Fig. 9a,b) and begin the preparation of the definitive restoration: an overlay type inlay with complete cusp coverage. Once the tooth was prepared (Fig. 10a), an impression was taken with Aquasil® silicone (Dentsply DeTrey), the antagonist impression, bite registrations and color taking; and was sent to the laboratory technician.
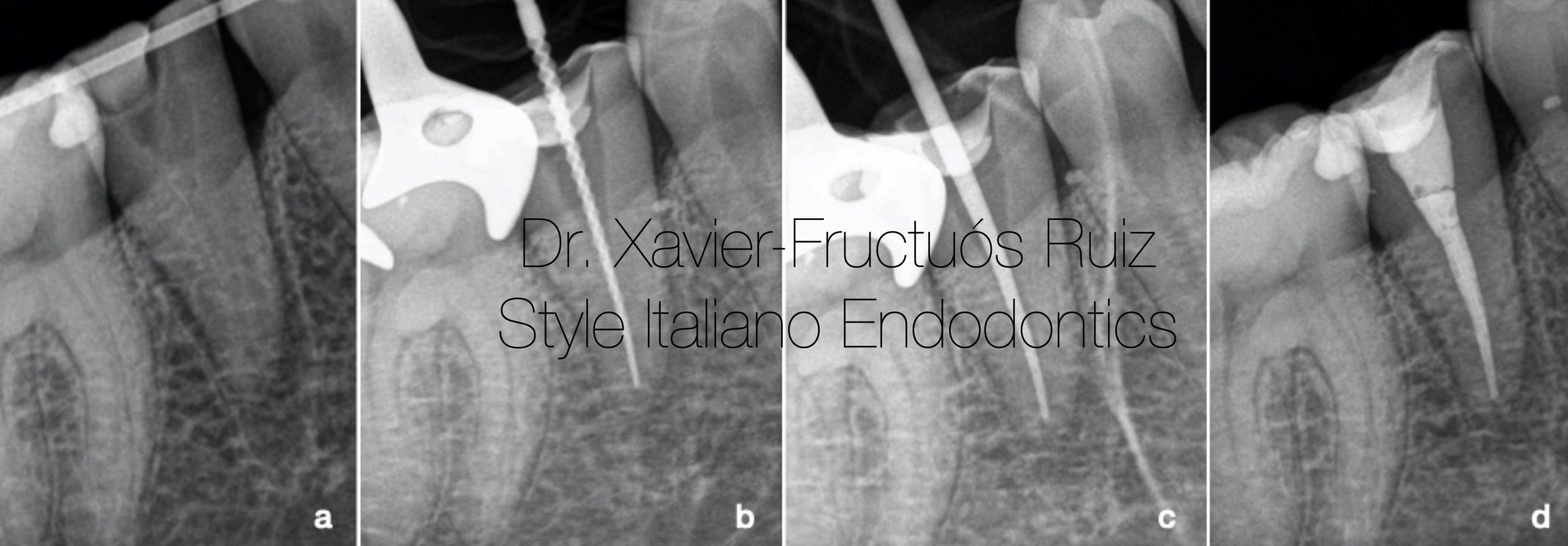
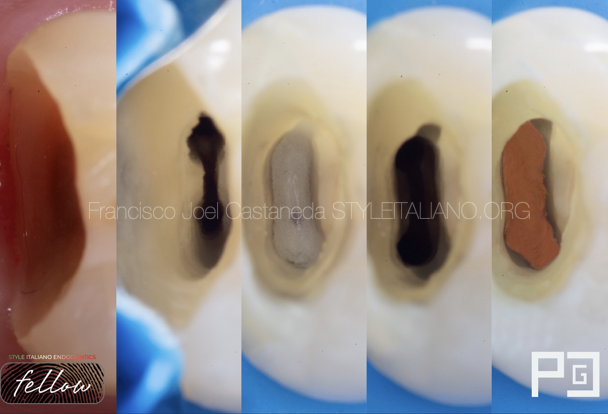
Fig. 8
Radiographic sequence of endodontic treatment. (a) Periapical radiograph 2 weeks after surgical extrusion. (b) Determination of working length. (c) Conometry. (d) Final.

Fig. 9
Radiographic control one month after performing the endodontic treatment. (a) Bitewing x-ray. (b) Periapical radiograph.

Fig. 10
On the next visit, the indirect CAD/CAM nanoceramic resin restoration was cemented. First, the marginal adaptation of the restoration was verified radiographically. Next, the preparation of the substrate and the restoration began for proper cementation. On the one hand, the restoration was sandblasted with 50 μm aluminum oxide and a layer of silane was applied for 60 seconds (Self-Cure Activator®, Dentsply DeTrey). At the same time, tooth preparation began by applying an abrasion using 50 μm aluminum oxide particles, protecting the adjacent teeth with Teflon and after performing absolute isolation with a rubber dam.
A 36% orthophosphoric etch was performed (DeTrey Conditioner®, Dentsply DeTrey) and Prime&Bond Active ® adhesive (Dentsply DeTrey) was applied to both the restoration and the tooth. The overlay was then cemented using Calibra® resin cement (Dentsply DeTrey). Finally, a correct polishing of the margins was performed and the occlusion was adjusted. (Fig.10b)
The clinical and radiographic controls after one year showed an asymptomatic tooth, with good health of the periodontal and periapical tissues, classifying the case as successful. (Fig.11a,b,c)

Fig. 11
Control clinical and radiographic examination 1 year after treatment (a) Intraoral photograph. (b) Bitewing x-ray. (c) Periapical radiograph.
Conclusions
Surgical extrusion represents a valid alternative to other procedures such as surgical crown lengthening and orthodontic extrusion. The selection of the appropriate treatment will depend on the aesthetic requirements, the position of the tooth in the arch, the crown-root proportion and the proximity and root morphology of the tooth and its adjacent teeth. The surgical extrusion procedure offers a series of advantages over other techniques such as a short treatment time and that can be performed in one session, low cost, good aesthetics, easy acceptance by the patient and a low incidence of failure.
In conclusion, surgical extrusion is a technique that presents good success rates for the preservation of natural dentition in teeth compromised by large subgingival cavities without sufficient healthy dental tissue structure, as shown in the present case.
Bibliography
1. Clark D, Levin L. In the Dental Implant Era, Why Do We Still Bother Saving Teeth? J Endod. 2019;45:S57-S65.
2. Marzadori M, Stefanini M, Sangiorgi M, Mounssif I, Monaco C, Zucchelli G. Crown lengthening and restorative procedures in the esthetic zone. Periodontol 2000. 2018;77:84-92.
3. Gargiulo AW, Wentz FM, Orban B. Dimensions and Relations of the Dentogingival Junction in Humans. J Periodontol. 1961;32:261-267.
4. Padbury A, Eber R, Wang HL. Interactions between the gingiva and the margin of restorations. J Clin Periodontol. 2003;30:379-385.
5. Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M. Ferrule effect: A literature review. J Endod. 2012;38:11-19.
6. Pilalas I, Tsalikis L, Tatakis DN. Pre-restorative crown lengthening surgery outcomes: a systematic review. J Clin Periodontol. 2016;43:1094-1108.
7. Faria LP de, Almeida MM de, Amaral MF, Pellizzer EP, Okamoto R, Mendonça MR. Orthodontic Extrusion as Treatment Option for Crown-Root Fracture: Literature Review with Systematic Criteria. J Contemp Dent Pract. 2015;16:758-762.
8. Pham HT, Nguyen PA, Pham TAV. Periodontal status of anterior teeth following clinical crown lengthening by minimally traumatic controlled surgical extrusion. Dent Traumatol. 2018;34:455-463.
9. Tegsjõ U, Valerius-Olsson H, Olgart K. Intra-alveolar transplantation of teeth with cervical root fractures. Swed Dent J. 1978;2:73-82.
10. Lee JH, Yoon SM. Surgical extrusion of multiple teeth with crown-root fractures: A case report with 18-months follow up. Dent Traumatol. 2015;31:150-155.
11. Kim DS, Shin DR, Choi GW, Park SH, Lee JW, Kim SY. Management of complicated crown-root fractures using intentional replantation: Two case reports. Dent Traumatol. 2013;29:334-337.
12. Moura LFAD, Lima MDM, Moura MS, Carvalho P V., Cravinhos JCP, Carvalho CMRS. Treatment of a crown-root fracture with intentional replantation - case report with 16-year follow-up. Int Endod J. 2012;45:955-960.
13. Das B, Muthu MS. Surgical extrusion as a treatment option for crown-root fracture in permanent anterior teeth: A systematic review. Dent Traumatol. 2013;29:423-431.
14. Hempton TJ, Dominici JT. Contemporary crown-lengthening therapy: A review. J Am Dent Assoc. 2010;141:647-655.
15. Krug R, Connert T, Soliman S, Syfrig B, Dietrich T, Krastl G. Surgical extrusion with an atraumatic extraction system: A clinical study. J Prosthet Dent. 2018;120:879-885.
16. Oikarinen KS, Stoltze K, Andreasen JO. Influence of conventional forceps extraction and extraction with an extrusion instrument on cementoblast loss and external root resorption of replanted monkey incisors. J Periodontal Res. 1996;31:337-344.
17. Elkhadem A, Mickan S, Richards D. Adverse events of surgical extrusion in treatment for crown-root and cervical root fractures: A systematic review of case series/reports. Dent Traumatol. 2014;30:1-14.