Re-treatment nightmare
18/05/2023
Ahmed Alwaidh
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
In our daily practice, we face a lot of difficulties in root canal treatment and re-treatment. Some of these difficulties may be due to the case itself, and others may happen during the procedure. Key factors to overcome such situations are identifying these difficulties and knowing how to deal with them.
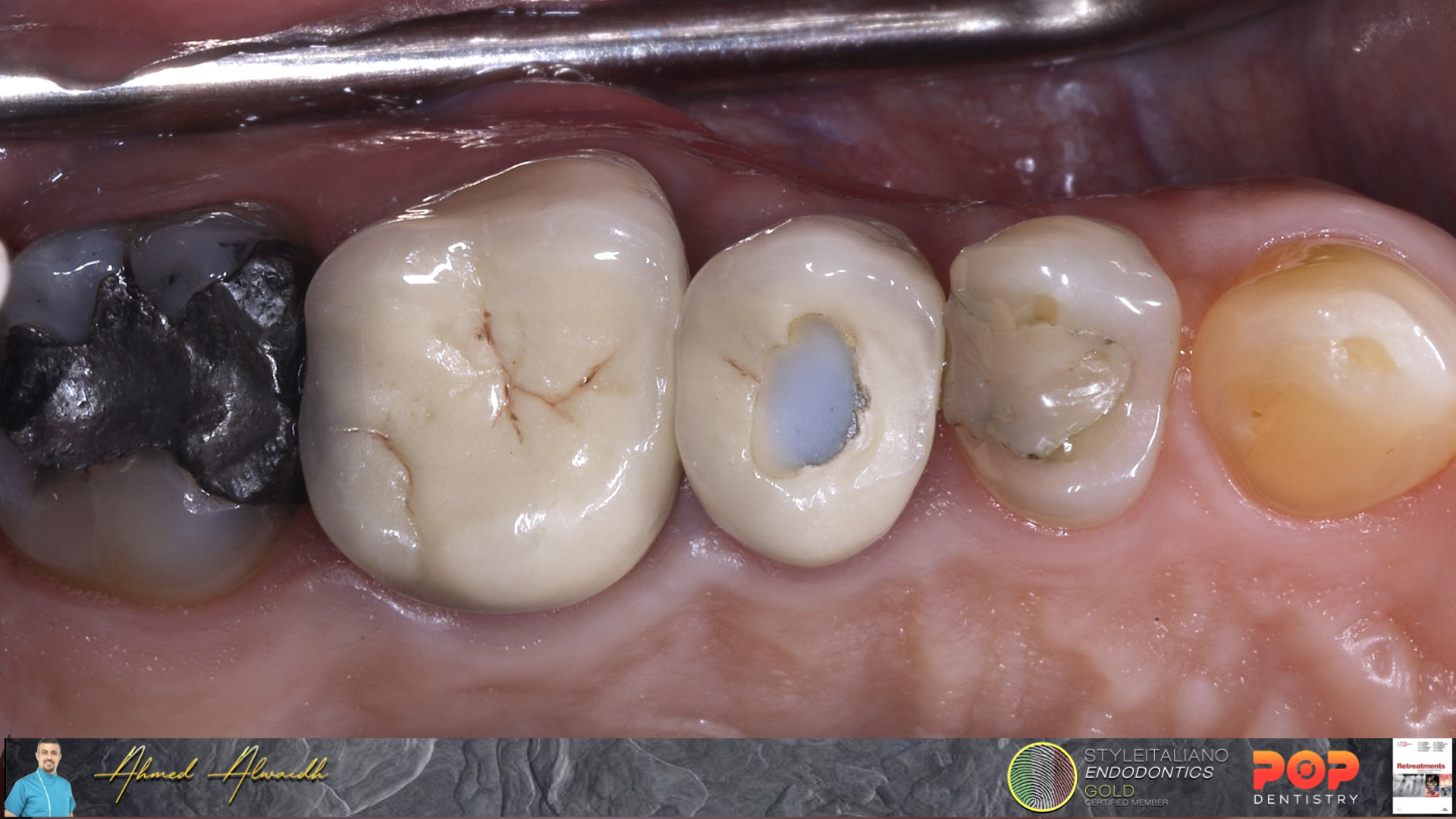
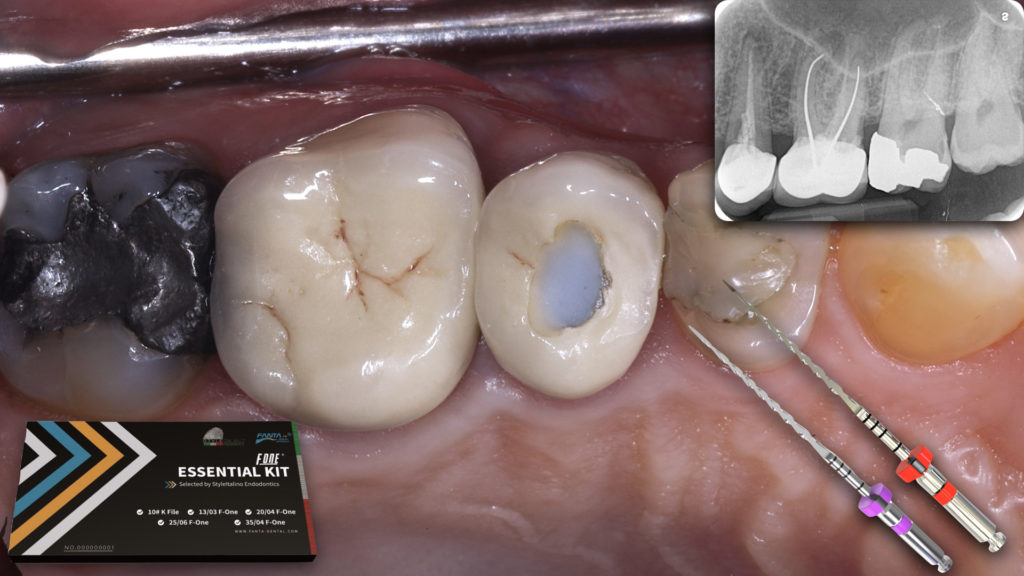
Fig. 1
A 47 years old male presented complaining of tenderness in his upper left posterior teeth. History of crowns 5 years ago, then he had a severe pain two weeks later. The patient went back to his dentist who did a root canal treatment in one of the crowned teeth without removing the crown. The patient mentioned the severe pain been gone, but he never felt comfortable on eating on the left side since then, which then started to increase in the last 3 weeks.
Clinically, UL5 & UL6 having PFM crowns, with a hole been sealed with composite in the occlusal surface of UL5 crown. Both UL5 & UL6 have moderate tender to percussion, with tenderness to buccal palpation, especially in the area related to mesio-buccal root of UL6.
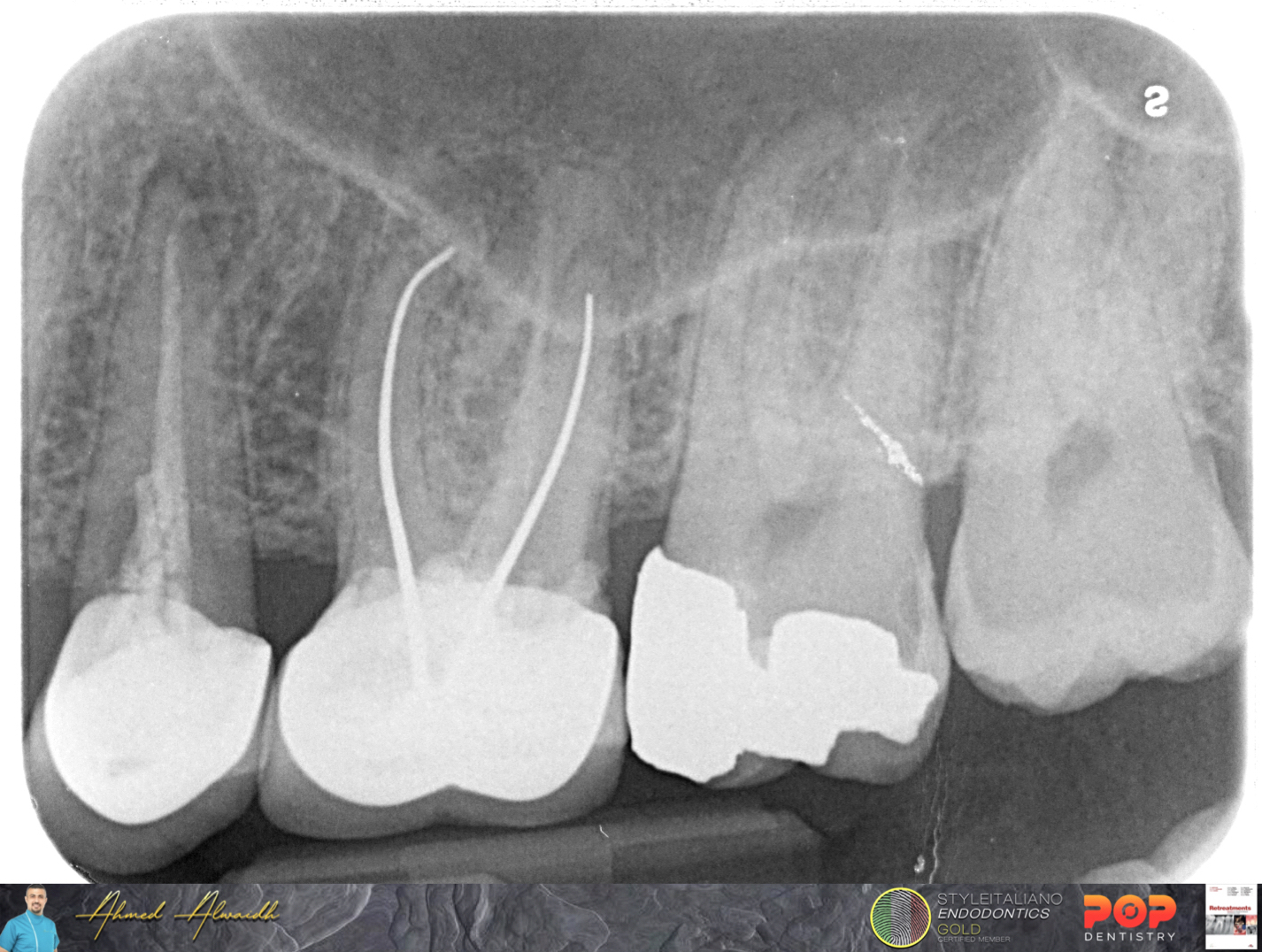
Fig. 2
Initial IOPA revealed both UL5 & UL6 had poor quality root canal treatments, which is considered one of the major causes of root canal treatment failure (Hoen & Pink 2002), with evident radiolucencies around the apices of UL5 & UL6 roots, and poorly fitted crowns.
Diagnosis: Both UL5 & UL6 previously treated with symptomatic apical periodontitis.
Treatment plan:
1- Dismantling the crowns of UL5 & UL6.
2- Root canal re-treatment of both UL5 & UL6.
3- Delivering new and well fitted crowns for both UL5 & UL6.
4- Keeping monitoring the healing.
Difficulties that can be anticipated from the IOPA reading:
1- Removal of silver points from MB1 & DB of UL6 which require careful handling.
2- Scouting and preparation of a missed MB2 in UL6.
Difficulties that can be anticipated from the IOPA reading:
1- Removal of silver points from MB1 & DB of UL6 which require careful handling.
2- Scouting and preparation of a missed MB2 in UL6.
At first visit, I started with re-treatment of UL6. Crown been dismantled to reveal defective composite restoration underneath.
UL6 been isolated with rubber dam, then started removal of the defected composite restoration, with special attention of not bringing the bur close to the silver points, in order not to damage the extension of the coronal part of the silver points and so better grasping.
The remnant composite close to the silver points been removed carefully with US scaler on low power, as excessive heat may cut the silver points. The silver points then been pulled successfully from MB1 & DB canals of UL6.
The pulp chamber been disinfected with NaOCl before going inside any of the canals. Chamber been cleaned by burs and ultrasonic tips.
The coronal part of MB1, DB and P canals of UL6 been prepared with Open file (Fanta Dental, Shanghai), then MB1 & DB been prepared to full working length with F One file #25/06 (Fanta Dental, Shanghai). While P canal been retreated to full working length with the same file F One #25/06. Copious NaOCl disinfection and US activation after each step.
MB2 been located under the microscope and confirmed with explorer. It was impossible to negotiate MB2 manually with C file #10. With the use of F One #13/03 (SIE Essential Kit, Fanta Dental, Shanghai), I was able to negotiate mechanically few mm of MB2, then coronal preparation with Open File. After that I used F One #13/03 to negotiate MB2 mechanically to full working length, followed by preparation of MB2 to full working length with F One #25/04. Thorough NaOCl disinfection and US activation, then UL6 been dressed with non-setting calcium hydroxide Intra canal medication.
After two days, I dismantled the crown of UL5.
UL5 been isolated with rubber dam. Re-treatment started by using Open file for the coronal part, followed by F One #25/06 for re-treatment to full working length. Thorough NaOCl disinfection and US activation. UL5 been dressed with non-setting calcium hydroxide intra canal medication
After two weeks, the patient presented symptoms-free. Thorough NaOCl disinfection, followed EDTA 17%, activated by US.
Unfortunately and before obturation, I noticed some bleeding from MB2 of UL6. After careful inspection under the microscope, I noticed a strip perforation in the middle third of MB2. So the obturation been modified as the following:
1- The strip perforation been sealed with BC Putty been placed at the perforation site with the use of MAP System.
2- The original MB2 canal been filled with Premixed BC cement, which came out through MB1, indicating both MB1 & MB2 merges together at the apical third.
3- DB, P, and UL5 canal been filled with premixed BC cement.
4- MB1 been obturated with hydraulic technique.
5- MB2 been obturated by hydraulic technique to a level just below the perforation site. Gutta percha remnant above the perforation site was easily removed with the aid of MC-Shaper (Fanta Dental, Shanghai).
6- DB, P and UL5 were obturated with hydraulic technique.
7- More BC Putty been placed above the perforation site and the gutta percha of the original canal.
8- The last coronal 3 mm of MB2 been obturated with Premixed Hi flow BC cement and thermoplasticized gutta percha.

Fig. 3
After finishing obturation of both UL5 & UL6, pulp chambers been cleaned from the excess of root canal filling materials. Both teeth been restored with composite restorations, and the patient been scheduled for full crown coverage for both UL5 & UL6.

Fig. 4
Post operative IOPA
Conclusions
Despite the damage in teeth and the peri-radicular area, non-surgical root canal re-treatment has high success rate (Salehrabi & Rotstein, 2010). Although this case had multi-disciplinary approaches and many difficulties been encountered, but with careful studying of the case, a systemic treatment plan after discussing with the patient about treatment options, and the ability to deal with different scenarios, a favourable treatment been approached.
Once again, the unique flat side design of the F One file by Fanta has proven that this file has superiority in dealing with many difficult scenarios like root canal re-treatment and mechanical negotiation of calcified canals, due to it’s ability to move the debris from the flutes to the flat side and then coronaly, so less stress on the file, and continuous cutting efficacy (Di Nardo et al. 2020, Zanza et al. 2021).
Bibliography
Di Nardo D, Miccoli G, Mazzoni A, Seracchiani M, Gambarini G, Testarelli L (2020) Centering ability of a new nickel-titanium rotary instruments with a peculiar flat-side design: an in vitro study. J Contemp Dent Pract 21(5), 539-42.
Hoen M M and Pink F E (2002) Contemporary endodontic retreatments: an analysis based on clinical treatment findings. Journal of endodontics 28(12), 834-836.
Salehrabi R. and Rotstein I. (2010) Epidemiologic evaluation of the outcomes of orthograde endodontic retreatment. Journal of endodontics 36(5), 790-792.
Zanza A, Seracchiani M, Reda R, Di Nardo D, Gambarini G, and Testarelli L (2021) Role of the crystallographic phase of NiTi rotary instruments in determining their torsional resistance during different bending conditions. Materials 14(21), 6324.