Non-surgical management of Large-Apical Lesion with Open Apex
06/12/2023
Fellow
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Bacterial infection of the dental pulp may lead to periapical lesions. They are generally diagnosed either during routine dental radiographic examination or following acute pain in a tooth. Most periapical lesions (>90%) can be classified as dental granulomas, radicular cysts or abscesses. The incidence of cysts within periapical lesions varies between 6 and 55%. The occurrence of periapical granulomas ranges between 9.3 and 87.1%, and of abscesses between 28.7 and 70.07%. There is clinical evidence that as the periapical lesions increase in size, the proportion of the radicular cysts increases. However, some large lesions have been shown to be granulomas. The definitve diagnosis of a cyst can be made only by a histological examination. However, a preliminary clinical diagnosis of a periapical cyst can be made based on the following: (a) The periapical lesion is involved with one or more non-vital teeth, (b) the lesion is greater than 200 mm2 in size, (c) the lesion is seen radiographically as a circumscribed, well-defined radiolucent area bound by a thin radiopaque line, and (d) it produces a straw-colored fluid upon aspiration or as drainage through an accessed root canal system.
The ultimate goal of endodontic therapy should be to return the involved teeth to a state of health and function without surgical intervention.All inflammatory periapical lesions should be initially treated with conservative nonsurgical procedures. Surgical intervention is recommended only after nonsurgical techniques have failed.Besides, surgery has many drawbacks, which limit its use in the management of periapical lesions.Various studies have reported a success rate of up to 85% after endodontic treatment of teeth with periapical lesions. A high percentage of 94.4% of complete and partial healing of periapical lesions following nonsurgical endodontic therapy has also been reported.

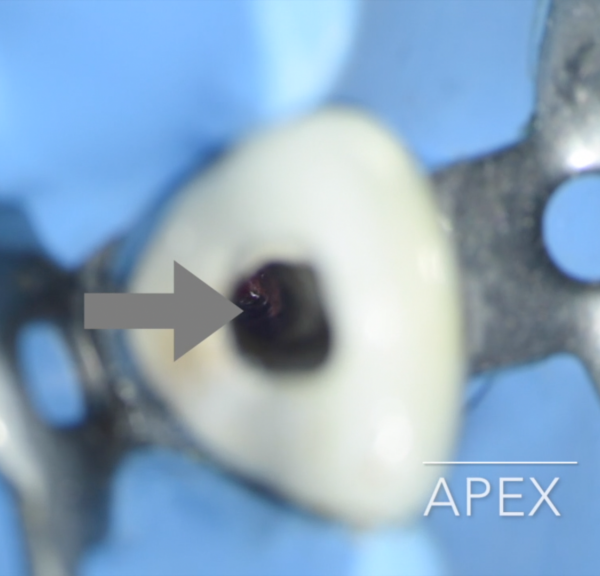
Fig. 1
A 22 year old female patient presented to practice with a chief complaint of discolored maxillary central incisors with sinus track opening. Dental history revealed that the patient had suffered a trauma 10 years ago and had neglected to consult a dentist. Clinical examination revealed discolored tooth no.11 and 12. Radiographic examination revealed central incisors with open apex and lateral incisor associated with periapical lesion.
Treatment planning was done and patient was advised to do root canal therapy followed by apexification procedure with MTA followed by prosthetic rehabilitation for discolored central incisors.

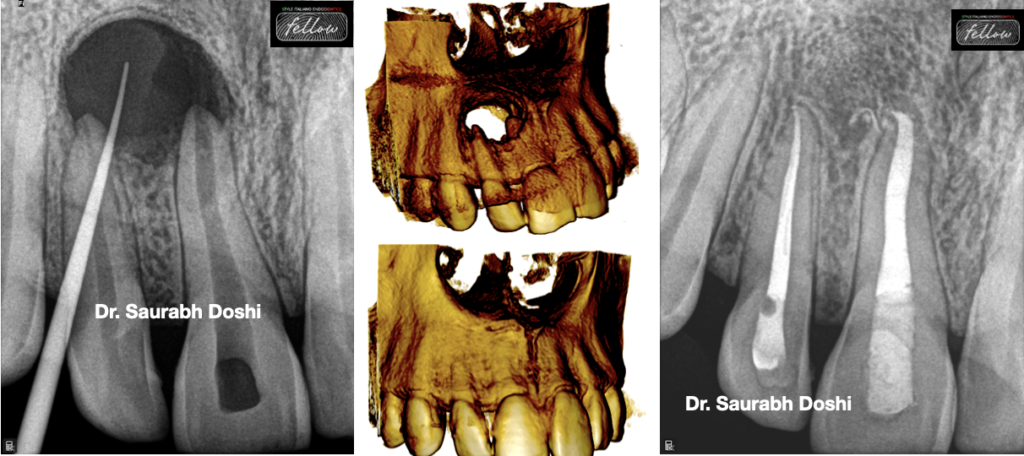
Fig. 2
After application of rubber dam (Hygienic Dental Dam, Colténe Whaledent, Germany) access cavity preparation was done. At this step, ISO 90 no.K-file(Dentsply Maillefer, Ballaigues, Switzerland) was placed in the canal till the working length (Figure 2)
The canal was then irrigated with 2.5% sodium hyopochlorite using a 30 gauge side vented needle to avoid its apical extrusion and walls of the canal were cleaned using a circumferential filing motion.

Fig. 3
Intracanal medication with Ca(OH)2 paste(Ultracal, Ultradent, USA) and sealing of the access cavity was done using a glass ionomer.
Three weeks later , the tooth was again isolated under rubber dam and the canals thoroughly irrigated with saline to wash out any remnants of the Ca(OH)2 dressing and 17% liquid EDTA Smear Clear(SybronEndo, CA, USA) for removal of the smear layer and the canal was then dried with paper points
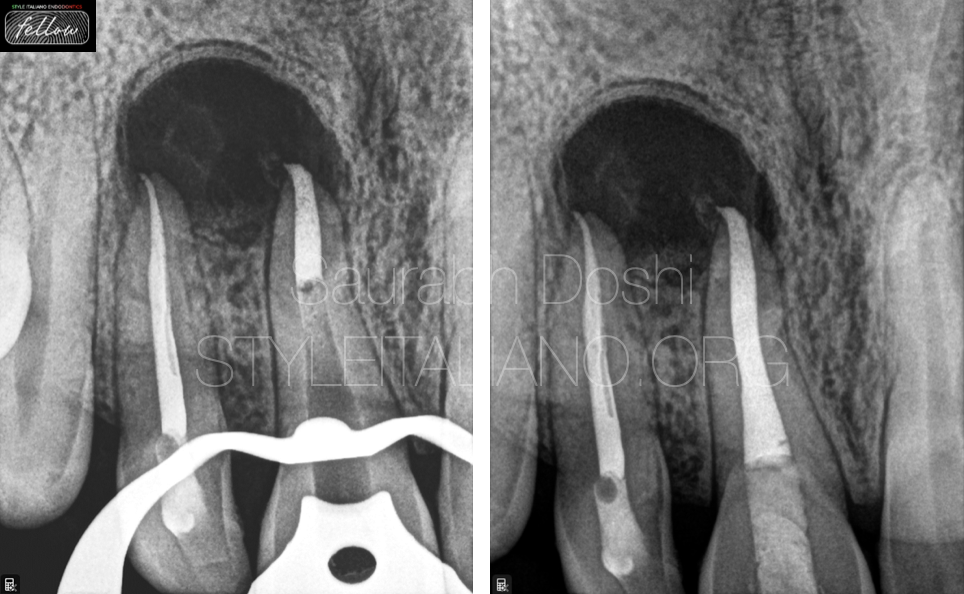
Fig. 4
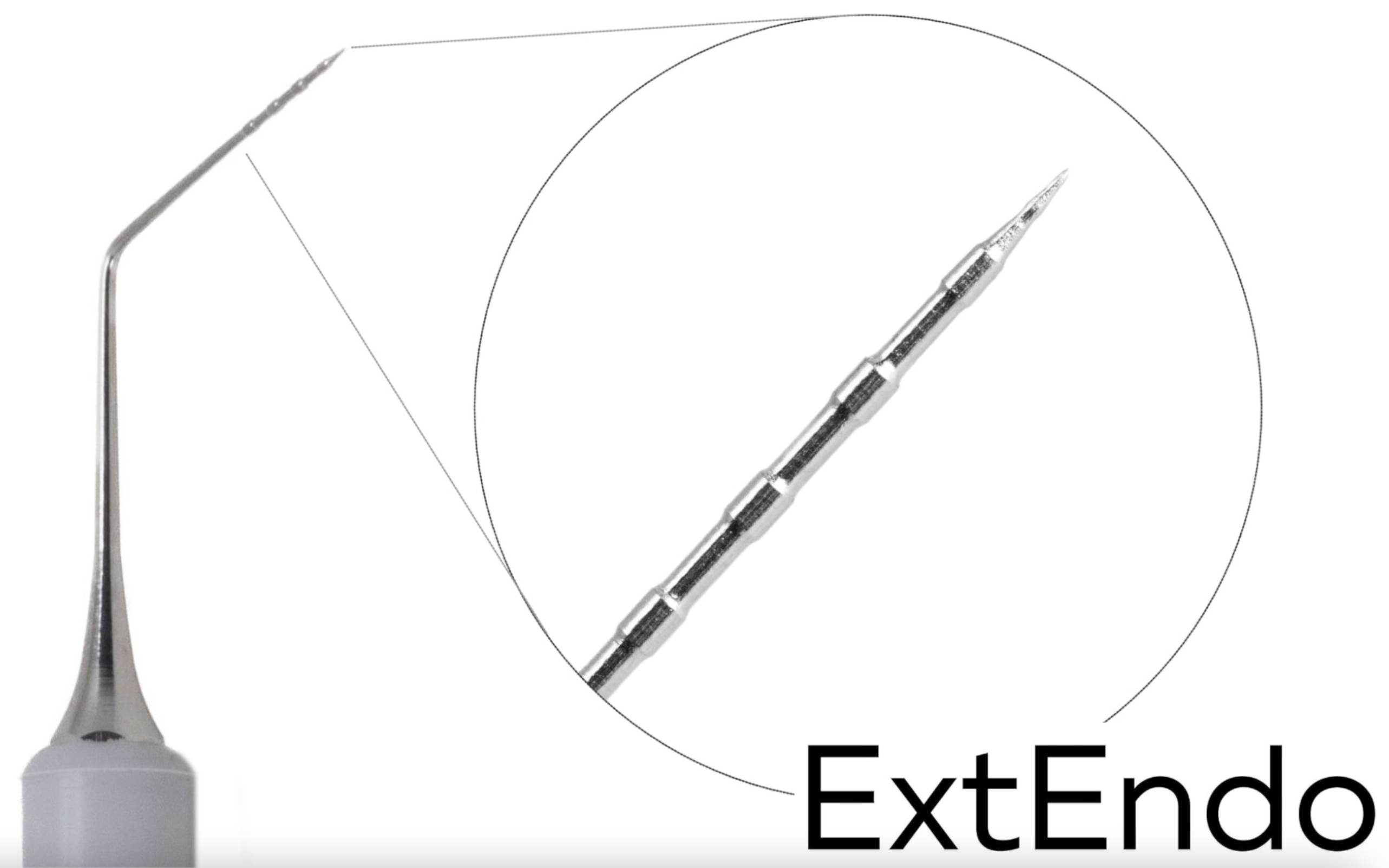
MTA carrier or Messing Gun or Dovgan carrirer used under operating microscope to place the MTA in open apex.
White MTA was then mixed with distilled water according to manufacturer’s instructions and 3-5 mm of MTA plug was subsequently placed at the apex
Butt end of a paper point was used to compact the material and clear out any excess from the walls. Subsequently, backfill was performed using Denjoy backfill gun and the access cavity was sealed using core build up material. A radiograph confirmed the completion of the endodontic therapy.
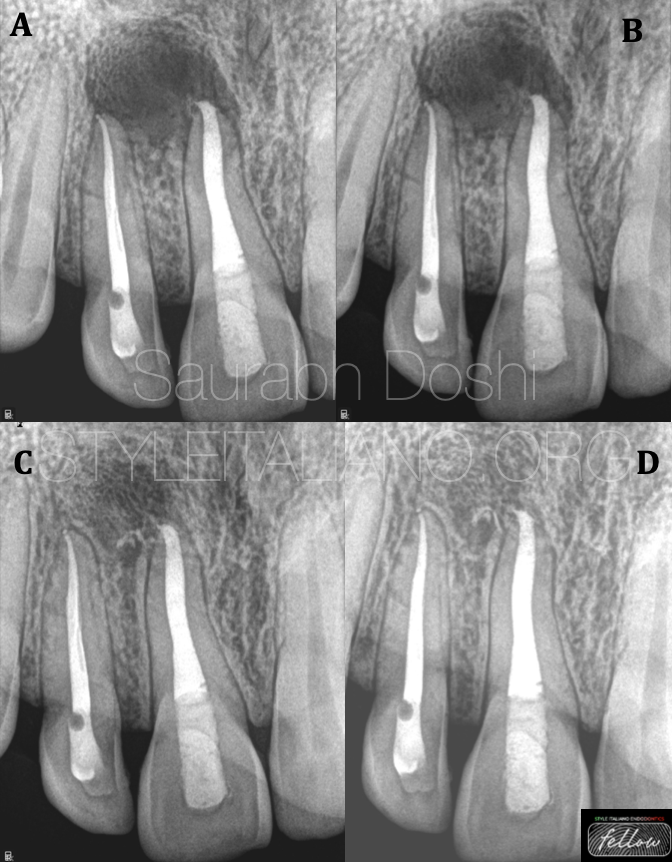
Fig. 5
Apical plug with MTA - a 30 months follow-up revealed complete healing and bone formation

Fig. 6
About the author:
Saurabh Doshi
2015: Diploma in laser dentistry (Austria)
2017: Master with honors in Endodontics from M.A. Ragoonwala Dental College and research centre, Pune, India
2021: Diplomate of Indian Board of Endodontics from prestigious India Endodontic Society
Author of book "The root canal obturation - Past, Present and Future
Speaker in various Indian Dental Association Forums
A passionate clinician, avid sportsman and doting father
Conclusions
Nonsurgical management of periapical lesions have shown a high success rate. A nonsurgical approach should always be adopted before resorting to surgery. The decompression and aspiration–irrigation techniques can be used when there is drainage of cystic fluid from the canals. These techniques act by decreasing the hydrostatic pressure within the periapical lesions. When there is no drainage of fluid from the canals, calcium hydroxide or the triple antibiotic paste can prove beneficial. Periodic follow-up examinations are essential and various assessment tools can be used to monitor the healing of periapical lesions. The surgical approach can be adopted for cases refractory to nonsurgical treatment, in obstructed or non-negotiable canals and for cases where long-term monitoring of periapical lesions is not possible.
Bibliography
1. Sjogren U., Hagglund B., Sundqvist G., Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990; 10: 498-503
2. Ingle J.Bakland L.Baugartner C. Ingle's endodontics. 6th ed. Saunders, St Louis2009