
Management of Internal Root Resorption
20/01/2017
Marino Sutedjo
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Root resorption is the loss of dental hard tissues as a result of clastic activities. There are two types of root resorption in dentistry that we know, one is physiologic and the other is pathologic. Root resorption in the primary dentition is considered a normal physiologic process except when the resorption occurs prematurely. On the other hand, pathologic resorption causes a progressive loss of tooth structure. It occurs when there is a break in the protective covering of the dentin, the cementum on the external surface, or the odontoblast layer on the internal surface, which allows clastic cells from the circulatory system access to the dentin. Unfortunately, pathologic resorption frequently is diagnosed too late for effective treatment, misdiagnosed and sometimes treated inappropriately.
There are four types of pathologic resorption in dentistry, one is internal and three external.
1. Internal resorption (IR)
2. Invasive Cervical Resorption (ICR)
3. External Inflammatory Resorption (EIR)
4. Replacement Resorption (RR)
In this article, internal root resorption only will be discussed from it’s prevalence, etiology, diagnosis to treatment perspective and followed case report.
Prevalence
Internal root resorption has been described as intraradicular or apical according to the location in which the condition is observed. Intraradicular internal resorption is an inflammatory condition that results in progressive destruction of intraradicular dentin and dentinal tubules along the middle and apical thirds of the canal walls. This condition is more frequently observed in male than female subjects. Patel el al (2010) reported that the most commonly affected teeth were maxillary incisors.
Apical internal resorption on the other hand is fairly common occurrence in teeth with periapical lesions. In the rest of this article, only intraradicular forms of internal root resorption will be discussed and and it will be simply referred to as internal resorption.
Etiology
For internal root resorption to occur, the outermost protective odontoblast layer and the predentin of the canal wall must be damaged, resulting in exposure of the underlying mineralized dentin to odontoclasts. Various etiologic factors have been proposed for the loss of predentin, including trauma, caries and periodontal infections, excessive heat generated during restorative procedures on vital teeth, calcium hydroxide procedures, vital root resections, orthodontic treatment, or simply idiopathic dystrophic changes within normal pulps. Calixskan MK, 1997 showed a study of 25 teeth with internal resorption, trauma was found to be the most common predisposing factor that was responsible for 45% of the cases examined. The other etiologies as suggested by Wedenberg, 1987 were inflammation as a result of carious lesions (25%) and carious / periodontal lesions (14%) also pulpal inflammation/infection. Those are the major contributory factors in the initiation of internal resorption. However, the advancement of internal root resorption depends on bacterial stimulation of the clastic cells involved in hard tissue resorption. Without this stimulation, the resorption will be self-limiting (Wedenberg, 1987).
Diagnosis
Among the four types of pathologic resorption, internal resorption is the most well known in the dental community although it is fairly uncommon. Internal resorption originates in a vital pulp, and the pulp must remain vital for the resorption to be progressive. Unfortunately in many cases internal resorption is found after the pulp has become necrotic and the process has arrested. Teeth with internal resorption usually are asymptomatic and often identified radiographically. Clinically, internal resorption teeth sometimes can be identified when resorption is in the coronal area and the tooth takes on a pink hue. Radiographically, internal resorption usually is round or oval-shaped and centered on the root canal, and the canal is not visible through the resorption area. Also, the defect for internal resorption is a widening of the canal.
Treatment Perspectives
In general, there are three treatment options for internal resorption
1. No treatment with eventual extraction if and when the tooth becomes symptomatic.
2. Immediate extraction.
3. Saving it by doing internal treatment that include conventional root canal treatment.
Before we decide our plans, we must make a decision first on the prognosis of the tooth. If the resorption is contained within the root with no perforation, good prognosis for treatment with conventional endodontic treatment can be achieved. If the resorption perforates the root the prognosis is reduced. If the resorption is in the cervical area of the tooth, long term predictability of the tooth needs to be considered from a structural point, especially for anterior teeth. Restorability also must not forget to consider for deciding the treatment plan and if the tooth is restorable and has a reasonable prognosis, saving it by doing root canal treatment is the choice.
In internal resorption, our purpose of doing root canal treatment is to remove any remaining vital or necrotic tissues in the systems that can sustained and stimulate the resorbing cells via their blood supply. Good access cavity preparation is important. In teeth with actively resorbing lesions, we might need to be extra careful since bleeding from the inflamed pulpal and granulation tissues can occur and might impair visibility during the initial stages of chemomechanical debridement. The use of material such as Mineral trioxide aggregate (MTA) is also suggested to repaire internal resorption successfully, especially when there is a perforation on the root.

Fig. 1
Case of tooth 22, female, 25 years, refered to our clinic due to internal root resorption case with periapical lesion. Tooth was tender to percussion. After shaping and cleaning procedure, Ca(OH)2 was placed for medication.
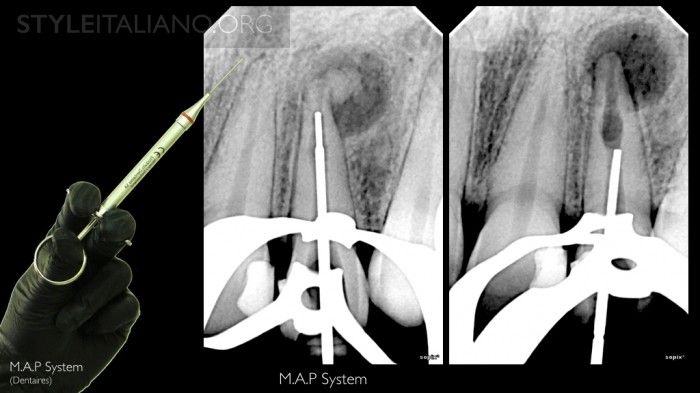
Fig. 2
MAP system was used to put MTA material for obturation.
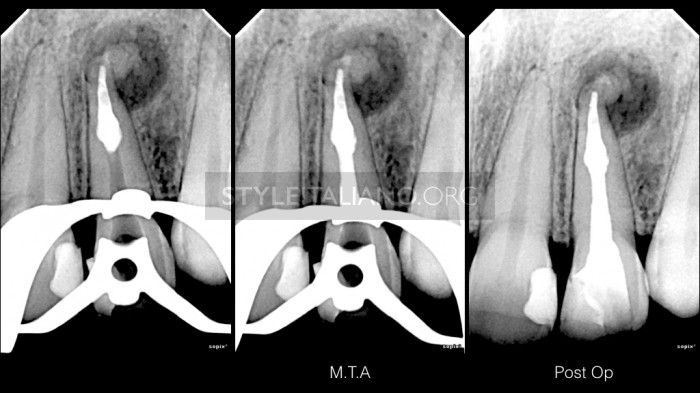
Fig. 3
MTA confirmation and post op xray

Fig. 4
Intra oral clinical images

Fig. 5
Follow up at 2 years, bone healing was evident, tooth was asymptomatic
Conclusions
Until now, root canal treatment is a good choice of treating teeth diagnosed with internal root resorption. Because the resorptive defect is the result of an inflamed pulp. Therefore, early detection is necessary for successful management of the outcome of internal resorption to prevent overweakening of the remaining root structures and root perforations since internal root resorption is often asymptomatic, and painful symptoms do not appear until an advanced stage of the lesion. CBCT in recent era no doubt has improved clinician to diagnosed internal root resorption more accurate.
Bibliography
1. Wedenberg C, Lindskog S. Evidence for A Resorption Inhibitor in Dentine. Eur J Oral ?Sci 1987; 95: 205 211
2. Wedenberg C, Zetterqvist L. Internal Resorption in Human Teeth: A Histological, ?Scanning Electron Microscopic and Enzyme Histochemical Study. J Endod 1987; ?6: 255 259
?3. Calixskan MK, Tu ?rku ?n M. Prognosis of Permanent Teeth with Internal Resorption: A Clinical Review. Endod Dent Traumatol 1997; 13: 75 81
4. Levin L, Trope M. Root Resorption. In: Hargreaves KM, Goodis HE, eds. Seltzerand Benders Dental Pulp. Chicago, IL: Quintessence Publishing Co Inc; 2002: 425 448.
5. Silveira FF, Nunes E, Soares JA, Ferreira CL, Rotstein I. Double Pink Tooth Asso?ciated with Extensive Internal Root Resorption After Orthodontic Treatment: A Case ?Report. Dent Traumatol 2009; 25: 43 47 ?
6. Patel S, Ricucci D, Durak C, Tay F. Internal Root Resorption: A Review. J Endod 2010; 36: 1107 - 1121

