Lower second molar: carrier based obturation...through the furcation
03/05/2021
Massimo Giovarruscio
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Perforations are defined as artificial communications between the root canal space and the surrounding tissues.
Endodontic perforations represent an interruption of the continuum between the endodontic space and the periradicular tissues, periodontal tissues or oral cavity.
In the presence of perforation, studies report a 10 to 12% increase in the failure rate of endodontic procedures.
The vast majority of perforations occur during access cavity preparation due to the lack of a reference point or the reduction in the size of the pulp chamber
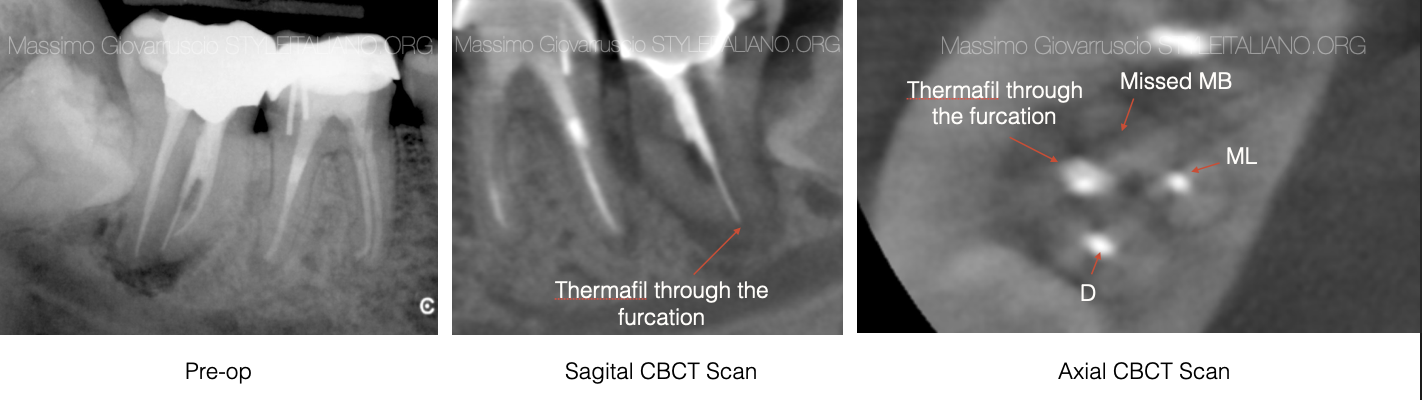
Fig. 1
Two-Dimensional images are often not useful for diagnosis. The use of CBCT at the diagnostic and treatment planning stages has significally improved clinicians’ ability to determine the perforation site and the size and the presence of associated bone loss, to plan the steps in the repair procedure.
Together with CBCT the surgical operating microscope has allowed a more precise intra-operative assessment and greater clinical precision in delivering the repair materials.
The literature has shown that MTA (Hydraulic Cement as a contemporary nomenclature) used to repair perforations yields a high success rate of 86% to 92%.

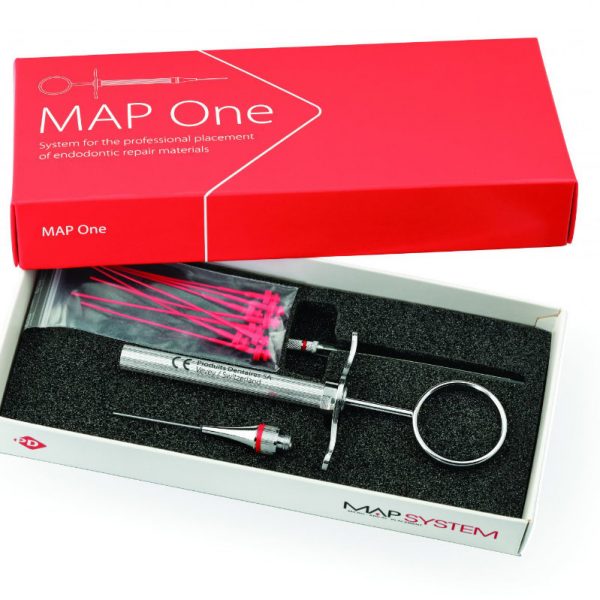
Fig. 2
Pulp chamber perforations can occur either while carrying out an access cavity or when scouting for non-obvious canal orifice. The site and size of the perforation affect the reparative approach and therefore, the overall outcome.
In the case reported, the preoperative periodical radiograph cannot show the presenze of perforation or extruded obturation material.
Only the CBCT Scan can detect the presence of obturation material not in the root canal system but in the furcation (Axial view)
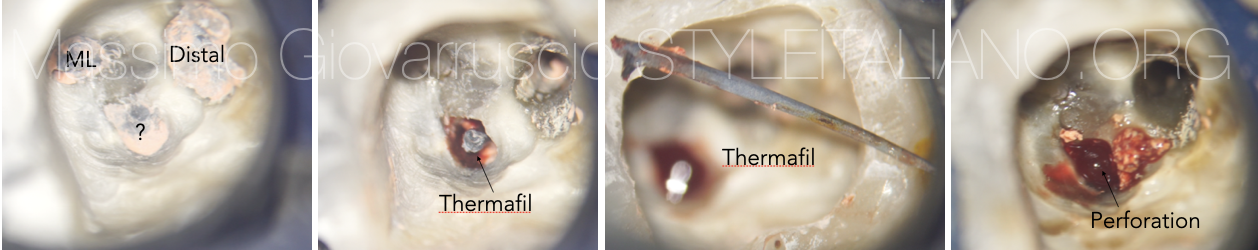
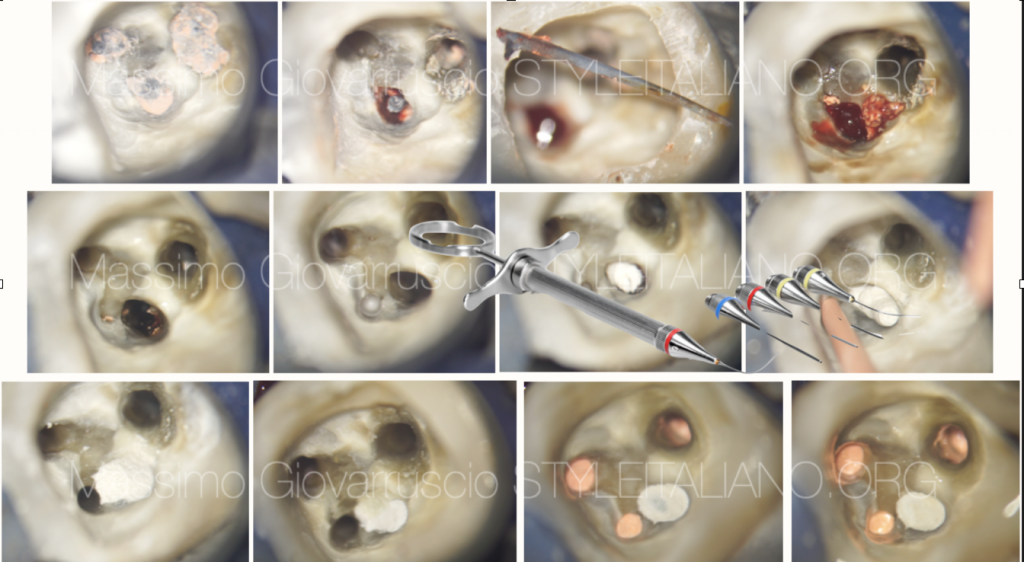
Fig. 3
Following re-access, a Thermafil carrier based was detected into the chamber perforation. The initial phase involved retrieval of the plastic carrier based which has been removed using Stieglitz forceps.
Then the gutta percha extruded material should be removed to prevent any potential foreign body reaction and delaying healing. In such cases, meticulous retrieval was carried out using a prototype micro excavator with different angulation (Dr. Morio Okaguchi, Japan).
A large bleeding can be appreciated due to the inflammatory tissues.
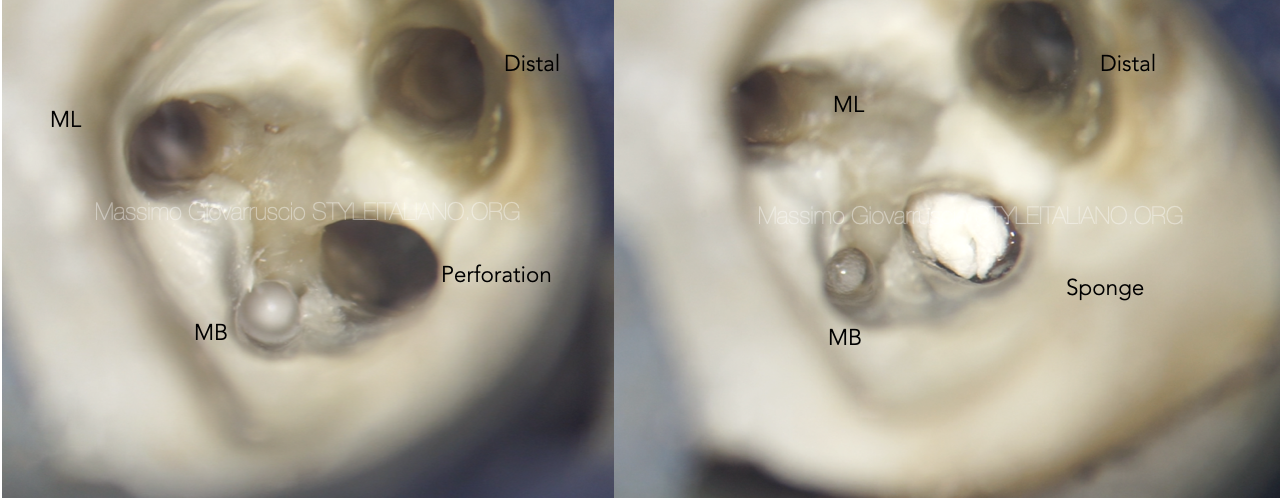
Fig. 4
Due to the large chamber perforation, a sterile resorbable collagen sponge was placed into the perforation to avoid extrusion of reparative hydraulic material.

Fig. 5
Before delivering MTA material, a gutta-percha point was placed into the MB canal as scaffolding to prevent obliterating the adjacent canal orifice. The gutta-percha cones will be retrieved prior to placement of the inter appointment dressing, once the scaffolding function is completed.
The perforation site is then repaired with a hydraulic cement delivered using a micro-apical placement (MAP) system (Produits Dentaires SA, Vevey, Switzerland)
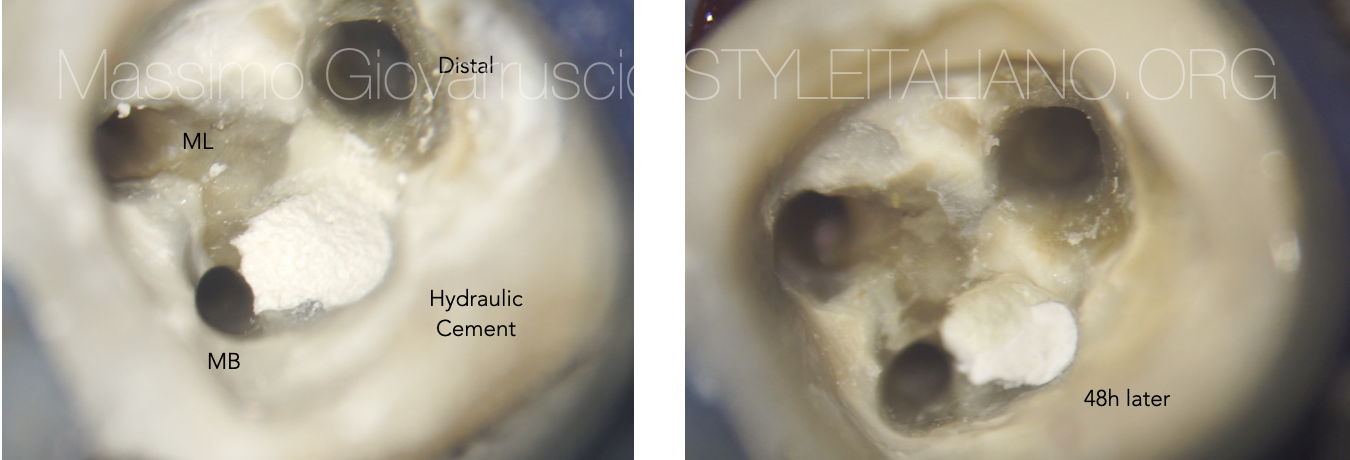
Fig. 6
When MTA is used, it is important to allow 48 hours before completing the root canal treatment to ensure full setting of the material.
When restoring teeth that have undergone repair with hydraulic cements, it is advisable to avoid the total etching technique because this can affect the properties and durability of the repair material.

Fig. 7
When applying a restoration on fresh hydraulic cements, it is advisable to apply a first layer of self-curing adhesive/GIC and then continue with the standard etch and bonding procedure and composite build-up. A self adhesive technique is indicated.
Video of the procedure

Fig. 8
Preoperative periapical radiograph showing the perforation site in the furcation area. The middle periapical radiograph showing the hydraulic cement placed on the perforation .
Postoperative radiograph showing the different materials employed in this technique with the repair material placed below the CEJ and the filling of the entire root canal system.
Conclusions
The predictability of perforation repairs has significantly improved over the last two decades, with MTA and other hydraulic cements having become the gold standard.
The techniques used for perforation repair have still not been standardised, and this is partially due to the different presentation characteristic of perforations.
In conclusion, when dealing with perforation, the main objectives are:
-To control the extrusion of soda hypochlorite through the perforation while continuing the chemical debridement
-To provide the traditional gutta-percha obturation without extruding material through the perforation site (Collagen Sponge)
-To deliver the hydraulic cement/repair material using an efficient method for precisely placing MTA
-To minimise the disruption of the bulk of hydraulic cement while completing the gutta-percha-based obturation
Bibliography
Gorni FG, Andreano A, Ambrogi F, et al. Patient and clinical characteristics associated with primary healing of iatrogenic perforation after root canal treatment: results of a long-term Italian study. J Endod. 2016;42 (2):211-215.
Giovarruscio M, Uccioli U, Malentacca A , Koller G, Foschi F, Mannocci F. A technique for placement of apical MTA plugs using modified Thermal carriers for the filling of canals with wide apices. Int Endod J 2013;46:88-97
Giovarruscio M, Tonini R, Zavattini A, Foschi F. Reparative procedures for endodontic perforations: towards a standardised approach. Endo Eat 2020;14(3):217-228