
Intentional replantation - forgotten tooth saving procedure?
13/07/2023
Ajay Bajaj
Warning: Undefined variable $post in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /home/styleendo/htdocs/styleitaliano-endodontics.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Intentional replantation or reimplantation is purposeful removal of a tooth and its reinsertion into the socket almost immediately after sealing the apical foramina.
It is a one-stage treatment that would maintain the natural tooth successfully.
Grossman calls it as one of the tooth saving procedure which is ‘the act of deliberately removing a tooth and following examination, diagnosis, endodontic manipulation, and repair—returning the tooth to its original socket to correct an apparent clinical or radiographic endodontic failure.’
Logically, when we can have someone else’s kidney, liver, heart, lungs etc, why can’t we have our own tooth back in the same place after repair on shortest possible time? Intentional replantation is considered as treatment option of the last choice when retreatment has limitations, extraction is imminent and tooth fracture while extraction is always a possibility.
Intentional replantation has history of over 1000 years and was a popular treatment option before advent of root canal procedures.

Fig. 1
A 45 year lady patient came to our clinic just 3 days before COVID lockdown with partial numbness in mandibular left jaw. She gave H/O endodontic treatment in mandibular 2nd molar 8 years ago. IOPA showed huge PA lesion associated with the tooth touching the lower border of mandible.
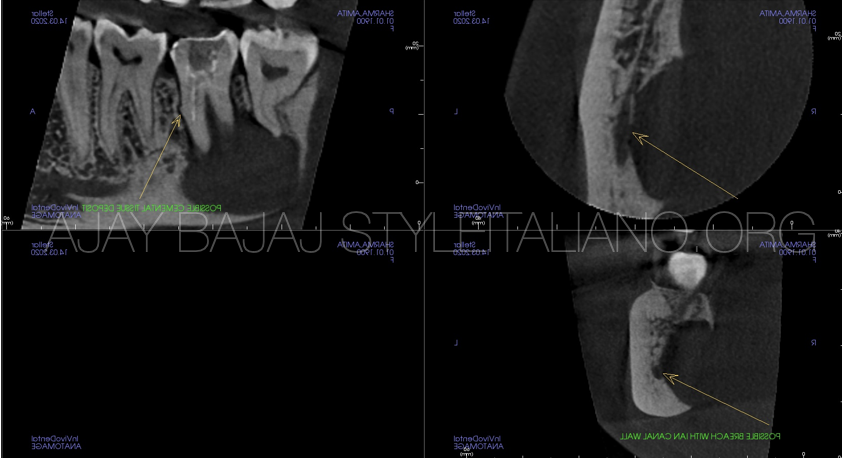
Fig. 2
Upon further CBCT examination, a large PA lesion mostly on the lingual aspect of the mandible seen involving mandibular canal and 3rd molar as well.
Video of the pre operative CBCT
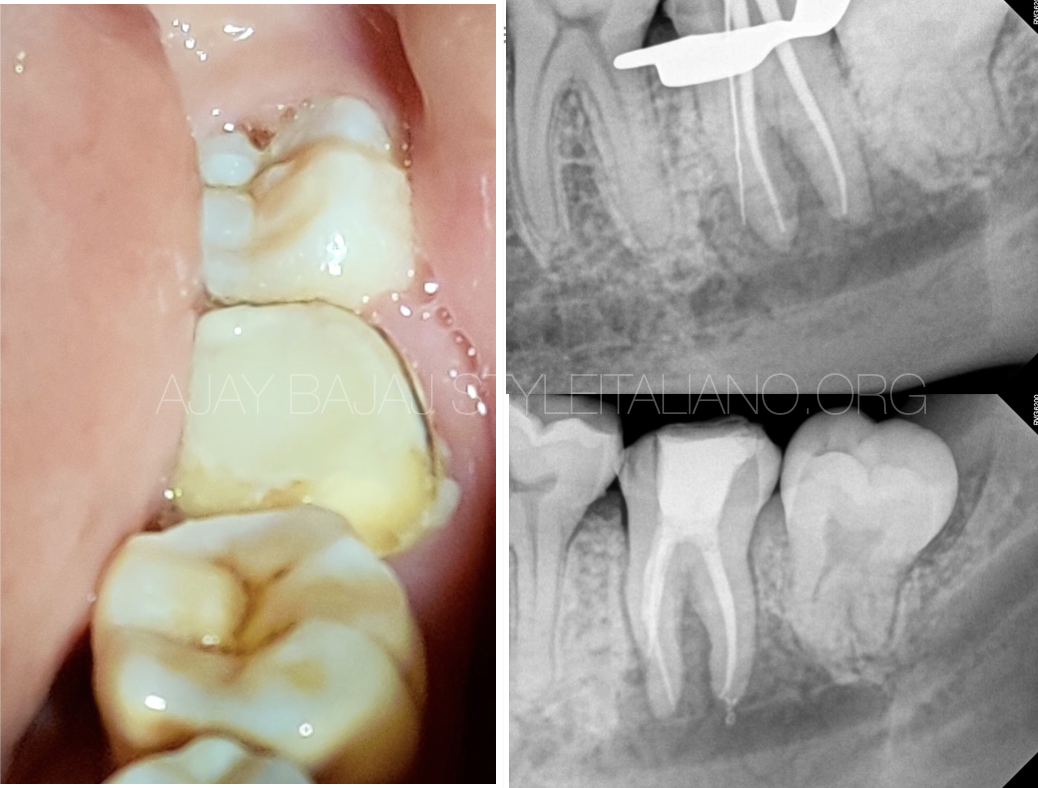
Fig. 3
Retreatment attempt also disclosed mesial ledge perforation in mesial root. Owing to complete lingual scooping of bone (inapproachable for PA surgery), mandibular canal involvement, perforation in mesial root of 2nd molar, wisdom tooth involvement and COVID lockdown, a decision to do disimpaction of 3rd molar and intentional replantation of 2nd molar was planned.

Fig. 4
Careful extraction with minimum handling of PDL is the key. There is no need to excavate PA lesion. It can lead to PDL damage. Time is an essence of the procedure. Earliest reinsertion of the tooth back in the socket ensures PDL vitality. Usually there is no need to suture or ligate most of the teeth in intentional replantation. This avoids accumulation of food particles and plaque around, and maintains physiological mobility needed to avoid ankylosis and external resorption.

Fig. 5
Immediate post op IOPA xray with Biodentine retrograde seal and 3rd molar disimpaction

Fig. 6
6 month post operative IOPA and CBCT images show excellent healing trend, with considerable closure of lingual defect. Patient reversed her numbness and gained her full normal sensation in about 2 months in lower left jaw.

Fig. 7
Pre operative and six months post operative CBCT
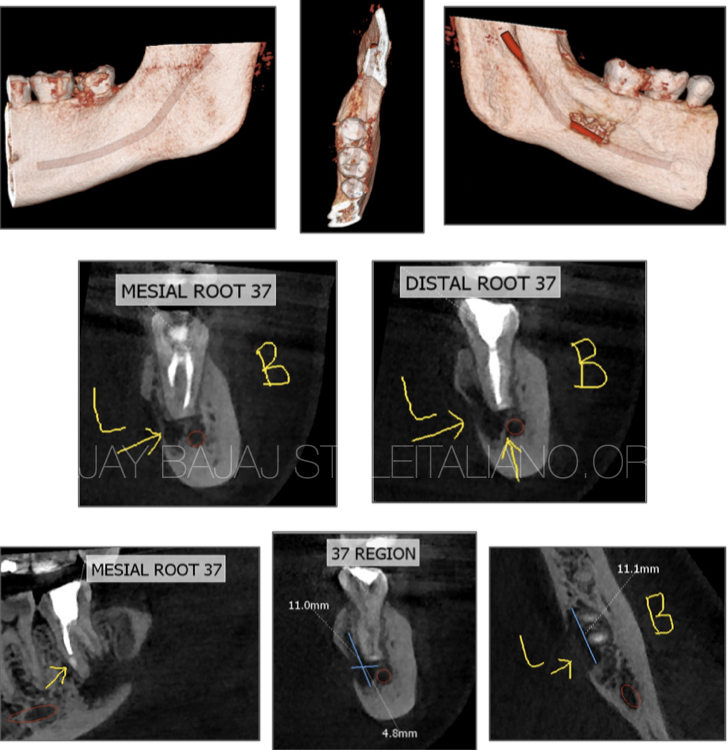
Fig. 8
6 month Post Op CBCT images
Conclusions
When orthograde routine retretment is not possible or can generate incomplete healing, and extraction cannot be avoided, one must consider intentional replantation as viable option before implants or dentures. It can be extremely satisfying treatment to the dentist as well as patient and an excellent practice building tool.
Bibliography
Grossman L I, Intentional replantation of teeth. J Am Dent Assoc. 1966: 72: 1111-1118
Niemczyk S P, Re-inventing Intentional replantation: A modification of the technique. Pract. Proced Aesthet Dent. 2001; 13 433-439
G Plotino, A Abella Sans et al. Clinical procedures and outcome of surgical extrusion, intentional replantation and tooth autotransplantation – a narrative review. Int. Endo. Journal, Dec. 2020 Vol 53, Issue 12 1636-1652

