Harmonised Multidisciplinary Endodontic treatment/Re-treatment
28/09/2023
Ahmed Alwaidh
Warning: Undefined variable $post in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
Warning: Attempt to read property "ID" on null in /var/www/vhosts/styleitaliano-endodontics.org/endodontics.styleitaliano.org/wp-content/plugins/oxygen/component-framework/components/classes/code-block.class.php(133) : eval()'d code on line 2
A 33 years old female patient been referred by a colleague to check RCT for UL6 she did a month ago with an onlay, but buccal fistula appeared and persisted even after antibiotics. History of pain about one and a half month ago, patient started the treatment at another clinic but didn’t finish there, then the patient went to the referral dentist who finished the treatment and mentioned the canals were very calcified and there was perforation in the bifurcation which she sealed with MTA.

Fig. 1
Clinically, UL6 partial onlay, with mild tenderness to buccal palpation, buccal fistula at bifurcation area, and small swelling related to MB apex. Normal probing, no evident crack.
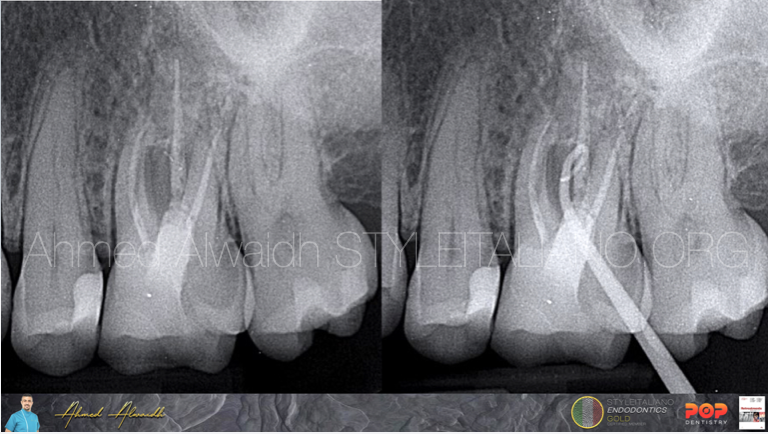
Fig. 2
IOPA revealed radiolucencies at furcation area and around all apices of UL6. Buccal sinus been traced by gutta percha to furcation area.
Fig 03:
Cone beam CT revealed big lesion communicating between MB root, furcation area and buccal plate. A missed MB2 canal was evident. Furcation perforation with no evident sealing material. There was no communication with the maxillary antrum.
Treatment plan:
After discussing the case with the patient and the treatment options with pros and cons, it was agreed on root canal re-treatment of UL6:
1- Conservative access.
2- Root canal re-treatment of the three major canals and thorough disinfection.
3- Managing to prepare the missed MB2 canal.
4- Sealing off the perforation with BC putty on a resorbable collagen sponge.
5- Filling the canals with non-setting calcium hydroxide intra-canal dressing for a week, to raise the pH, and to ensure the BC putty is set in the next visit and not been washed away.
6- Finishing the treatment by a three dimensional root filling material, and restoring UL6 to function.

Fig. 3
After access opening, the furcation perforation was evident without any evident sealing material.
Re-treatment of the three major canals been done with Open file #12/17 (Fanta Dental, Shanghai, China) and AF F-One #25/06 (Fanta Dental, Shanghai, China) to full working length, with integrated apex locator and without the use of any gutta percha solvent.
The missed MB2 been identified by tracing its location under the microscope and been trephined with US tips
Tried to negotiate the MB2 with C file #10 but it was impossible. Then MB2 was mechanically negotiated easily with the new file Harmony #17/04 (Fanta Dental, Shanghai, China) to full working length, then canal been prepared with AF F-One #25/06.
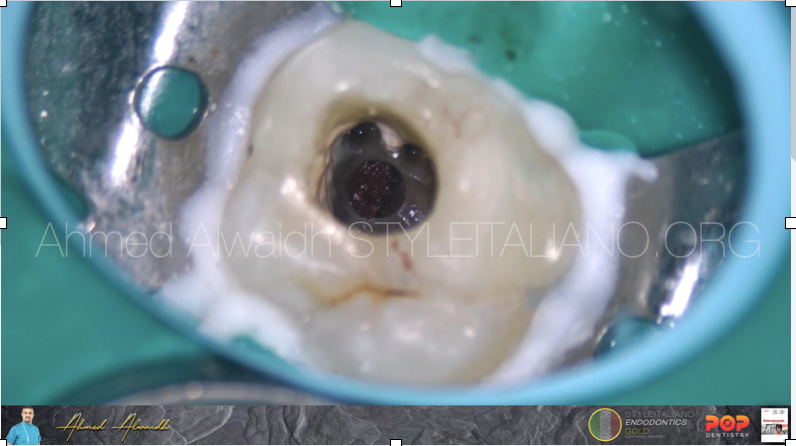
Fig. 4
After cleaning the perforation site with ultrasonic, a resorbable haemostat collagen sponge been placed to work as a platform so the sealing material can be placed on, and to cease bleeding until the sealing material is fully set.

Fig. 5
Bioceramic putty been placed on the the collagen sponge. Canals been filled with non-setting intra-canal calcium hydroxide dressing. A wet cotton pallet been placed on the BC putty to decrease setting time, and glass ionomer temporary filling, and the patient been scheduled for the next visit after 7 days.
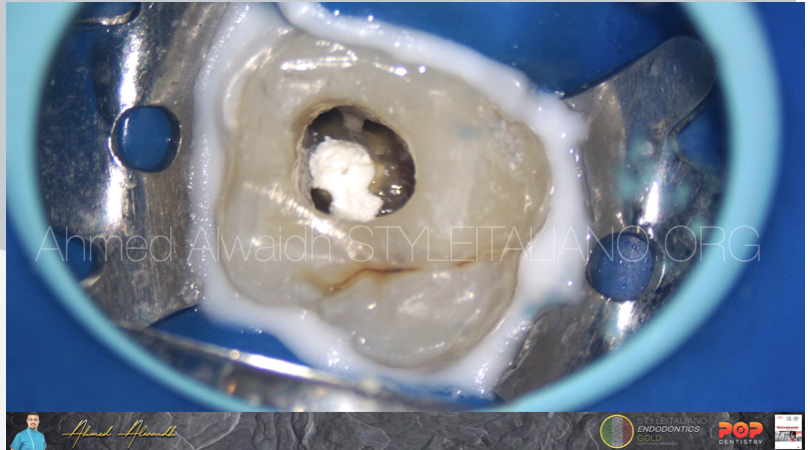
Fig. 6
After a week, patient presented with absence of symptoms and absence of buccal fistula. After removal of the temporary restoration, the BC putty was intact.
Irrigation with NaOCl 3%, EDTA 17%, PUI (passive ultrasonic irrigation)
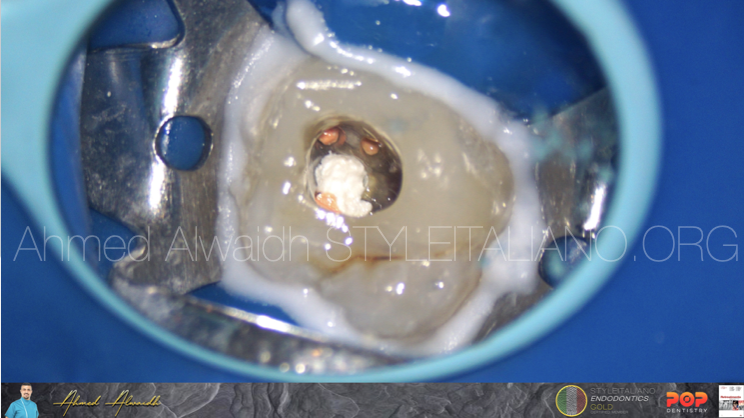
Fig. 7
Obturation of UL6 was done by hydraulic obturation with premixed bioceramic cement.
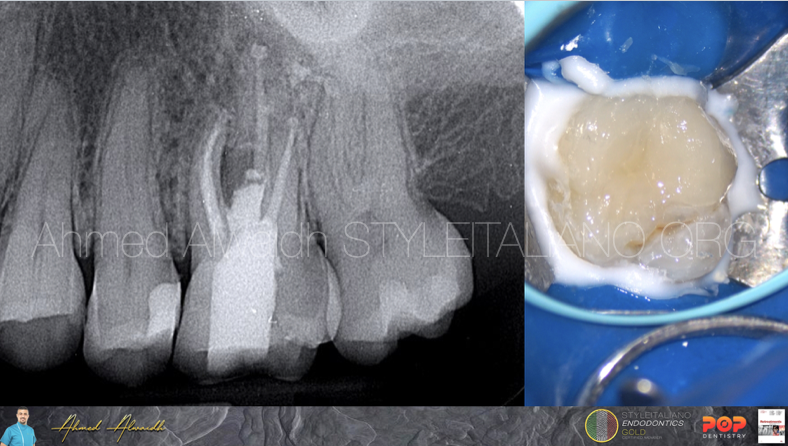
Fig. 8
The cavity then been restored with composite restoration.
Conclusions
Although MTA (mineral trioxide aggregate) exhibits great biocompatibility, excellent sealing ability, high antibacterial activity, and regenerative properties, however; MTA has some drawbacks including difficult manipulation, limited primary setting time, decreased washout due to long final setting time (Parirokh & Torabinejad 2010, Darvell & Wu 2011, Basturk et al. 2015 ). On the other hand, Bioceramic putty shows faster setting time and hydrating process compared to MTA (Guo et al. 2016) and better manipulation, which makes it more reliable in the treatment of large perforations.
Regarding mechanical negotiation of narrow and calcified canals, AF F-One #13/03 (SIE selection files, Fanta Dental, Shanghai, China) manifested great results as I mentioned before in many articles, due to the benefits of the flat-side design. In this case, I used the newly introduced Harmony file (Fanta Dental, Shanghai, China) for mechanical negotiation of extremely narrow and calcified MB2 canal, which exhibited great ability due to the unique design of variable taperness and variable cross section design.
Bibliography
Basturk F B, Nekoofar M H, Gunday M, Dummer P M (2015) Effect of varying water-to-powder ratios and ultrasonic placement on the compressive strength of mineral trioxide aggregate. Journal of endodontics 41(4), 531-534.
Darvell B W and Wu R C T (2011) “MTA” an hydraulic silicate cement: review update and setting reaction. Dental Materials 27(5), 407-422.
Guo Y J, Du T F, Li H B, Shen Y, Mobuchon C, Hieawy A, Wang Z J, Yang Y, Ma J, Haapasalo M (2016) Physical properties and hydration behavior of a fast-setting bioceramic endodontic material. BMC oral health 16, 1-6.
Parirokh M and Torabinejad M (2010) Mineral trioxide aggregate: a comprehensive literature review—part III: clinical applications, drawbacks, and mechanism of action. Journal of endodontics 36(3), 400-413.